Prospective associations between joint categories of physical activity and insomnia symptoms with onset of poor mental health in a population-based cohort
Mitch J Duncn *,Elizbth G Hollidy ,Nicol W Burton ,Nichols Glozir ,Stin Oftdl,b
a School of Medicine and Public Health;College of Health,Medicine,and Wellbeing,The University of Newcastle,Callaghan,NSW 2308,Australia
b Priority Research Centre for Physical Activity and Nutrition,The University of Newcastle,Callaghan,NSW 2308,Australia
c School of Applied Psychology,Griffith University,Brisbane,QLD 4122,Australia
d Menzies Health Institute Queensland,Griffith University,Brisbane,QLD 4122,Australia
e Brain and Mind Centre,Central Clinical School,The University of Sydney,NSW 2050,Australia
Abstract Background: Physical inactivity and insomnia symptoms are independently associated with increased risk of depression and anxiety;however,few studies jointly examine these risk factors.This study aimed to prospectively examine the joint association of physical activity (PA) and insomnia symptoms with onset of poor mental health in adults.Methods: Participants from the 2013 to 2018 annual waves of the Household Income and Labour Dynamics in Australia panel study who had good mental health (Mental Health Inventory-5 >54) in 2013,and who completed at least 1 follow-up survey (2014-2018),were included(n=10,977).Poor mental health(Mental Health Inventory-5 ≤54)was assessed annually.Baseline(2013)PA was classified as high/moderate/low,and insomnia symptoms (i.e.,trouble sleeping) were classified as no insomnia symptoms/insomnia symptoms,with 6 mutually exclusive PAinsomnia symptom groups derived.Associations of PA-insomnia symptom groups with onset of poor mental health were examined using discrete-time proportional-hazards logit-hazard models.Results: There were 2322 new cases of poor mental health (21.2%).Relative to the high PA/no insomnia symptoms group,there were higher odds (odds ratio and 95% confidence interval (95%CI)) of poor mental health among the high PA/insomnia symptoms (OR=1.87,95%CI:1.57-2.23),moderate PA/insomnia symptoms (OR=1.93,95%CI: 1.61-2.31),low PA/insomnia symptoms (OR=2.33,95%CI: 1.96-2.78),and low PA/no insomnia symptoms(OR=1.14,95%CI:1.01-1.29)groups.Any level of PA combined with insomnia symptoms was associated with increased odds of poor mental health,with the odds increasing as PA decreased.Conclusion: These findings highlight the potential benefit of interventions targeting both PA and insomnia symptoms for promoting mental health.
Keywords: Depression;Physical activity;Sleep quality
1.Introduction
Depression and anxiety are common mental health conditions affecting an estimated 4.4%and 3.6%of the global population,respectively.1Depression and anxiety increase the risk of cardiovascular disease2,3and all-cause mortality,4,5and are significant contributors to years lived with disability globally and the global burden of disease.1Consequently,there is a need for interventions targeting modifiable risk factors to reduce the onset of poor mental health.
When examined as separate risk factors,physical inactivity and insomnia symptoms are consistently associated with increased risk of depression and anxiety in prospective cohort studies.6-10However,studies that examine either physical inactivity or insomnia symptoms as separate risk factors7,11-13do not provide insight regarding how the combination of these 2 factors influence the risk of poor mental health.There is also evidence that the co-occurrence of insomnia symptoms and shorter sleep duration (e.g.,<7 h) is associated with a greater likelihood of chronic mental health symptoms relative to the presence of either insomnia symptoms or shorter sleep duration alone.14Physical inactivity and poor sleep frequently cooccur and demonstrate a bidirectional relationship.15-18People with depressive symptoms more frequently report inactivity and insomnia symptoms than do people without depressive symptoms,19-21and insomnia symptoms (e.g.,difficulty falling asleep or staying asleep)are both a risk factor for and a symptom of depression.22Increasing physical activity (PA)can improve sleep quality in a variety of populations.23Furthermore,physical inactivity and insomnia symptoms may influence mental health through common mechanistic pathways,such as oxidative stress and inflammation,hormone regulation (i.e.,dopamine and serotonin),and psychological factors(i.e.,worry,low self-esteem).24
Cross-sectional studies have shown that adults with low levels of PA in combination with short sleep duration and poor sleep quality have poorer self-rated health and higher mental distress than those adults with more favorable patterns of activity and sleep.15,18Understanding how both factors are potentially associated with the onset of poor mental health could inform multicomponent interventions,which may be an effective use of participants’ time and health promotion resources.Therefore,the aim of the current study was to examine the prospective relationship between combinations of PA and insomnia symptoms and the onset of poor mental health in a population-based cohort of Australian adults.The prospective relationship between combinations of PA and sleep disturbance,defined as the co-occurrence of insomnia symptoms and short sleep duration,and the onset of poor mental health was also examined.
2.Methods
2.1. Study design
The study included data from 5 annual waves(2013-2018)of the Household Income and Labour Dynamics in Australia(HILDA) study,which is described in detail elsewhere.25,26The HILDA study began with a large national probability sample of Australian households occupying private dwellings in 2001 and has surveyed participants annually since then.Briefly,households were selected using a multi-staged approach.First,a sample of collection districts (a census administrative area each containing 200-250 households)were selected from across Australia;second,dwelling units within each collection district were randomly selected,followed by the selection of households.25,26All household members(≥15 years of age)who provided at least 1 interview in Wave 1 formed the basis of the panel to be pursued in each subsequent wave,and the sample has been gradually extended to include any new household members whose addition resulted from changes in the composition of the original households.
Participant assessment consists of face-to-face interviews as well as self-completion questionnaires.The HILDA project was initiated and is funded by the Australian Government’s Department of Social Services and is managed by the Melbourne Institute of Applied Economic and Social Research.All procedures involving human participants were approved by the Human Ethics Research Committee of The University of Melbourne (ID: 1647030).Written informed consent was obtained from all participants.In 2013,2014,2015,2016,2017,and 2018,the total number of interviews completed and the in-scope response rates were 17,500(67.4%),17,511 (66.5%),17,605 (65.6%),17,693 (64.6%),17,570(63.7%),and 17,434(62.0%),respectively.26Summary information on variables is provided as follows,with details on the items used to assess the outcome,exposure variables and confounders,their response options,and subsequent classification provided in Supplementary Table 1.
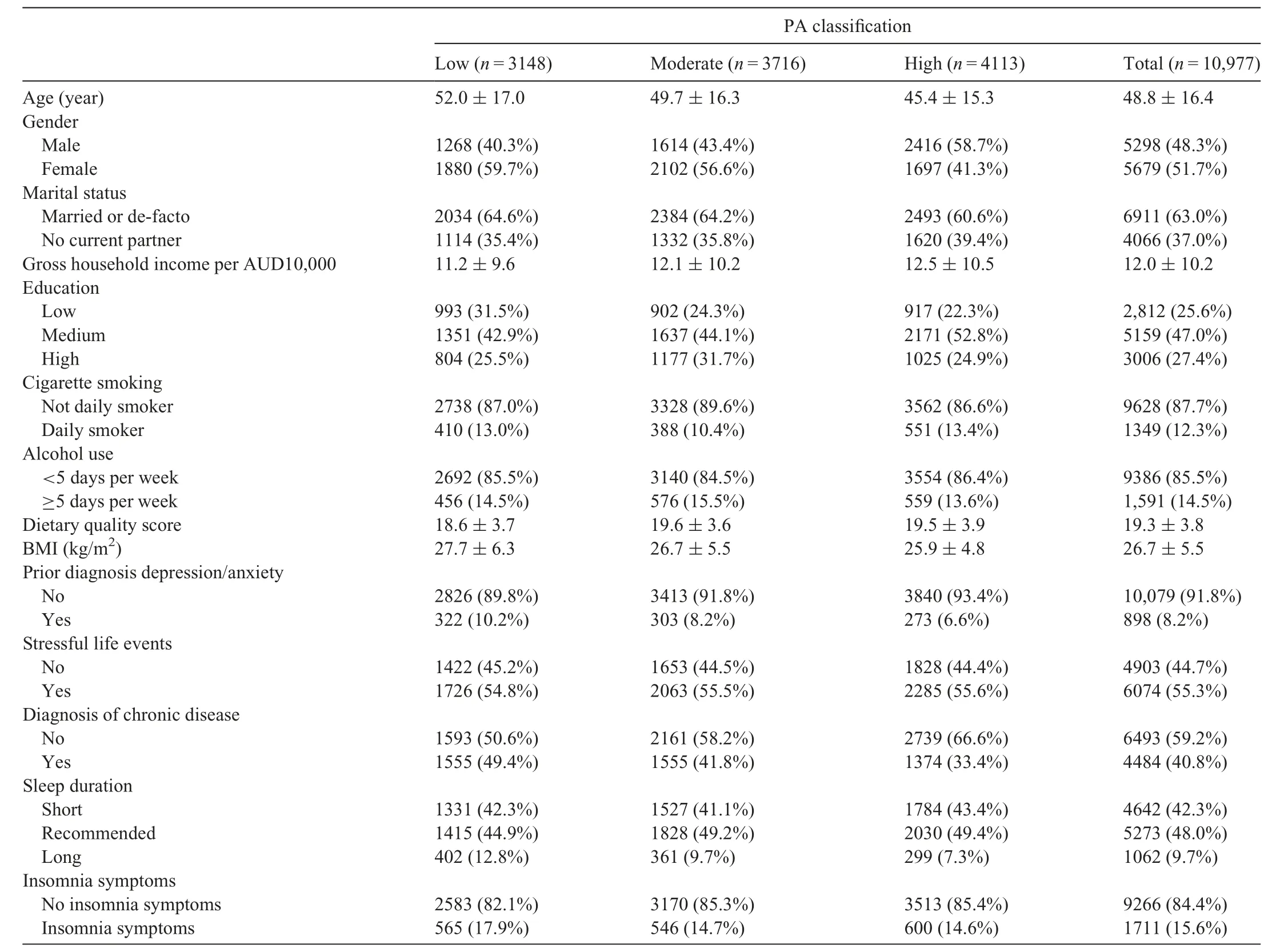
Table 1 Participant characteristics in 2013 by PA classification(n=10,977).
2.2. Outcome
Mental health was assessed using the Mental Health Inventory-5 (MHI-5),a 5-item screening tool for depression and anxiety derived from the 36-Item Short Form Health Survey.27Each item uses a 6-point Likert scale to report the frequency of symptoms,ranging from “none of the time” to “all of the time”.Responses to the 5 items are summed,and the raw scores range from 5 to 35 and are standardized to create a scale ranging from 0 to 100,where higher scores indicate better mental health.27The instrument has demonstrated good internal consistency (Cronbach’s α=0.83),and a cut-point of≤54 has shown moderate sensitivity (63%) and high specificity (96%) for identifying diagnosed depression.27Based on this previously identified optimum cut-point,participants were classified as having poor mental health(MHI-5 ≤54)or good mental health(MHI-5 >54)at each wave.
2.3. Exposures
The 2013 survey wave provided data on PA and insomnia symptoms.PA during the previous week was assessed using the International Physical Activity Questionnaire Short Form(IPAQ-SF).28Items assess the frequency and duration of walking,moderate,and vigorous intensity PA over the previous week.The total metabolic equivalent(MET)minutes(MET-min) of walking,moderate,and vigorous intensity PA and total PA were calculated according to standard IPAQ scoring protocols using MET values of 3.3 for walking,4.0 for moderate intensity PA,and 8.0 for vigorous intensity PA.28,29Participants’ total MET-min of PA were subsequently classified as low PA,moderate PA,or high PA using standard IPAQ scoring protocols.28The IPAQ assesses PA in multiple domains (i.e.,occupation,recreation,household,and transport),therefore the high PA category(≥3 days of vigorous PA accumulating a total of ≥1500 MET-min/week or ≥7 days of any activity intensity and accumulating a total of ≥3000 MET-min/week) can be considered a useful target for health enhancing PA at the population level when multiple domains are assessed.30
Participants reported the frequency over the last month that they had trouble sleeping because they (a) could not get to sleep within 30 min,and/or (b) woke up in the middle of the night or early morning.Participants reporting sleep difficulties at least 3 nights per week were classified as having“difficulty initiating or maintaining sleep”,consistent withDiagnostic and Statistical Manual of Mental Disorders,5th edition,criteria for insomnia.14,31A separate item asked participants to rate their sleep quality on a 4-point scale,which was subsequently classified as“poor”(very bad or fairly bad)or“good”(fairly good or very good).A dichotomous indicator of insomnia symptoms was created based on participants reporting both difficulty initiating or maintaining sleep and poor subjective sleep quality (insomnia symptoms) or not (no symptoms).14,31-34Using these 2 exposure measures,participants were classified into 1 of 6 unique combinations of PA and insomnia symptoms:high PA and no insomnia symptoms,high PA and insomnia symptoms,moderate PA and no insomnia symptoms,moderate PA and insomnia symptoms,low PA and no insomnia symptoms,as well as low PA and insomnia symptoms.
Consistent with the aims of the study,a dichotomous indicator of sleep disturbance was created based on participants reporting both short sleep duration (<7 h/night,see baseline covariates) and insomnia symptoms (sleep disturbance) or reporting only one or neither of these (no sleep disturbance).14,34Participants were subsequently classified into 1 of 6 unique combinations of PA and sleep disturbance: high PA and no disturbance,high PA and sleep disturbance,moderate PA and no disturbance,moderate PA and sleep disturbance,low PA and no disturbance,as well as low PA and sleep disturbance.
2.4. Baseline covariates(2013)
In the 2013 survey wave,participants self-reported a range of sociodemographic,lifestyle,and psychosocial characteristics.Participants reported age (year),sex (male/female),marital status(married or de facto/no current partner),level of education (categorized as low (i.e.,did not complete high school),medium (i.e.,completed high school,advanced diploma),high (i.e.,university degree)),and gross annual household income.Income was calculated as the product of positive minus negative gross regular household income in the last financial year.Reported employment status and work arrangement were combined to create a single indicator of employment: daytime work (full time or part time);retired/home duties/non-working student/other;night-time work(permanent,rotating,irregular);and unemployed.
Participants reported whether or not they had ever received a diagnosis of arthritis or osteoporosis,asthma,cancer,chronic bronchitis or emphysema,Type 1 diabetes,Type 2 diabetes,heart disease,hypertension,or any other serious circulatory condition(e.g.,stroke).A binary indicator of chronic condition(present/not present) was created if participants self-reported the presence of any of these conditions.Participants also reported whether they had ever received a diagnosis of depression or anxiety,which was classified as a dichotomous variable(history/no history).Self-reported height and weight were used to create body mass index.
Cigarette smoking status was assessed using a single item and grouped into 1 of 3 categories (never smoked/previous smoker/current smoker).34The frequency of alcohol consumption was used to classify participants into 1 of 2 categories(<5 days/week or ≥5 days/week).32,34Sleep duration (h/day)included daytime naps and was self-reported;it was used to classify sleep duration in terms of age specific criteria from the National Sleep Health Foundation.35Participants>65 years of age who reported getting 7-9 h of sleep per night,and those aged ≥65 years who reported getting 7-8 h of sleep per night,were classified as“recommended”.35Those who reported fewer than 7 h of sleep were classified as “short sleep”,and those who reported >8 h and were ≥65 years of age or who reported >9 h and were <65 years of age were considered to have“long sleep”.35
A diet quality score was calculated based on frequency of consumption of foods from recommended food groups (9 items),discretionary foods (5 items),fruit and vegetable serves (2 items),salt added to food (1 item),meals purchased from a food outlet (1 item),and the main type of milk consumed (1 item).32,34The total score ranged from 0 to 31 points,where a higher score indicated better dietary quality(see Supplementary Table 2 for scoring).The HILDA survey assesses the occurrence of 21 major life events in the 12 months preceding the survey.The univariate association between poor mental health (MHI-5) and each life event and the association between joint PA and insomnia exposure and each life event were examined used a series of χ2tests.Only those 14 life events that were associated with both the outcome and the exposure(p<0.250)were included in the overall life event scale(data not shown).32
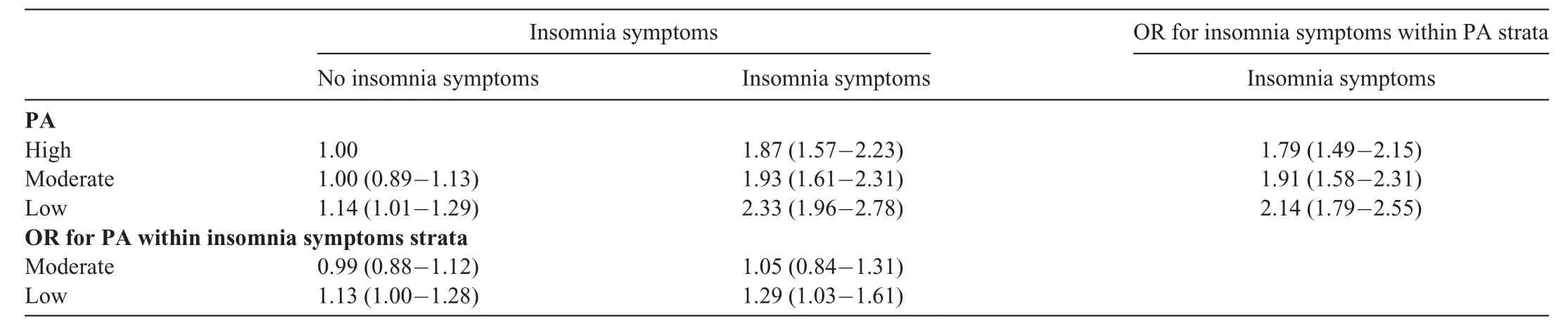
Table 2 Adjusted associations of PA classification and insomnia symptoms with onset of poor mental health(n=10,977).
2.5. Analysis
Participants were included in the current study if in 2013 they were aged 18 years or older,had complete data on covariates and exposure variables,did not report current symptoms of poor mental health based on the MHI-5(MHI-5 >54),and also provided data on mental health in at the least one of the subsequent 2014-2018 surveys.Participant sociodemographic characteristics across PA classifications and also across the joint categories of PA and insomnia symptoms are made using descriptive statistics.Comparison of participants whose data were included and excluded from the analysis in terms of sociodemographic characteristics,PA,and insomnia were conducted using χ2tests andttests.A discrete-time proportional-hazards model was estimated using a logit-hazard (i.e.,logistic)regression model to examine the association between joint categories of PA and insomnia symptoms and onset of mood disorder (yes/no) for each survey between 2014-2018.36This analysis used a person-survey year dataset with each survey year represented as a separate observation until the onset of mood disorder.Participants who were lost to follow-up were right-censored at the time of their last available survey.
Three separate models were fitted to examine associations between PA,insomnia symptoms,and the onset of mood disorder.Model 1 was an unadjusted model that included only the joint categories of PA and insomnia symptoms.Model 2 additionally estimated the potential confounding variables of sex,age,marital status,income,education,employment,smoking,alcohol,dietary quality score,body mass index,sleep duration,and chronic disease.Model 3 included all Model 2 covariates as well as previous/current diagnosis of depression/anxiety prior to 2013 and stressful life events.Wald tests were used to estimate linear trends across the joint categories of PA and insomnia symptoms and were estimated using the Stata“contrast”command.Residual diagnostics and the Stata “linktest” command were used to assess model fit and identify model specification errors.The multiplicative(e.g.,PA×insomnia symptoms) and additive interactions of the 2 exposures were estimated,and their 95% confidence intervals (95%CIs) were estimated using the delta method.The additive interactions estimated were the Relative Excess Risk due to the Interaction (RERI),the Attributable Portion due to the interaction,and the Synergy Index.To assist with the interpretation of any interaction effects,the association of PA with poor mental health within strata of insomnia symptoms was examined (reference category: high PA),as was the association of insomnia symptoms with poor mental health within strata of PA(reference category:no symptoms).37,38To address the second aim of the study,the same series of models was also used to examine associations between PA,sleep disturbance,and the onset of mood disorder;these models omitted the sleep duration variable as a confounder.Associations were expressed as odds ratios with 95%CI andpvalue.Statistical significance was set at 0.05 for all analyses,and the analyses were conducted May 2020 to August 2021,using Stata MP(Version 17;StataCorp.,College Station,TX,USA).
3.Results
Fig.1 provides a summary of the number of participants who were eligible,included in analyses,and excluded.There were 13,046 adults aged >18 years who were classified as having good mental health in 2013.Of these participants,2069 were excluded due to missing or incomplete data on confounders or exposures (Fig.1),with 10,977 participants included in the analytic sample.Included participants were older,and a higher proportion of them were married/de facto,had a high education level,were non-smokers,reported a chronic disease,had recommended sleep duration,and reported no insomnia symptoms when compared with those participants who were excluded(Supplementary Table 3).The sociodemographic,behavioral,and health characteristics of participants overall and by PA classification are shown in Table 1.The average age of participants was 48.8 ±16.4 years (mean ± SD),52% were women,and 47% had medium levels of education.Most participants were classified as either high PA and no insomnia symptoms(32%),moderate PA and no insomnia symptoms (29%),or low PA and no insomnia symptoms(24%),with approximately 5%of participants classified in each of the high PA and insomnia symptoms,moderate PA and insomnia symptoms,and low PA and insomnia symptoms groups (Supplementary Table 4).Within each PA and insomnia group for a given activity level,there was a higher proportion of participants without insomnia symptoms who were male,had a high education level,were not daily smokers,did not report prior diagnosis of depression/anxiety,reported a chronic disease,and had recommended sleep duration when compared with those participants who had insomnia symptoms (Supplementary Table 4).Rates of loss to follow-up by PA and insomnia group are shown in Supplementary Table 5.Across PA groups,loss to follow-up rates were 34%-38% when insomnia symptoms were absent and higher among groups when insomnia symptoms were present(44%-50%).
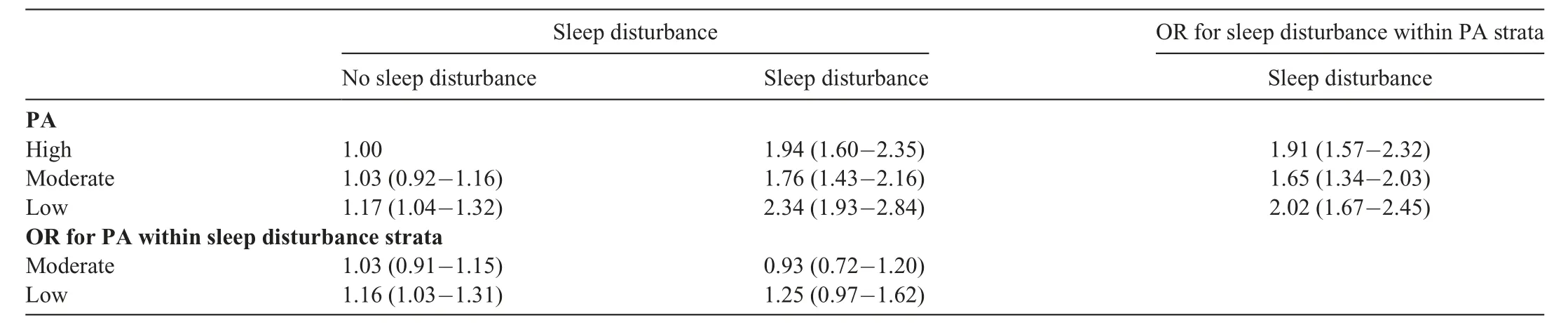
Table 3 Adjusted associations of PA classification and sleep disturbance with onset of poor mental health(n=10,977).
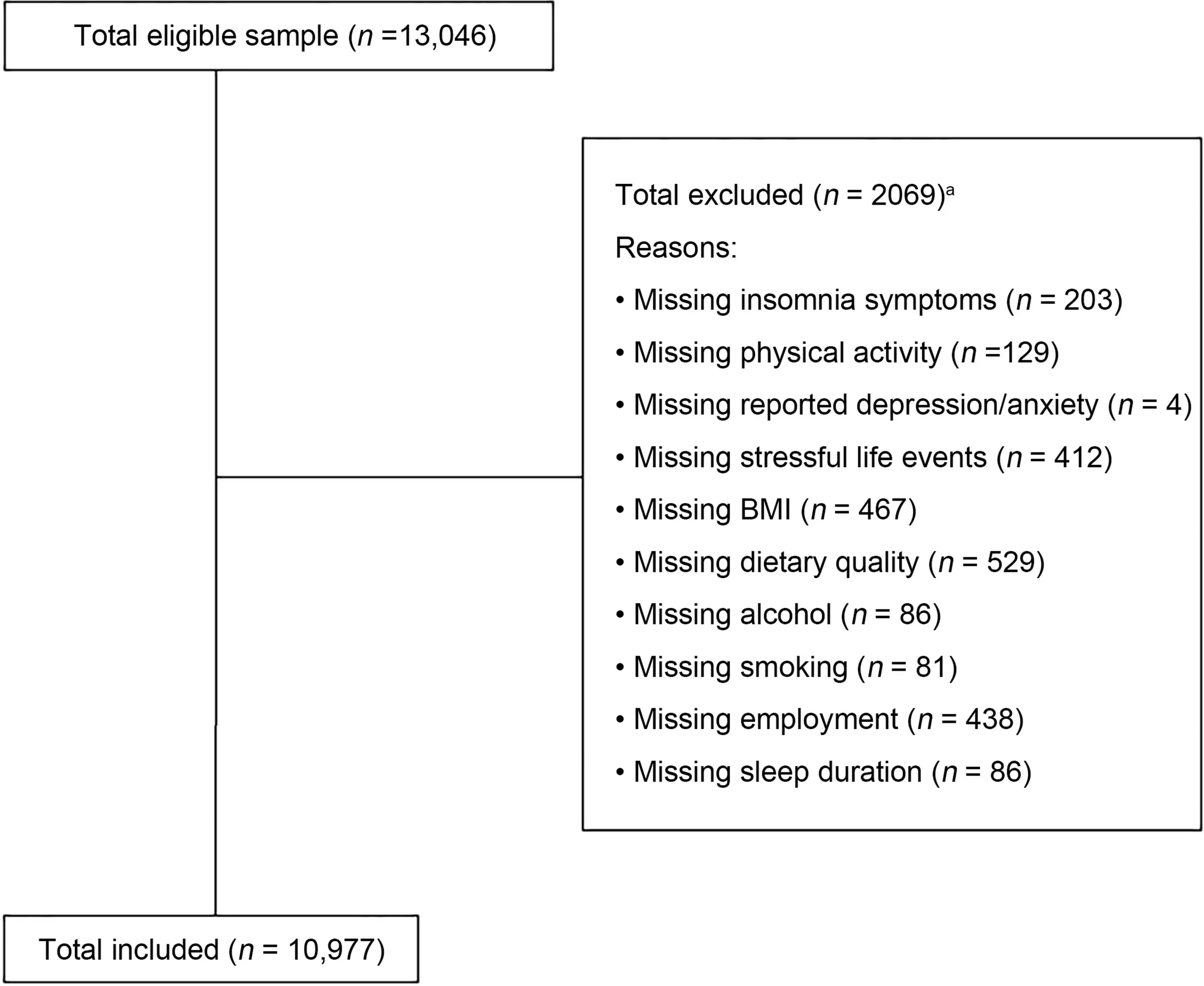
Fig.1.Participant flow chart and reasons for exclusion.a Participants could be excluded for more than 1 missing variable.BMI=body mass index.
The incidence of poor mental health between 2014 and 2018 was 21.2% (n=2322) (Supplementary Tables 6 and 7).The residual diagnostics and the link test revealed no noticeable violations of model assumptions.The associations between joint categories of PA and insomnia symptoms and the onset of poor mental health (MHI-5 ≤54) are shown in Table 2.Model 3 results are presented in text,as the pattern of associations was consistent in each of the 3 models (Model 1,Model 2,and Model 3),although the magnitude of associations was attenuated with the adjustment of additional confounders(Table 2;Supplementary Tables 8 and 9).Following adjustment for confounders and relative to participants with high PA and no insomnia symptoms,reporting either high PA and insomnia (OR=1.87,95%CI: 1.57-2.23),moderate PA and insomnia (OR=1.93,95%CI: 1.61-2.31),or low PA and insomnia(OR=2.33,95%CI:1.96-2.78)was associated with increased odds of poor mental health (Table 2;Fig.2).In combination with insomnia,the odds of poor mental healthincreased as PA levels decreased(Table 2;Fig.2).Relative to participants with high PA and no insomnia symptoms,reporting moderate PA and no insomnia was not associated with poor mental health (OR=1.00,95%CI: 0.89-1.13),but reporting low PA and no insomnia (OR=1.14,95%CI:1.01-1.29) was associated with increased odds of poor mental health.Within each stratum of insomnia symptoms,relative to high PA,low PA categories were associated with increased odds of poor mental health (Table 2).Within each stratum of PA,relative to no insomnia,insomnia symptoms were associated with increased odds of poor mental health (Table 2).The multiplicative and additive interactions indicated that the combination of insomnia symptoms with either moderate PA (OR=1.03,95%CI: 0.81-1.32;RERI=0.06,95%CI: -0.37 to 0.48) or low PA (OR=1.09,95%CI: 0.86-1.39;RERI=0.32,95%CI: -0.14 to 0.77) increased the odds of poor mental health more than either the product or the sum of these 2 exposures separately,although none of these interactions were statistically significant (Table 2).
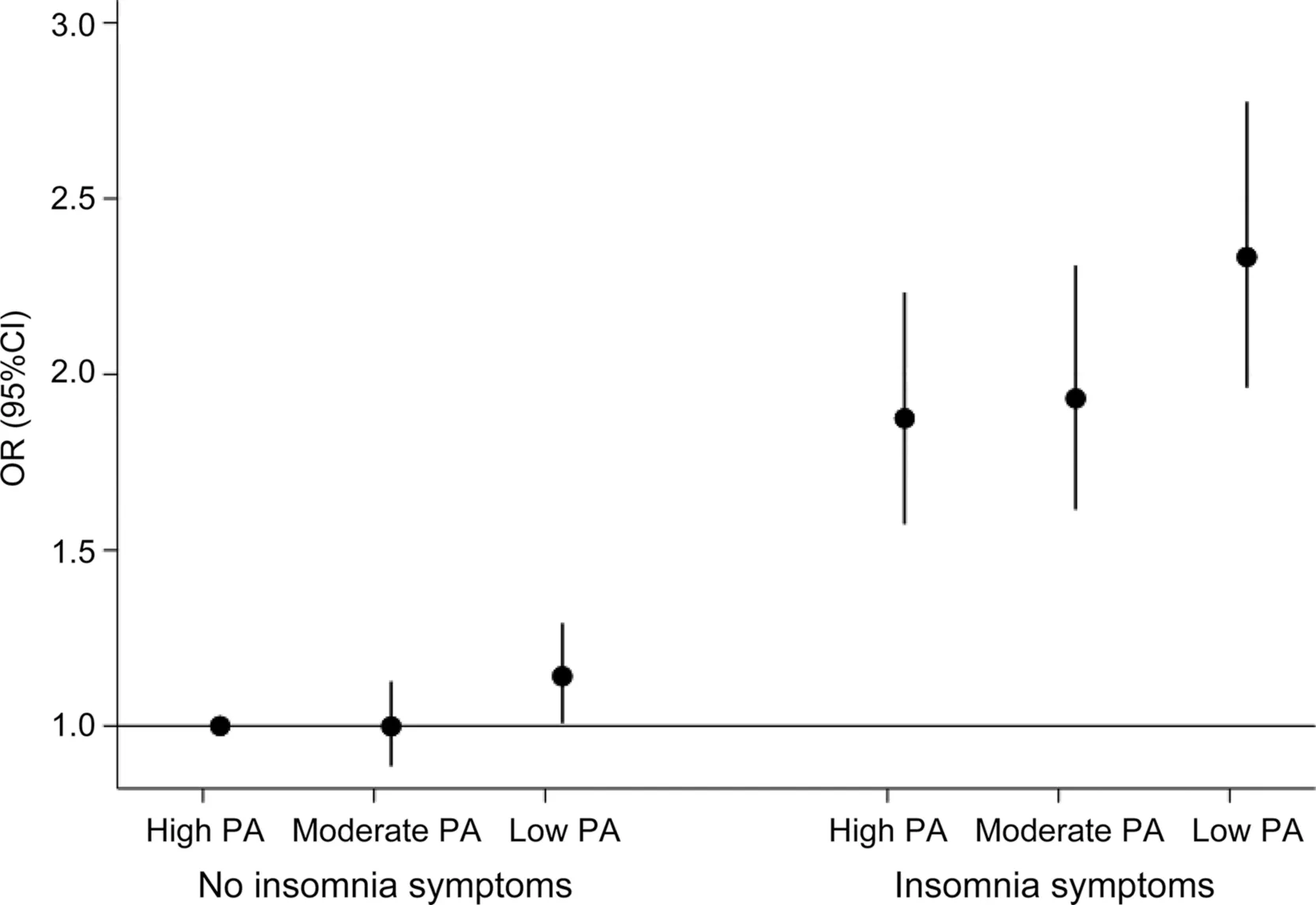
Fig.2.Adjusted associations of PA classification and insomnia symptoms with onset of poor mental health.Estimates based on Model 3.Adjusted for sex,age,marital status,income,education,employment,smoking,alcohol,dietary quality score,BMI,chronic disease,previous/current diagnosis of depression/anxiety (in 2013),stressful life events,and sleep duration.p value for trend ≤0.001.95%CI=95%confidence interval;BMI=body mass index;OR=odds ratio;PA=physical activity.
Examining the joint association of PA and sleep disturbance with the onset of poor mental health revealed a similar pattern and magnitude of associations to that observed for the joint association between PA and insomnia (Table 3;Supplementary Tables 10 and 11;Supplementary Fig.1).Although the odds of onset of poor mental health was significantly increased among participants with moderate PA and sleep disturbance(OR=1.76,95%CI: 1.43-2.16).In addition,the additive interactions for the combination of moderate PA and sleep disturbance (RERI=-0.21,95%CI: -0.70 to 0.27) indicated that the association of this combination with the onset of poor mental health was less than the sum of these 2 separate exposures(Table 3).
4.Discussion
The aim of this study was to examine the association between joint categories of PA and insomnia symptoms and the onset of poor mental health in a population-representative sample of adults over a 5-year period.Among adults with insomnia symptoms,the odds of developing poor mental health increased as PA levels decreased.When insomnia symptoms were absent,only adults with the lowest level of PA had increased odds of developing poor mental health relative to adults with the highest level of PA and no insomnia symptoms.A similar pattern of associations was observed when examining joint categories of PA and sleep disturbance,although the dose-response relationship between PA levels and poor mental health was not observed among adults with sleep disturbance.
Meta-analyses demonstrate that both lower levels of PA and the presence of insomnia symptoms are independently prospectively associated with increased risk of depression.7,9,10Similar associations are also observed for anxiety.8The findings of the current study extend this evidence in 3 ways.These results demonstrate that in the absence of insomnia symptoms,only low levels of PA were associated with increased odds of developing poor mental health.Approximately 24% of participants were in this group,and given the low levels of PA observed,this group is likely to benefit from interventions to increase PA levels.Increases in PA have been shown previously to improve sleep quality,physical health outcomes,and symptoms of depression and anxiety.12,23,39-41Current results also indicated that when insomnia symptoms were present,the odds of poor mental health progressively increased as PA levels decreased.This pattern is consistent with epidemiological and intervention evidence for the beneficial effect of PA on depression and anxiety.7,8,12,39,40Furthermore,for any given PA level,the presence of insomnia symptoms markedly increased the odds(OR:1.8-2.3) of onset of poor mental health relative to the absence of insomnia symptoms.These associations are of a lower magnitude than those observed in meta-analyses comparing the presence/absence of insomnia with risk of depression(OR:2.3-2.8).9,10This may potentially be because few studies(e.g.,3/34 studies in the review by Li et al.9)in these meta-analyses accounted for PA as a confounder,which may have upwardly biased the associations.42-44The interaction analyses of the current study suggest that the effect of the combination of moderate activity and insomnia symptoms,and of low activity and insomnia symptoms,on the risk of developing poor mental health is greater than both the sum and the product of these risk factors.To our knowledge,this is the first study to report these associations and to highlight the potential that increasing PA and reducing insomnia symptoms in combination could reduce the odds of developing poor mental health.Approximately 10% of participants were in these 2 groups(Supplementary Table 4)and are likely to benefit from multicomponent interventions that target improvements in both PA and insomnia symptoms.
From a prevention and treatment perspective,PA interventions can reduce symptoms of depression and anxiety,6,12,39,40and interventions reducing insomnia symptoms can reduce depressive symptoms.30,45We are unaware of published interventions explicitly targeting combined improvements in PA and sleep specifically to improve mental health.There is some evidence that improvements in the overall pattern of PA and sleep during an intervention targeting improvements in PA and sleep quality can improve depression and stress.46However,this study was exploratory and not specifically designed to examine how improvements in PA and sleep quality effected mental health outcomes,and it included participants with a range of mental health symptoms as well as those without any symptoms.46Such multi-behavior interventions may leverage the overlap in the potential biological and psychological mechanisms linking physical inactivity and insomnia symptoms to depression and anxiety,such as changes in neuroplasticity,emotional regulation,inflammation,and psychological factors;6,10,47they may also effectively engage the bi-directional relationship between activity and sleep.16,17,23,41Given the impact of PA on a range of physical health outcomes(i.e.,cardiometabolic health,weight management),combined PA and sleep interventions may be useful for improving the physical health of individuals who are at risk of developing or who are living with poor mental health.2
An interesting observation in the current study was that the magnitude of associations was largely unchanged when sleep disturbance was examined (Tables 2 and 3;Fig.2;Supplementary Fig.1).This was somewhat surprising given other studies have observed that insomnia symptoms in the presence of short sleep duration have a larger magnitude of associations with a range of outcomes,including intermittent and chronic mental health symptoms14and cardiovascular disease,48than do insomnia symptoms without short sleep.These differences may be in part due to the current study’s use of a dichotomous classification for insomnia symptoms instead of multiple categories (e.g.,insomnia and short sleep,insomnia and recommended sleep,no insomnia and short sleep),which could potentially obscure the additional effect of insomnia symptoms and short sleep.
To our knowledge,the current study is the first to examine the relationship between combined categories of PA and insomnia symptoms and the onset of poor mental health in the general population.Additional strengths include the 5-year length of follow-up period,the representative populationbased cohort,and the statistical adjustment for a number of potential confounders,such as life events and physical health conditions,which can also be associated with poor sleep,inactivity,and poor mental health.It is possible that some of these confounders (e.g.,chronic disease) may be on the causal pathway between exposure and outcome and may,therefore,attenuate the associations observed.The potential of reverse causality and residual confounding due to prior poor mental health was addressed by omitting individuals with poor mental health (based on MHI-5 score) at baseline,adjusting for prior diagnosis of depression/anxiety,and examining the onset of poor mental health after at least 1 year of follow-up.Rates of loss to follow-up were higher among adults reporting insomnia symptoms,which has the potential to bias results.A generalized measure of poor mental health was used as the outcome,and additional studies are needed to explore how combinations of PA and insomnia symptoms are related to specific mental health outcomes,such as depression and anxiety,given previous evidence that PA can have different magnitudes of associations with these conditions.12PA was self-reported,which means it is subject to recall bias;consequently,participants in the current study may have been misclassified based on their reported PA level.
5.Conclusion
The results of the current study suggest that lower levels of PA were associated with increased odds of the onset of poor mental health among adults regardless of whether insomnia symptoms were present of not.However,among adults with insomnia symptoms,higher levels of PA appeared to reduce these odds and indicate some protective effect.More research on the synergies between these key lifestyle behaviors may help improve the understanding and management of poor mental health.
Acknowledgments
The findings and views reported in this paper are those of the authors and should not be attributed to either Department of Social Services or the Melbourne Institute.MJD is supported by a Career Development Fellowship(APP1141606) from the National Health and Medical Research Council,Australia.The funder had no role in the design or conduct of the current study.
Authors’contributions
MJD drafted the initial manuscript,conceptualized the study,and conducted the analyses;EGH critically reviewed and edited the manuscript,contributed to writing,critically reviewed the analysis plan,and oversaw the analyses;NWB critically reviewed and edited the manuscript,contributed to writing,and critically reviewed the analysis plan;NG critically reviewed and edited the manuscript,contributed to writing,and critically reviewed the analysis plan;SO critically reviewed and edited the manuscript,contributed to writing,and critically reviewed the analysis plan.All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Supplementary materials
Supplementary materials associated with this article can be found in the online version at doi:10.1016/j.jshs.2022.02.002.
 Journal of Sport and Health Science2023年3期
Journal of Sport and Health Science2023年3期
- Journal of Sport and Health Science的其它文章
- Impact loading in female runners with single and multiple bone stress injuries during fresh and exerted conditions
- Are EPB41 and alpha-synuclein diagnostic biomarkers of sport-related concussion?Findings from the NCAA and Department of Defense CARE Consortium
- Factors and expectations influencing concussion disclosure within NCAA Division I athletes:A mixed methodological approach
- Effects of contact/collision sport history on gait in early-to mid-adulthood
- Refinement of saliva microRNA biomarkers for sports-related concussion
- Lacrosse-related injuries in boys and girls treated in U.S.emergency departments,2000-2016
