Construction of cough ref lex intensity score for critically ill patients based on the Delphi method
Yong-kai Li, Yang Liu, Wen-bin Jia, Jian-zhong Yang, Jun Xu
1 Emergency Trauma Center, the First Affiliated Hospital of Xinjiang Medical University, Urumqi 830000, China
2 Emergency Department, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100730, China
3 Clinical Medical College & Affiliated Hospital of Chengdu University, Chengdu 610000, China
Airway management is important for critically ill patients.Improper airway management can directly threaten the life of patients.[1]Early correct airway assessment and effective airway management can improve patient prognosis.[2]Coughing ability plays an important role in the decision-making process of airway management.Patients with impaired coughing ability have a higher risk of tracheal intubation during treatment.The concept of cough strength was first proposed by Khamiees in 2001,[3]but the evaluation criteria did not include coughing ability.The purpose of this study was to assess patients’coughing ability through the Delphi method and expert consultation, to provide data support for establishing a cough reflex intensity score and to construct an advanced airway management model for quick and effective evaluation.[4,5]
METHODS
The inclusion criteria of consultation experts were as follows: (1) ten years of experience or more in emergency medicine, intensive care medicine, or other related medical fields; (2) attending physicians or above with at least a bachelor degree; and (3) volunteering to participate in this study and making recommendations to improve the cough ref lex intensity scores.
The research team consisted of two chief physicians and three graduate students in emergency medicine.A preliminary scoring system for evaluating the cough reflex intensity was developed based on a literature review and case studies on airway management (supplementary Table 1).[6]
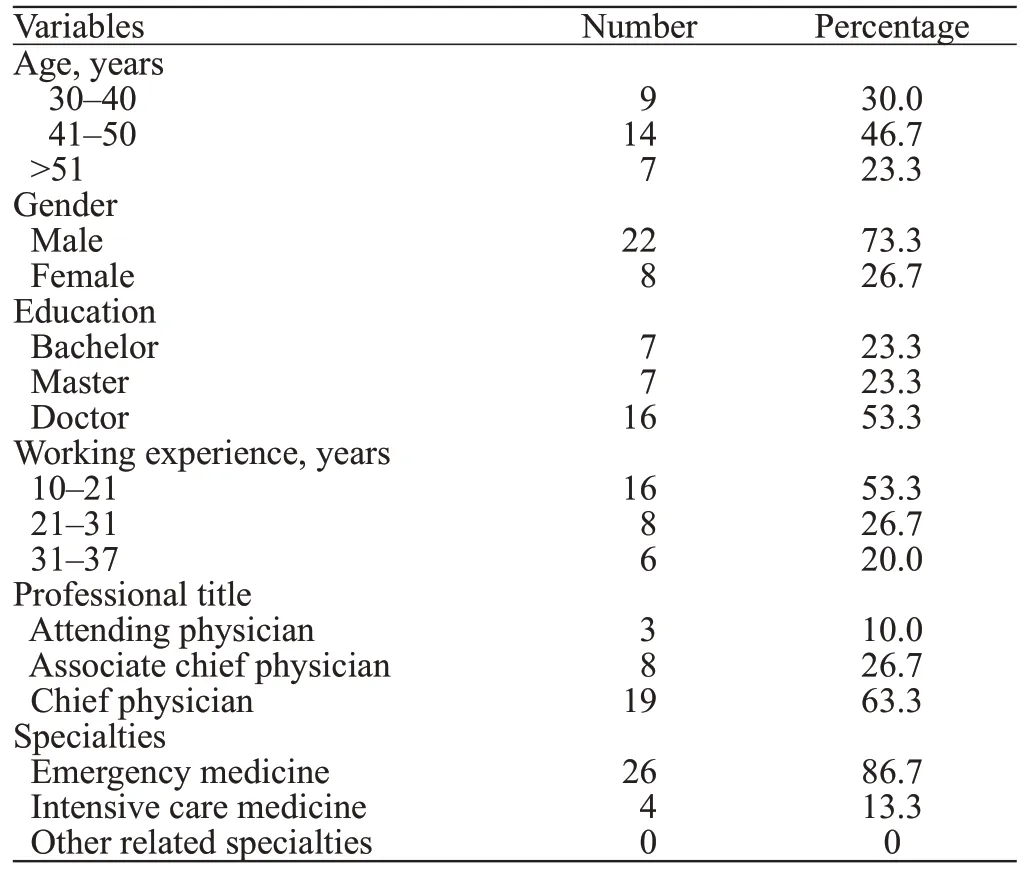
Table 1.Basic information about recruited experts
The first round of expert consultation was conducted through questionnaires distributed on site or by email.The scoring system was analyzed and revised according to expert opinions.The expert group discussed the potential inclusion of the new suggestions in the next round of survey.On the basis of literature evidence, each criterion in this study was required to have an approval rating of ≥70%, a mean value of the approval rating >4.0,and a coefficient of variation <0.25.[7]
All statistical analyses were conducted with SPSS version 26.0 (IBM, USA).Descriptive statistics and nonparametric tests were used to calculate the mean,standard deviation, active coefficient, authority coefficient,coordination coefficient, and variation coefficient.
RESULTS AND DISCUSSION
In our study, a total of 30 experts from Class A tertiary hospitals from different provinces, autonomous regions, and municipalities were selected for correspondence.Twentythree (76.7%) experts had master degree or above, 27(90.0%) had an associate chief physician title or above,and all 30 experts had worked for more than 10 years,indicating that the experts had rich experience in treating acute and critical illnesses (Table 1).
Active coefficient of experts
The active coefficient of experts is expressed as the effective response rate of the questionnaire.A response rate of more than 70% was considered good, representing a higher active coefficient.In this study, 30 letters were sent out in each round, and 30 letters were collected, with an effective response rate of 100%.In addition, after the first round of consultation,15 (50%) experts made 32 suggestions (25 of them were the same or similar).These results indicated that the experts were highly motivated and cooperative and considered this research work very important.
Authority coefficient of experts
The authority coefficient (Cr) is an important indicator that affects the accuracy of evaluation and prediction.It is usually determined by two factors: the judgment basis of the indicators (Ca) and the familiarity with the indicator (Cs).The calculation formula is Cr = (Ca+Cs)/2.The values of Ca and Cs were obtained mainly through the self-evaluation of the experts.The larger the Cr value is, the higher the authoritative coefficient, and Cr ≥ 0.7 is regarded as a high degree of authority coefficient.In this study, the authority coefficients in the two rounds were 0.820 and 0.905,indicating that the experts included in this study obtained a high degree of authority (supplementary Table 2).
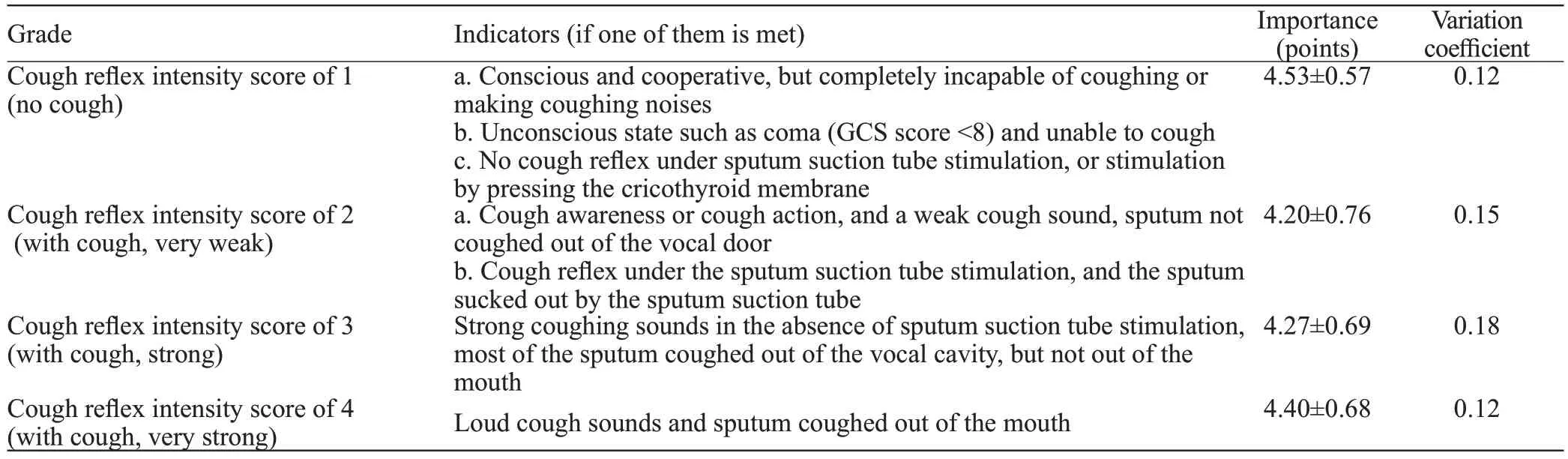
Table 2.The second round of investigation on cough ref lex intensity scores
Concentration and coordination of expert opinions
The coordination coefficient (W) indicates the coordination degree of expert opinions.In this study, the coordination coefficient of the Delphi method survey in round one was 0.064 (P=0.12), indicating unsatisfactorycredibility of the assessment or prediction of expert opinions.However, the coordination coefficient in round two was 0.1 (P=0.02), suggesting high credibility and good coordination of the assessment or prediction of expert opinions (supplementary Table 3).
Modification of entries
The entries with an expert approval rating of <70%were modified as follows.For the decibel of cough sound, most experts believe that the measurement was affected by many interference factors, so this parameter was excluded.Due to the differences in disease type and incidence rate, the Clinical Frailty Scale (CFS) is not applicable to acute and critically ill patients and is also deleted.The Glasgow Coma Scale (GCS) score was applied to patients with a cough intensity score of 1, which required a GCS score of <8, and the phrase“including post-tracheal intubation and tracheotomy”was deleted from the questionnaire.For the detailed indicators with cough intensity scores of 1 and 2, they were listed as a, b, c and a, b and can be scored if one of them is met.
In the second round of investigation, the expert agreement rate for each criterion was >80% (Likert score ≥4 indicated agreement), and the mean value of each item was >4.0 with a variation coefficient <0.25,indicating a convergence of expert opinions (Table 2).
CONCLUSION
Through two rounds of Delphi expert consultation,a cough reflex intensity score system was established,which was featured with good authority, reliability and comprehensiveness.It can provide a reference for effectively assessing the patient’s airway status and disease progress.Nevertheless, this scoring system needs to be further validated in future clinical practice.
Funding:This study was funded by the Autonomous Region Education Reform Project (PT2020023).
Ethical approval:The Ethics Committee of the First Affiliated Hospital of Xinjiang Medical University approved the study(reference number K201908-03).
Conflicts of interest:All authors declare that they have no Conflicts of interest.
Contributors:YKL and YL contributed equally to this work.YKL collected and analyzed the data and drafted the manuscript; YKL,YL, and WBJ organized, analyzed, and interpreted the data; YKL designed the study and was responsible for the integrity of the data and the accuracy of the data analysis; JZY and JX provided administrative, technical, and material support and provided the necessary theoretical guidance for this study.YL helped with the statistical analysis, and YKL and YL organized the data and performed the literature search.
All the supplementary files in this paper are available at http://wjem.com.cn.
 World journal of emergency medicine2023年3期
World journal of emergency medicine2023年3期
- World journal of emergency medicine的其它文章
- Most patients with non-hypertensive diseases at a critical care resuscitation unit require arterial pressure monitoring: a prospective observational study
- Over-expression of programmed death-ligand 1 and programmed death-1 on antigen-presenting cells as a predictor of organ dysfunction and mortality during early sepsis: a prospective cohort study
- Effects of continuous renal replacement therapy on inflammation-related anemia, iron metabolism and prognosis in sepsis patients with acute kidney injury
- Effects of early standardized enteral nutrition on preventing acute muscle loss in the acute exacerbation of chronic obstructive pulmonary disease patients with mechanical ventilation
- Development and validation of a predictive model for the assessment of potassium-lowering treatment among hyperkalemia patients
- The relationship between physical activity in early pregnancy and hypertensive disorders of pregnancy:a cohort study in Chinese women
