The relationship between physical activity in early pregnancy and hypertensive disorders of pregnancy:a cohort study in Chinese women
Qian Lu, Shi-jiao Yan,2, Huan-jun Chen, Xiong-fei Pan, Yi-xiang Ye, Xing-yue Song, Ri-xing Wang, Chuan-zhu Lyu
1 International School of Public Health and One Health, Hainan Medical University, Haikou 570100, China
2 Research Unit of Island Emergency Medicine, Chinese Academy of Medical Sciences, Hainan Medical University, Haikou 570100, China
3 Section of Epidemiology and Population Health, Ministry of Education Key Laboratory of Birth Defects and Related Diseases of Women and Children, West China Second University Hospital & West China Biomedical Big Data Center,West China Hospital, Sichuan University; Shuangliu Institute of Women's and Children's Health, Shuangliu Maternal and
Child Health Hospital, Chengdu 610041, China
4 Department of Epidemiology and Biostatistics, School of Public Health, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430000, China
5 Department of Emergency, Hainan Clinical Research Center for Acute and Critical Diseases, the Second Affiliated Hospital of Hainan Medical University, Haikou 570100, China
6 Emergency Medicine Center, Sichuan Provincial People's Hospital, University of Electronic Science and Technology of China, Chengdu 610072, China
7 Ministry of Education Key Laboratory of Emergency and Trauma, Hainan Medical University, Haikou 570100, China
KEYWORDS: Physical activity; Gestational hypertension; Preeclampsia; Prospective cohort study
INTRODUCTION
Hypertensive disorders of pregnancy (HDP) refer to hypertension that occurs after 20 weeks of pregnancy.[1,2]Gestational hypertension (GH) and preeclampsia (PE) are the two main subtypes of HDP.The global incidence of HDP is 5%–10%.[3]In China, the incidence of HDP is 6.4%.[4]
HDP is a serious complication of pregnancy, threatening the lives of mothers and children.HDPs can lead to secondary chronic hypertension and related cardiovascular diseases in pregnant women, such as stroke, liver or kidney failure,disseminated intravascular coagulation (DIC), multiple organ failure, and even death in severe cases.[1,3,5-7]Therefore, it is important to develop appropriate measures to prevent and manage HDP and its subsequent complications.
To date, the pathogenesis of HDP is not completely clear, and it is difficult to make early diagnoses in the clinic.Therefore, to prevent the occurrence of HDP and its complications, it is very important to determine its risk factors, especially modifiable risk factors.A previous epidemiological study has found that physical activity (PA)in early pregnancy has a protective effect on HDP,[8]possibly because exercise during pregnancy can improve endothelial function and promote angiogenesis, thus reducing the risk of disease.[9]At present, there is little evidence of a correlation between PA and HDP at home and abroad.Therefore, this study prospectively explored the relationship between PA and HDP in early pregnancy through a cohort study, providing a reference for the prevention of HDP and guidance for PA during pregnancy.
METHODS
Study design and participants
Data were collected from the Tongji-Shuangliu Birth Cohort (TSBC).[8]Detailed study design and procedures have been previously reported.[8]Pregnant women attending their first prenatal visit at a hospital were eligible for our study if they met the following criteria:[10](1) singleton pregnant women aged 18 to 40 years and (2) gestational age ≤15 weeks.Women were excluded if they (1) experienced assisted reproductive technology (such asin vitrofertilization or intrauterine insemination); (2) reported serious chronic diseases or infectious diseases (such as pre-pregnancy diabetes, cancer, tuberculosis or HIV infection); or (3) were unable to complete the questionnaire or refused to sign the informed consent form.By August 2020,6,820 eligible pregnant women had been recruited.This study was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology,Wuhan, China (the protocol number of the ethics approval was[2017] No.S225).All participants provided written informed consent at recruitment.
PA assessment
The Chinese version of the pregnancy physical activity questionnaire (PPAQ) was used in this study.It has good reliability and validity and is suitable for the investigation of pregnant women in China.[11]The PPAQ includes household/caregiving, occupational, sports/exercise, and transportation activities, with 32 activities in total.By multiplying the time spent in each activity by the intensity corresponding to each activity and summing these values, the average weekly total energy expenditure of the PA in the first trimester of pregnancy, expressed as metabolic equivalent of task (MET)h/week, was calculated.Activity intensity is determined according to the Outline of Physical Activity:[9]sedentary(<1.5 MET-h/week), light (1.5–2.9 MET-h/week), moderate(3.0–6.0 MET-h/week), and vigorous (>6.0 MET-h/week).PA variables of different intensities and types were divided into three tertiles, and the first tertile was used as the reference group.In this study, few pregnant women participated in moderate-intensity or vigorous-intensity PA, so they were combined for analysis and expressed as moderate-to-vigorous intensity PA (MVPA).
Diagnosis of HDP
GH: sustained blood pressure readings (systolic blood pressure [SBP] ≥140 mmHg [1 mmHg=0.133 kPa] or diastolic blood pressure [DBP] ≥90 mmHg), without associated proteinuria occurring after 20 weeks of gestation,based on the average of at least two measurements, with a 4-hour interval, using the same arm; for severe hypertension patients, the interval between the two measurements should be at least 15 min.[12,13]
PE: pregnancy-induced hypertension with marked proteinuria or without proteinuria but with maternal organ dysfunction, including acute kidney injury, liver involvement with or without right upper quadrant or epigastric pain,neurological complications, hematologic complications, and uteroplacental dysfunction.[12,14,15]
Covariate assessment
Data regarding demographic information, disease history,and family history were collected via interviews using structured questionnaires at recruitment.PA was assessed using the PPAQ.Pregnant women’s weight and height were measured by removing their shoes and socks.At baseline,the SBP and DBP of the left upper arm were measured using an Omron electronic sphygmomanometer, and the pregnant women rested for more than five minutes before the measurement.Pre-pregnancy body mass index (BMI) was calculated as self-reported pre-pregnancy weight in kilograms divided by the square of height in meters.
Statistical analyses
Baseline characteristics are expressed as the mean±standard deviation (SD) for continuous variables andn(%) for categorical variables.The Chi-square test was used to compare the general characteristics between the GH group and the PE group.The Wilcoxon rank sum test was used to compare the energy expenditure of different intensities and different types of PA between pregnant women with GH and PE.With the first tertile as the reference group, unconditional logistic regression was used to analyze the relationship between PA in early pregnancy and GH and PE.Relevant confounding factors were further adjusted.The adjusted odds ratio (OR) value and its 95% confidence intervals (95%CI) were calculated.All analyses were performed with SPSS software (version 25.0), and aP-value <0.05 was considered significantly different.
RESULTS
Baseline characteristics of study participants
Among the 6,820 women who met the baseline inclusion criteria, the GH incidence was 1.8% (n=126), and the PE incidence was 0.8% (n=52).Family history of hypertension,pre-pregnancy BMI, HDP history, parity, gestational diabetes mellitus (GDM), mean SBP and DBP at the first delivery were correlated with GH incidence, and the differences were statistically significant (P<0.05).GH was related to GDM.Family history of hypertension, pre-pregnancy BMI, SBP,and DBP were correlated with the incidence of PE, and the differences were statistically significant (P<0.05) (Table 1).
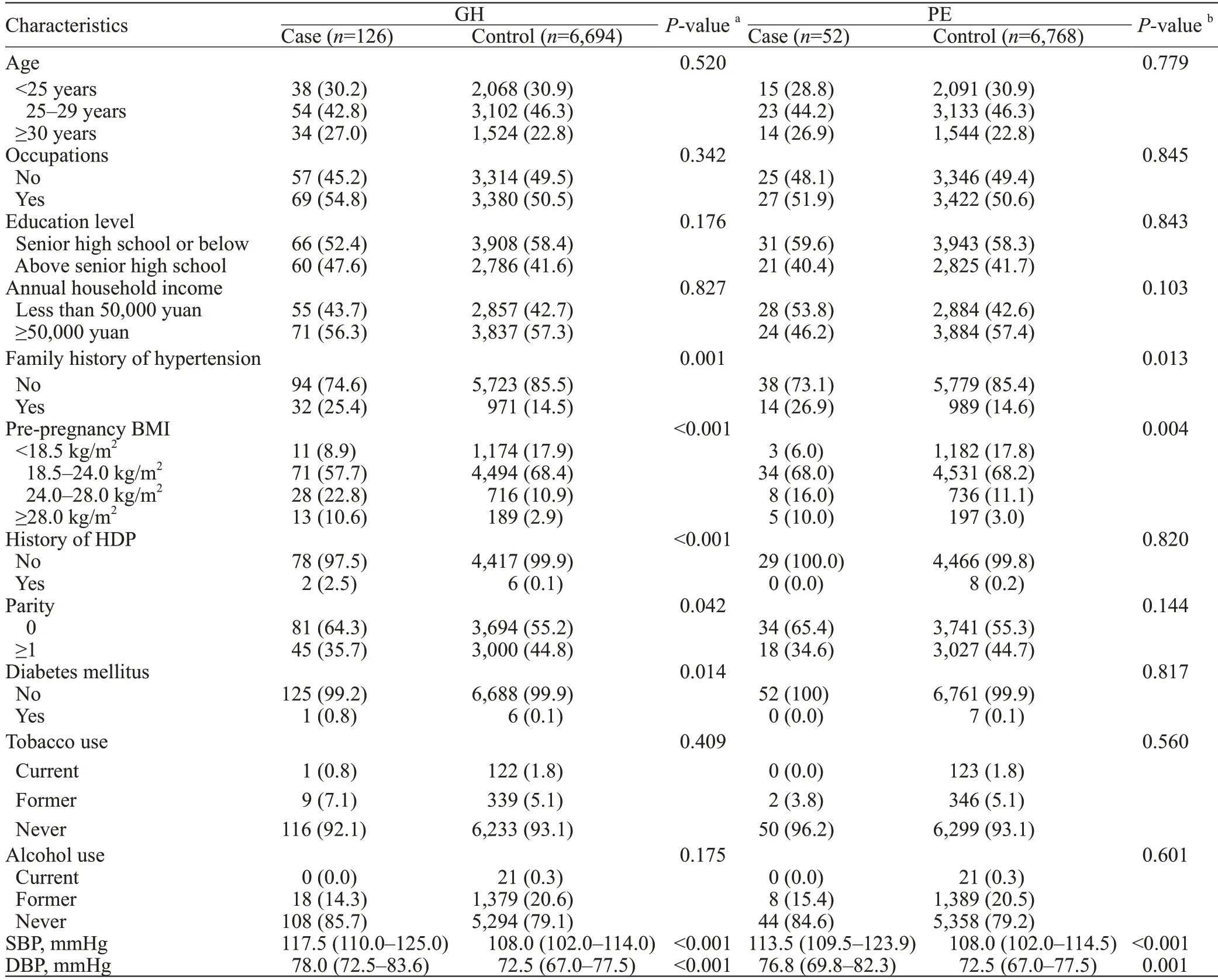
Table 1.Characteristics of the study participants by GH and PE
Energy expenditure of PA in pregnant women with GH and PE
The total PA was slightly higher in the PE group than in the GH group (123.5 MET-h/week vs.118.0 MET-h/week).Among the types of PA in the first trimester, the energy expenditure of household/caregiving activities was the highest in the GH and PE groups.Compared with the PE group, the energy expenditure of MVPA in the first trimester was significantly lower in the GH group(P<0.05), but there was no significant difference in the energy expenditure of the total PA, sedentary-intensity PA, light-intensity PA, household/caregiving activities,occupational activities, sports/exercise activities, or transportation activities (Table 2).
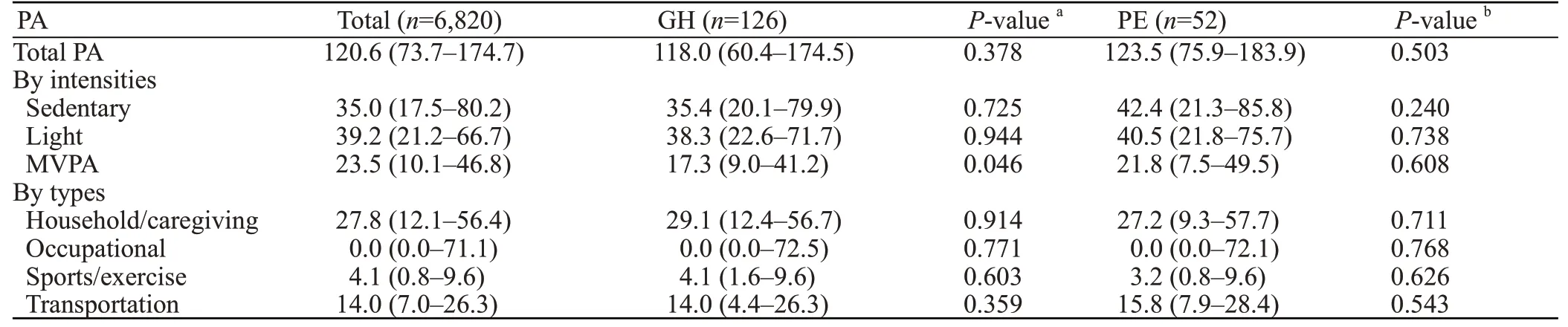
Table 2.Energy expenditure from PA during early pregnancy in women with GH and PE, MET-h/week
Odds ratio of HDP by intensities and types of PA in early pregnancy
In unadjusted analyses, the risk of GH was 37% lower in the second tertile of MVPA (OR0.63, 95%CI0.41–0.98)than in the first tertile.After adjusting for confounding factors such as age, occupation, education level, annual family income, family history of hypertension, pre-pregnancy BMI,history of HDP, presence or absence of diabetes, tobacco use,alcohol use, SBP, DBP, the risk of GH was significantly lower in the third tertile of MVPA (OR0.54, 95%CI0.31–0.96,Pfor trend=0.104) than in the first tertile.Pregnant women had a 46% lower risk of GH (supplementary Table 1).We also evaluated the association between PA and PE in early pregnancy (Table 2).No statistically significant difference was observed between PA and PE in the first trimester, regardless of different intensities or types of PA (supplementary Table 2).
DISCUSSION
In this prospective cohort study, we found that the incidence of HDP was 2.6%, GH 1.8%, and PE 0.8%.Higher levels of MVPA in early pregnancy was associated with a reduced risk of GH.In addition, we did not observe a statistical association between total PA or other types of PA during pregnancy and GH.
The incidence of HDP and its subtypes varies in different countries and regions.The specific reasons are not clear and may be different from the definition and classification of HDP or may be related to the lifestyle and region of the study subjects.
A previous study on pregnant women in the United States concluded that the incidence of HDP was as high as 14.6%, which was found to be related to old maternal age, black race, obesity, diabetes and other risk factors for HDP.[16]A retrospective cohort study in Romania showed an HDP incidence of 3.7%.[17]The HDP incidence was lower in Romania than in the USA, possibly because the women in their study were young white women and only 7% were obese.[17]Therefore, the incidence of HDP is closely related to many aspects of motherhood.
Previous studies have assessed the association between PA in early pregnancy and HDP and have generally suggested a protective effect.[18-20]Among them, Martínez-Vizcaíno et al[20]showed that the PE incidence was reduced only when exercise was initiated during the first trimester of pregnancy,and they specified the optimal start time, duration, and intensity of PA.Spracklen et al[21]have showed that increasing PA levels during pregnancy could effectively reduce the risk of PE, while women with higher levels of sedentary activity had a higher risk of PE.Mate et al[22]suggested that pregnant women should maintain a healthy lifestyle from preconception to postpartum, mainly reflected in diet and PA, to reduce the risk of PE.It may be that the biological mechanism of PE is characterized by placental dysplasia, oxidative stress,inflammation and endothelial dysfunction, while PA during pregnancy is conducive to the growth and development of the placenta, stimulates antioxidant defense, increases the number of mitochondria in the body, and makes the body more resistant to oxidative stress.[21]
However, the relationship between PA and HDP during pregnancy remains controversial.da Silva et al[23]compared randomized controlled trials and cohort studies to show that PA in pregnant women was not associated with PE risk, but they conducted only three trials.In a case-control study that simultaneously assessed the effect of different types of PA on the risk of GH and PE, they found that women with higher levels of PA during pregnancy had a lower risk of PE, while women with higher levels of sedentary activity had a higher risk of PE.[21]
Limitations
There are some limitations to this study.The main limitation is that the study population did not adopt the probability sampling method to infer the characteristics of the whole population from the sample characteristics, which affected the research results to some extent.At present, there is no clear recommended standard of PA during pregnancy in China, and further studies are needed in the future.
CONCLUSIONS
This study suggests that higher levels of MVPA in early pregnancy are associated with the risk of GH,but different types of PA in early pregnancy are not associated with GH.No statistically significant difference was observed between PA and PE in the first trimester,regardless of different intensities or types of PA.Further confirmation of this finding in larger prospective studies and investigation of the underlying biological mechanisms are needed.
ACKNOWLEDGEMENTS
The authors thank the study participants of the Tongji-Shuangliu Birth Cohort for their support and the physicians and nurses in the Shuangliu Maternal and Child Health Hospital for their collaboration in conducting this project.
Funding:This study was supported by Hainan Provincial Natural Science Foundation of China (821QN414, 822RC845, 821RC557), the Central Guidance on Local Science and Technology Development Fund of Hainan Province (ZY2021HN19), Hainan Clinical Medical Research Center Project (LCYX202205).
Ethical approval:The Tongji-Shuangliu Birth Cohort was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China (the protocol number of the ethics approval was [2017] No.S225).All participants provided written informed consent before enrolment.
Conflicts of interest: The authors declare that they have no conflicts of interest.
Contributors:QL and SJY contributed equally to this work.QL,SJY, HJC, and XYS conceived and designed the study.QL, SJY, HJC,and XYS participated in the acquisition and analysis of data.QL and SJY drafted the manuscript, and XFP, XYS, RXW, CZL revised the manuscript.All authors read and approved the final manuscript.CZL is the guarantor of this work, has full access to all data in the study, and takes responsibility for its integrity and the accuracy of the data analysis.
All the supplementary files are available at http://wjem.com.cn.
 World journal of emergency medicine2023年3期
World journal of emergency medicine2023年3期
- World journal of emergency medicine的其它文章
- Most patients with non-hypertensive diseases at a critical care resuscitation unit require arterial pressure monitoring: a prospective observational study
- Over-expression of programmed death-ligand 1 and programmed death-1 on antigen-presenting cells as a predictor of organ dysfunction and mortality during early sepsis: a prospective cohort study
- Effects of continuous renal replacement therapy on inflammation-related anemia, iron metabolism and prognosis in sepsis patients with acute kidney injury
- Effects of early standardized enteral nutrition on preventing acute muscle loss in the acute exacerbation of chronic obstructive pulmonary disease patients with mechanical ventilation
- Development and validation of a predictive model for the assessment of potassium-lowering treatment among hyperkalemia patients
- Mutual promotion of mitochondrial fission and oxidative stress contributes to mitochondrial-DNAmediated inflammation and epithelial-mesenchymal transition in paraquat-induced pulmonary fibrosis
