Most patients with non-hypertensive diseases at a critical care resuscitation unit require arterial pressure monitoring: a prospective observational study
Emily Engelbrecht-Wiggans, Jamie Palmer, Grace Hollis, Fernando Albelo, Afrah Ali, Emily Hart, Dominique Gelmann, Iana Sahadzic, James Gerding, Quincy K.Tran,,, Daniel J.Haase,
1 University of Maryland School of Medicine, Baltimore 21201, USA
2 The Research Associate Program in Emergency Medicine and Critical Care, Department of Emergency Medicine,University of Maryland School of Medicine, Baltimore 21201, USA
3 Department of Emergency Medicine, University of Maryland School of Medicine, Baltimore 21201, USA
4 Program in Trauma, the R Adams Cowley Shock Trauma Center, University of Maryland School of Medicine, Baltimore 21201, USA
KEYWORDS: Non-hypertensive diseases; Invasive arterial blood pressure; Non-invasive blood pressure
INTRODUCTION
Non-invasive blood pressure (NIBP) is the most common way to monitor patients’blood pressure (BP) and mean arterial pressure (MAP) in the acute care setting.A previous study suggested that in the intensive care unit(ICU), NIBP measurements are less accurate than the gold standard of invasive arterial BP (IABP) measurements;[1]however, IABP use can result in rare complications, such as ischemia, hematoma formation, and local or catheter-related infection or sepsis.
Although NIBP values significantly differ from IABP values in the acute care setting, previous smaller studies in both hypertensive[2]and non-hypertensive[1]patient populations have not investigated whether this discrepancy was associated with a change of management (COM).A study by Keville et al[3]suggested that there was a potential COM in 9% of patients with non-hypertensive disease states;however, this study was limited by its retrospective nature, for which the authors used a hypothetical definition for a COM.
Our study prospectively investigated the prevalence of a COM when IABP was initiated among a larger group of patients with non-hypertensive disease states.We hypothesized that the differences between IABP and NIBP among non-hypertensive patients would result in clinically significant changes in their BP management.Furthermore,we studied predictors associated with a COM as well as complications from arterial catheter cannulation.This information would provide clinicians with further evidence regarding the utility of IABP monitoring in the acute care setting.
METHODS
Study setting
This prospective observational study was performed at the critical care resuscitation unit (CCRU) of the University of Maryland School of Medicine from February 1, 2019, to May 31, 2021.It is standard CCRU practice to place arterial catheters in patients who are receiving continuous infusions of vasopressors, inotropes, or anti-hypertensive medications,as well as those who are at high risk for hemodynamic decompensation.Per institutional policy, arterial catheter placement is performed by CCRU clinicians, and BP measurements are documented hourly.In the event of a lost waveform, the arterial catheter is replaced, as clinicians rely upon these measurements for hemodynamic monitoring.
Patient selection
We consecutively enrolled all adult patients who had non-hypertensive disease states and required IABP for hemodynamic monitoring during their CCRU stay.Patients with a hypertensive emergency or who only needed an arterial catheter for blood draws were excluded.We excluded patients who did not have a NIBP reading within 60 min of an IABP reading, as greater than 60 min was deemed too long for direct comparison between these ideally simultaneous measurements.We also excluded patients who already had an existing form of hemodynamic monitoring, such as an arterial catheter or pulmonary artery (PA) catheter, prior to arrival at the CCRU since we could not ascertain whether they had a COM with arterial catheter insertions prior to arrival at the CCRU.
The study protocol was reviewed and approved by the Institution Review Board of University of Maryland School of Medicine.No formal consent was required as it was an observational study of standard clinical practice.
Outcome measures
The primary outcome of the study was the prevalence of a COM between IABP and NIBP monitoring.The secondary outcomes were the potential independent variables that may have associations with a COM.
Blood pressure management
After arterial catheter insertion, but before leveling and zeroing, a NIBP was obtained.The CCRU clinician stated a plan for addressing the BP in the clinical context of the patient.The IABP was then revealed, and the CCRU clinician would assess the quality of the waveform and decide which mode (NIBP or IABP) would be used for monitoring.The clinician would then use the chosen BP monitoring mode to determine how to address the BP.
A clinical COM was defined as a change in direction of pharmacological interventions.For example, a clinical COM occurred when the NIBP value indicated no change in the current dose of vasoactive infusion, while the IABP value suggested an increase in the current dose of vasoactive infusion to increase the patient’s MAP.In contrast, no COM occurred when both NIBP and IABP values suggested increasing doses of vasoactive infusion.
Data collection
Relevant data, including demographics such as age,sex, body mass index (BMI), and past medical history,and clinical data, were collected from patients’electronic medical records.Race and ethnicity were not deemed significant factors for our outcome measures and thus were not collected.Clinical data included diagnosis, medications administered within 1 h prior to (e.g., intravenously pushed medications) or at the time of arterial catheter insertion (e.g.,continuous infusion), and components for the Sequential Organ Failure Assessment (SOFA) score.For missing SOFA score components, normal values were imputed.Other collected data included white blood cell (WBC) counts,hemoglobin levels, serum lactate levels, crystalloid intake,and echocardiogram results.We also collected patient outcomes, including arterial catheter complications, length of hospital stay, and discharge destination.Arterial catheter complications were defined as any necrosis of the hand,wrist, fingers, or extremity identified as a source of local or bloodstream infection or any bleeding or (pseudo)aneurysm.Complication data were gathered from arterial catheter insertion procedure notes, nursing records when arterial catheters were removed, and discharge summary notes.
Data were collected and entered into a standardized Excel spreadsheet (Microsoft Corp., USA).To minimize bias and to validate the data after collection was completed, multiple investigators independently checked the data for accuracy.Discrepancies were validated by a senior investigator.
Sample size calculations
We calculated our sample size according to a report that up to 20% of patients with septic shock had a MAP difference between IABP and NIBP of ≥10 mmHg (1 mmHg=0.133 kPa).We decided that a MAP difference of 10 mmHg would be clinically relevant.[4]Therefore, we estimated that we would need approximately 200 pairs of IABP and NIBP measurements to detect a difference of 10 mmHg with a power of 80% and an alpha of 0.05.
Data analysis
Descriptive analysis was used to present the patients’information.Continuous variables were described as a mean±standard deviation (SD) or median (interquartile range [IQR]), while categorical variables were reported as percentages, as appropriate.Student’st-test and Mann-WhitneyU-test were used to compare differences between groups of continuous variables, while a Chi-square test was used for categorical variables, as indicated.
A Bland-Altman plot was used to graphically compare the difference between IABP and NIBP.The average MAP of NIBP values are displayed on theX-axis, and the MAP difference between IABP and NIBP is displayed on theY-axis.We also indicated the clinically significant regions where the MAP difference between IABP and NIBP was>10 mmHg or ≤10 mmHg.
We used a classification and regression tree (CART)analysis to identify independent variables most associated with a COM in patients’BP management.All independent variables were selected apriori ( supplementary Table 1).The CART algorithm performed multiple recursive partitioning of interactions between independent variables and the outcome (yes vs.no COM) to provide a series of dichotomous splits (yes vs.no COM) and to generate a decision tree.The CART then assigned the independent variable with the most significant associations with the outcome a “relative variable importance”(RVI) value of 100%.Other factors having significant associations with the outcome were subsequently given RVI values as a percentage of the most important independent variable.Descriptive and CART analyses were performed with Minitab version 19.0 (Minitab, USA).We considered all variables withP<0.05 statistically significant.
RESULTS
Patient characteristics
We identified and analyzed the records of 206 patients who met the inclusion criteria ( supplementary Figure 1).We identified 94 ( 45.6%) patients who had a COM.The average patient age was 57±16 years, and the mean BMI was 31±10 kg/m2.There were no statistically significant differences between patients with a COM compared with those without a COM regarding their demographics, past medical history,laboratory values, or amount of crystalloids within 4 h of arterial cannulation (supplementary Table 2).However, there were higher percentages of patients with a COM among those who had received norepinephrine at the time of arterial cannulation as compared to patients without a COM (47.9%vs.28.6%, respectively,P=0.004) (supplementary Table 2).Among patients diagnosed with hemorrhagic shock,there were higher percentages of patients without a COM as compared to patients with a COM (15.2% vs.6.4%,respectively,P=0.04) (supplementary Table 2).
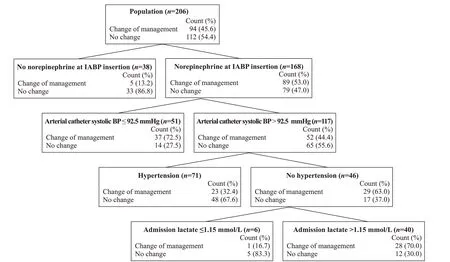
Figure 1.Classification and regression tree analysis decision tree.IABP: invasive arterial blood pressure; BP: blood pressure.
The median [IQR] number of arterial catheter days was 2.5 [1–5] d for patients with a COM, which was similar to those without a COM (2.5 [1–4] d) (P=0.63) ( supplementary Table 2).Additionally, patients without a COM were more likely to be discharged home than those with a COM(39.3% vs.24.5%, respectively,P=0.03).No complications from arterial catheters were reported among all patients(supplementary Table 2).
Primary outcome
The most common change among all patients was to increase the dosage of the current infusion (40/206 patients,19.4%).Compared to patients without a COM, patients with a COM were more likely to require an increased dose of their current infusion (32/94 [34.0%] vs.8/112 [7.1%],P=0.001)or an addition of another medication (29/94 [30.9%] vs.9/112 [8.0%],P=0.001) (supplementary Table 2).
The decision tree diagram (Figure 1) showed that patients who did not receive norepinephrine at the time of arterial cannulation were associated with higher percentages of no COM than COM (86.8% [33 patients]) vs.13.2%[5 patients]) (Figure 1).In contrast, among patients who received norepinephrine at the time of arterial cannulation,89 (53.0%) patients had a COM, compared with 79 (47.0%)patients without a COM (Figure 1).From the patients who received norepinephrine without a history of hypertension,patients whose serum lactate level was >1.15 mmol/L were more likely to have a COM (70.0% [28 patients] vs.30.0%[12 patients]) (Figure 1).
The CART identified receiving norepinephrine at the time of arterial catheter insertion (RVI=100%) as the most significant factor associated with a COM, followed by a history of hypertension and arterial SBP (RVI=52% for both)(Figure 2).
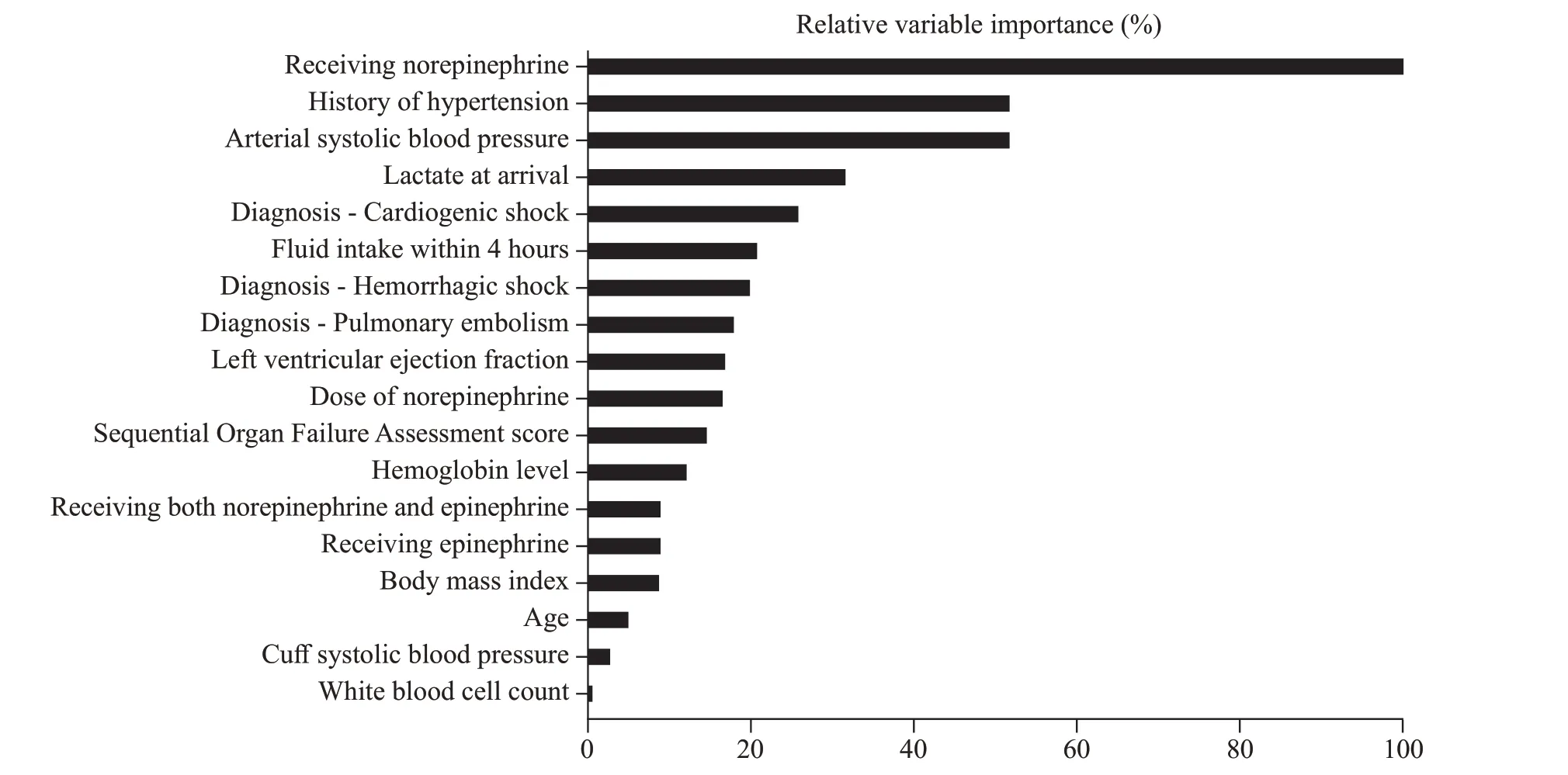
Figure 2.Relative importance of variables identified in the cart decision tree.
Secondary outcome
Overall, the mean NIBP MAP was 4 mmHg higher than that with IABP, and a lower arterial MAP was associated with a COM (P=0.001) (supplementary Table 2).Figure 3 also indicated that in general, IABP reported lower values than NIBP; it also showed that there were higher percentages of patients who had [IABP-NIBP] difference ≤ –10 mmHg(45 patients [21.8%]) than the number of patients who had[IABP-NIBP] difference ≥ +10 mmHg (9 patients [4.4%])(Figure 3,Y-axis & supplementary Table 2).The MAP differences for the sub-groups of receiving norepinephrine and serum lactate levels are outlined in supplementary Figures 2 and 3.
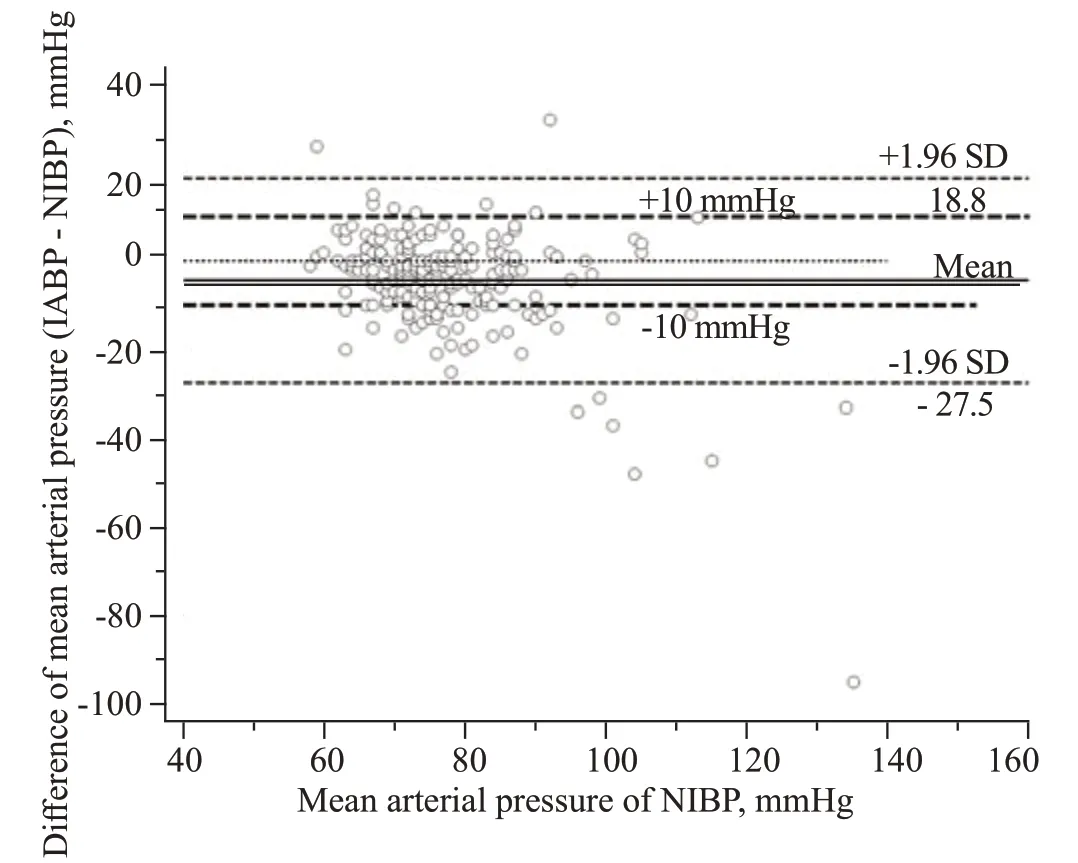
Figure 3.Bland Altman plot of the mean arterial pressure difference among all patients.IABP: invasive arterial blood pressure; NIBP: noninvasive arterial blood pressure.
DISCUSSION
Our prospective study showed that arterial BP monitoring was associated with a COM in approximately 45.6% of patients with non-hypertensive disease states.Most of changes in management were an increase from the current vasoactive medication.Our CART analysis also identified a few independent variables that were associated with a COM among our patient population.
Our study showed that 22% of patients had NIBP MAP values >10 mmHg higher than the values for IABP, which means that the IABP method was able to detect hypotension that was otherwise not detected by cuff BP monitoring(occult hypotension) in 1 of every 5 patients.Our study’s findings were different from those of a previous study by Riley et al,[1]which stated that there was a difference of >10 mmHg in MAP between IABP and NIBP but did not report on the clinical relevance.We found a COM in almost half of our patient population.Additionally, the percentage of our patients with a real-time COM was even higher than that in a previously reported retrospective study with hypothetical assumptions of clinical management.[3]The importance of detecting hypotension is highlighted in a previous study by Walsh et al,[4]which found that a brief period of hypotension lasting 5 min during the intraoperative period was associated with an 18% higher likelihood of developing acute kidney injury and a 30%higher likelihood of developing myocardial infarction.Furthermore, early vasopressor administration has been shown to improve in-hospital mortality among patients with septic shock.[5]Thus, detecting and treating hypotension early in the acute resuscitation phase could reduce organ damage and mortality.
Receiving norepinephrine was identified as an important independent variable associated with a COM in our study population.Our findings were in agreement with previous studies showing that IABP measurements among patients receiving norepinephrine were usually lower than NIBP measurements.[1,6]Furthermore, patients with cardiogenic shock who received a norepinephrine infusion at a dosage of ≥0.6 μg/(kg·min) were associated with the highest discordance between IABP and NIBP measurements compared to patients who received lower dosages of norepinephrine infusion,[6]thus resulting in a higher likelihood of a COM.Norepinephrine causes vasoconstriction via α-1 receptors and may exert greater dose-dependent vasoconstrictions[7]in the peripheral arteries (radial arteries) than the proximal arteries (brachial arteries), where BP cuffs are usually placed.Therefore, a higher dose of norepinephrine is associated with a higher likelihood of differences between IABP and NIBP,[6]and a higher likelihood for a COM.Our results provided further information to support the Surviving Sepsis Campaign’s recommendation that patients receiving vasopressors should receive arterial monitoring.When patients are in shock,using NIBP may overestimate the BP, causing these patients to be at higher risk of occult hypotension.
Admission serum lactate levels as low as 1.15mmol/L was also identified as a significant factor (RVI=31.6%)for COM in our patient population.Serum lactate levels ≥2 mmol/L indicate hypoperfusion,[8]or shock, which prompts the use of vasopressors; this may illustrate the correlation of higher rates of a COM among the patients who had elevated serum lactate levels.Additionally, the finding that serum lactate was a significant factor in a COM is consistent with a previous retrospective study that found that each unit increase in serum lactate was associated with 11% higher odds of a COM with IABP.[3]Until more data become available, we recommend that clinicians consider using IABP in this high-risk patient population.
A previous study found that patients who had IABP monitoring were not associated with improved mortality[9]as compared to NIBP monitoring but that arterial catheters were associated with complications.However, the reported prevalence of complications is low, with rates estimated at less than 1%[2]or 0.9/1000 catheter days.[10]Our study found no instances of complications.This discrepancy between the literature and our study could be due to the limited number of patients included in our study or possibly due to strict observation of our institutional policies when performing arterial cannulations, which could help prevent catheter-associated blood stream infections, as well as other complications.Overall, IABP monitoring is associated with low rates of complications and provides the benefit of detecting hypotension that otherwise would not be detected via NIBP monitoring among a high-risk patient population.Therefore, clinicians in the acute resuscitation phase should consider using IABP monitoring until further studies about the risk-to-benefit ratios for IABP are available.
Limitations
There are several limitations to our study.Our study utilized a group of patients with heterogeneous disease states that were managed in the acute resuscitation phase.Therefore, our findings may not apply to other ICU settings where IABP monitoring is also frequently utilized.Another limitation was that the majority of our patients had arterial catheters in their radial arteries, which are hypothesized to be more prone to vasoconstriction by norepinephrine.Thus,our patient population may have had a different [IABPNIBP] discordance rate if we had more patients with arterial catheters in femoral arteries.
CONCLUSIONS
Approximately 45.6% of critically ill patients with nonhypertensive diseases had a COM when IABP monitoring was initiated.Norepinephrine infusion and serum lactate levels were among the significant independent variables associated with a COM.Due to the low risk of complications among our patients, clinicians should implement early and frequent IABP monitoring in critically ill patients with non-hypertensive diseases.Further studies should focus on patient outcome data among these high-risk patients.
Funding:None.
Ethical approval:The study protocol was reviewed and approved by the University of Maryland Institution Review Board (HP-00079864).
Conflicts of interest:The authors declared there are no conflicts of interest.
Contributors:EEW: validation, investigation, data curation,writing – original draft, writing – review & editing, visualization; JP:investigation, data curation, writing – original draft, writing – review& editing; GH: formal analysis, investigation, data curation, writing –original draft, writing – review & editing; FA: writing – original draft,writing – review & editing; AA: validation, investigation, writing –original draft, writing – review & editing; EH: validation, data curation,writing – original draft, writing – review & editing; DG: investigation,data curation, writing – original draft, writing – review & editing;IS: writing – original draft, writing – review & editing; JG: data curation, writing – original draft, writing – review & editing; QKT:conceptualization, methodology, formal analysis, writing – original draft, writing – review & editing, project administration, corresponding author; DJH: conceptualization, methodology, writing – original draft,writing – review & editing, guarantor.
All the supplementary files in this paper are available at http://wjem.com.cn.
 World journal of emergency medicine2023年3期
World journal of emergency medicine2023年3期
- World journal of emergency medicine的其它文章
- A 94-year-old patient with severe burns: a case report
- Pregnancy-related spontaneous coronary artery dissection after intravenous ritodrine infusion: a case report
- Twelve family members with tetramine poisoning after consumption of vegetables grown in polluted soils
- Resuscitative endovascular balloon occlusion of the aorta in the treatment of severe hemorrhagic shock caused by upper gastrointestinal bleeding
- A rare case of purulent pericarditis secondary to subdiaphragmatic abscess
- Laryngeal mask airway bougie ultrasonography guided intubation in a morbidly obese patient with difficult airway
