Laryngeal mask airway bougie ultrasonography guided intubation in a morbidly obese patient with difficult airway
Rachana Bhat, Preeti Yadav, Jyothiswaroop Bhaskararayuni, Akhil Neseem, Savan Kumar Nagesh, Prakash Ranjan Mishra
1 Department of Emergency Medicine, Kasturba Medical College, Manipal Academy of Higher Education, Manipal 576104,India
2 Department of Emergency Medicine, All India Institute of Medical Sciences, New Delhi 110029, India
3 Department of Anaesthesiology, All India Institute of Medical Sciences, New Delhi 110029, India
4 Department of Anaesthesiology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal 576104, India
Airway management of morbidly obese patients is challenging due to inherent anatomical and physiological variations.[1]The frequent association of compromised hemodynamics, hypoxemia, or acidosis in an emergency department (ED) setting adds to the difficulty of the procedure.Rapid airway management position (RAMP),awake fiber-optic guided intubation, use of intubating laryngeal mask airway (ILMA), and video-laryngoscope are a few techniques that have been described to tackle difficult airways in these patients.[2]Studies have shown that the availability of fiber-optic scopes (3%–60%), videolaryngoscopes (39%–88%), and laryngeal mask airways(LMA) (65%–83%) varies in different ED settings.[3,4]Furthermore, a lack of adequate training and the need for time-bound resuscitation make implementation of the above techniques challenging.Supraglottic airway devices(SADs) are potential rescue airway devices with a fastlearning curve.Point-of-care ultrasound (POCUS) is an easily available, convenient adjunct for airway management in emergency and critical care settings.Various studies have shown the utility of POCUS in the confirmation of correct endotracheal tube placement in real time.[5,6]
We describe a technique of intubation using the LMA bougie ultrasonography (L-B-US) technique in a morbidly obese patient.
CASE
A 36-year-old woman, morbidly obese (estimated body mass index [BMI] >40 kg/m2), was referred to our center for management of urosepsis, septic shock,and multiorgan dysfunction syndrome (MODS).During transfer to our center, the patient had a seizure, and a LMA (AMBU LMA size 4; AMBU®, Denmark) was placed by the paramedic for airway control.On arrival to the ED, the initial assessment revealed a first-generation LMAin situ, respiratory rate of 32 breaths/min, oxygen saturation of 98% (on 100% fraction of inspiration O2[FiO2]) and bilateral crepitation on auscultation.Heart rate was 136 beats/ min, and blood pressure was 100/40 mmHg (1 mmHg=0.133 kPa).Her Glasgow Coma Scale was E2VTM5.Conjunctival chemosis, icterus, and bleeding from the oro-nasal cavity (probably mucosal)were other findings on examination.Initial blood gas indicated mixed metabolic and respiratory acidosis with pH 7.16, PCO257 mmHg, bicarbonate 18 mmol/L,and PO251 mmHg.Taking into consideration the risk of aspiration, hemodynamic instability, and need for optimizing ventilation, a decision was made to intubate the patient.
Obesity, short neck, large tongue, restricted mouth opening, and oral bleeding made the procedure an anatomically difficult airway; coexisting hemodynamic instability, acidosis, and hypoxia made it a physiologically difficult airway with a high risk of peri-intubation arrest.Furthermore, the short neck and propensity for bleeding make it a potentially difficult surgical airway in cases of failed endotracheal intubation.
The intubating team consisted of a physician and an emergency nurse trained in POCUS (Figure 1).For ultrasonography, a high-frequency linear probe was used(HFL38x, 13-6 MHz bandwidth, Sonosite M-Turbo®;FUJIFILM Sonosite®, USA).Initial screening ultrasound of the airway was performed to look for any aberrant vessels in the neck and mark the cricothyroid membrane.The patient was placed in the ramped position.Thorough suctioning of the oral cavity was performed.Preoxygenation was continued via the LMA with the ventilator.Injection ketamine 50 mg and rocuronium 50 mg were used as the induction and paralysing agents, respectively.The ultrasound probe was placed horizontally just above the suprasternal notch to view the airway at the level of the upper tracheal rings and esophagus in the same axial plane.It is important to note that the air in the LMA cuff may obscure visibility at the level of the glottis.A bougie was inserted through the LMA.POCUS was used for dynamic tracking of the bougie passing through the trachea, which appeared as a bright dot on cross-section.Position was also confirmed by simultaneous absence of post echoic shadowing at the esophagus indicated by an intact hyperechoic line of the transverse process of the cervical vertebra behind the esophagus (Figure 2 and supplementary video).Following this, the LMA was removed, keeping the bougiein situ.Laryngoscopy was performed (Cormack-Lehanne Grade 3), and a size 7 endotracheal tube (ETT)was railroaded over the bougie.The position of the ETT was again confirmed with ultrasound.The double tract sign,which is a sign of esophageal intubation, was absent.Right mainstem bronchus intubation was ruled out by the presence of left-lung sliding.The ventilator circuit was connected to the ETT, and correct placement was reconfirmed with the end-tidal carbon dioxide (ETCO2) curve.

Figure 1.A “representative”image depicting the setup during the L-B-US technique.
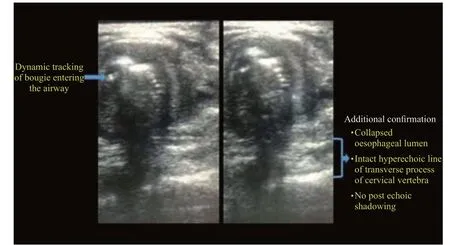
Figure 2.Tracking of bougie placement and confirmation with airway ultrasonography.
DISCUSSION
In this case, we discussed the combination of the use of LMA bougie and ultrasound for the management of a difficult airway in a morbidly obese patient.
Intubation in critically ill patients with challenging neck anatomy and compromised physiological reserves[7]aggravates the risk of peri-intubation deterioration, making rapid first-pass intubation success crucial.SADs have proven to be very effective and easy-to-use equipment with a relatively high success rate, especially in difficult airway situations.[8]It holds the advantage of providing adequate oxygenation and ventilation and can be utilized for preoxygenation and further as a conduit for endotracheal intubation.Various techniques have been described for the same, of which the highest success rates have been obtained by using a flexible fiber-optic bronchoscope inserted through an already placed LMA.[9]Other techniques,such as blind bougie insertion or the use of intubation guides (airway exchange catheters -Cook medical®;Cook Medical LLC®, USA) via SADs, have had just approximately 50% first-pass success rates.[10,11]The use of ultrasound as a guide for bougie placement has been previously described in pediatric patients with anticipated difficult airways.[12]The nonavailability of fiber optic bronchoscope and obscured visibility led us to use this novel combination of adjuncts for management of the difficult airway.ILMA is another alternative that has been used in obese patients with a reasonable success rate.[13]However, studies have shown that the first-pass success with blind intubation with ILMA is up to 90%,which reduces further in novice users; there may be up to 8% risk of esophageal intubation with the blind technique.[14,15]The time taken for tracheal intubation and maneuvers may be significantly longer when using conventional polyvinylchloride tracheal tubes with ILMA.These may be the perceived advantages when considering the L-B-US technique described by us,where the risk of esophageal intubation may be avoided.However, further study in a larger cohort is required to test the ease of use, learning curve and time to intubation using this technique.
CONCLUSIONS
This report highlights the use of a combination of a simple LMA, bougie, and ultrasound for effective preoxygenation and safe intubation in morbidly obese patients with a difficult airway.The technique utilizes existing equipment available in most EDs.
Funding:None.
Ethical approval:The Institutional Ethics Committee provided waiver of consent for case reports with no direct patient identifiers.Conflicts of interest: The authors have no Conflicts of interest.
Contributors:RB: conceptualization, writing original draft; PY:draft writing; JB: case image acquisition; AN: conceptualization,collecting case data; SKN: review of draft, intellectual inputs;PRM: review of draft.
All the supplementary files in this paper are available at http://wjem.com.cn.
 World journal of emergency medicine2023年3期
World journal of emergency medicine2023年3期
- World journal of emergency medicine的其它文章
- A 94-year-old patient with severe burns: a case report
- Pregnancy-related spontaneous coronary artery dissection after intravenous ritodrine infusion: a case report
- Twelve family members with tetramine poisoning after consumption of vegetables grown in polluted soils
- Resuscitative endovascular balloon occlusion of the aorta in the treatment of severe hemorrhagic shock caused by upper gastrointestinal bleeding
- A rare case of purulent pericarditis secondary to subdiaphragmatic abscess
- Factors associated with the clinical outcomes of adult cardiac and non-cardiac origin cardiac arrest in emergency departments: a nationwide retrospective cohort study from China
