Pregnancy-related spontaneous coronary artery dissection after intravenous ritodrine infusion: a case report
Ya-qing An, Yan-ling Dong, Yi-jiao Men, Liang Liu, Yu Gong, Jian-ling Su, Heng-bo Gao, Ying-ping Tian
Emergency Department, the Second Hospital of Hebei Medical University, Shijiazhuang 050051, China
Ritodrine hydrochloride (ritodrine) is a β2-adrenoceptor stimulant that has been effectively prescribed for the prevention of premature labor.[1]In clinical practice, one of the biggest drawbacks of β-mimetics is their adverse Effects, including arrhythmias,myocardial ischemia, and pulmonary edema, due to their β-sympathomimetic effects.[2]Here, we report a rare pregnant case of spontaneous coronary artery dissection(SCAD) after intravenous infusion of ritodrine.
CASE
A 29-year-old woman visited the local hospital at gestational age of 32 weeks and 3 days with frequent uterine contractions for 2 d.She was in good general health with no abnormalities in regular obstetric examinations or family history of genetic diseases.Physical examination and obstetrical ultrasound showed that her cervix was shortened, and irregular contractions were observed during fetal heart rate monitoring.In addition, myocardial enzyme, troponin, brain natriuretic peptide (BNP),electrocardiogram (ECG), and echocardiography on admission were normal.Subsequently, she only received intravenous infusion of ritodrine to inhibit uterine contraction.The initial dose of ritodine was 100 μg/min,increased by 50 μg per 10 min, and finally maintained at 250 μg/min.After 3 h of ritodrine infusion, the patient developed chest tightness and chest pain, and myocardial enzyme, troponin, BNP, ECG and echocardiography were immediately tested (these results were normal).Then,the ritodine dose was reduced to 100 μg/min, and these symptoms were relieved, with stable blood pressure and heart rate 90–100 beats/min.After the disappearance of chest pain, ritodrine was gradually increased to 250 μg/min, as she still had contractions.Chest tightness and chest pain occurred again after 30 min of infusion at 250 μg/min.After reducing the dose to 100 μg/min, the symptoms were relieved and tolerable.After maintaining this dose for 2 h, the patient suddenly developed severe chest pain and radiated to the left upper limb, left shoulder, and left back.The ritodrine infusion was immediately stopped, and her chest pain and radiation pain were relieved.ECG showed acute anterior myocardial infarction (MI).The patient was then transferred to our hospital.
An ECG re-examination at our hospital showed sinus rhythm, ST-segment elevation in leads V1 to V6, and T wave inversion in leads V1 to V5 (Figure 1A).Laboratory tests showed that creatine kinase (CK) was 1,628 U/L (normal range 18–198 U/L), creatine kinase isoenzyme (CK-MB)162 U/L (normal range <20 U/L), myoglobin 133 mg/L(normal range 10–70 mg/L), and troponin 34.996 ng/mL(normal range 0–0.020 ng/mL).Other serum biochemical indexes were normal.Transthoracic echocardiography showed that her left ventricular wall had abnormal phasic motion (Figures 1 B, C).Based on these findings, her initial diagnosis was suspected to be acute extensive anterior ST-elevation MI.After multidisciplinary consultation and discussion, she received a cesarean section on the second day after admission.Later, coronary angiography(CAG) and optical coherence tomography (OCT) were performed on the 7thday after admission.The CAG revealed approximately 60% eccentric stenosis in the middle of the left anterior descending (LAD) branch and approximately 80% localized stenosis in the distal segment with a linear spontaneous dissection obturating the true arterial lumen (Figures 2 A, B).OCT showed distal intimal detachment of the LAD, accompanied by intramural hematoma, thrombus, and a few fibrous plaques (Figures 2 C, D).On the 8thday after admission,she was discharged home and took 90 mg of tegrenol orally twice a day for 12 months, 75 mg of aspirin, and 2.5 mg of bisoprolol once a day.At 6 months of followup, she was clinically asymptomatic and refused further consultation.
DISCUSSION
SCAD is an acute noniatrogenic tear in the coronary arterial wall, leading to disruption of coronary blood f low and MI.[3]SCAD is an uncommon but increasingly recognized cause of acute MI among young and middle-aged women and is an important cause of pregnancy-associated MI.Pregnancyrelated SCAD (P-SCAD) accounts for <5% of SCAD cases.[4]Ritodrine is a selective β2 receptor agonist that strongly inhibits uterine contractions and is widely used clinically to prevent preterm birth.[5]A previous study found that the incidence of adverse reactions in ritozine tablets was approximately 3.9%,and in injections, it was approximately 18.3%.[5]
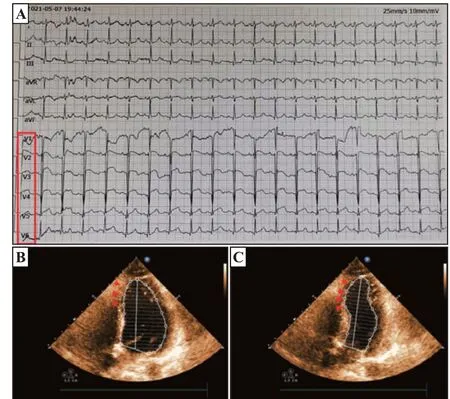
Figure 1.Examination at our hospital.A: admission ECG; B, C:transthoracic echocardiography showed segmental weakening of left ventricular wall motion (arrows).
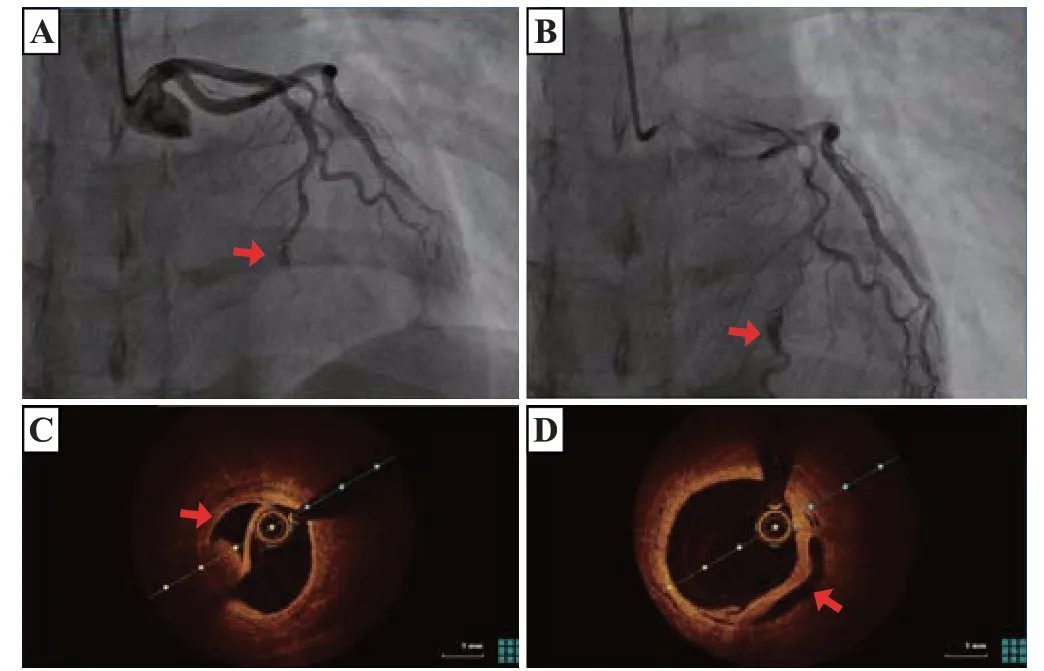
Figure 2.Images of CAG and OCT.A, B: CAG showed an intimal tear(A, arrow) with persistent distal filling defects and a linear dissection (B,arrow) in the distal segment of LAD with false lumen filled with contrast agent; C, D: OCT indicated distal intimal detachment of LAD with intramural hematoma and thrombus (arrows).CAG: coronary angiography;OCT: optical coherence tomography; LAD: left anterior descending.
In this case, SCAD occurred after ritodrine infusion.The reason may be as follows: (1) after exclusion of other causes or triggers of SCAD during pregnancy, a clinically relevant fact was clearly observed, that is, SCAD-related symptoms disappeared with ritodrine withdrawal or dose reduction and recurred with dose increase; (2) the pathological changes in vascular wall structure related to progesterone in the third trimester of pregnancy could provide a prerequisite for the formation of dissection;[6]and (3) due to the relatively large dose of ritodrine used in the clinic to inhibit premature labor,ritodrine may have lost its β-receptor selectivity, leading to increased adverse cardiac effects such as increased cardiac output, stroke volume, or heart rate.
CONCLUSIONS
This case highlights that in addition to other previously reported complications, ritodrine may also cause SCAD.Therefore, we suggest that pregnant women should be cautious in using ritodrine.In addition, when acute coronary syndrome occurs in the context of environmental stress factors (such as ritodrine treatment), CAG and OCT should be performed for final diagnosis.
Funding:None.
Ethical approval:This study was approved by the Local Ethical Committee.Written informed consent for publication of their clinical details and clinical images was obtained from our patient.
Conflicts of interests: The authors declare no conflict of interest.
Contributors:YQA and YLD contributed equally to this work.All authors made a significant contribution to the work reported.
 World journal of emergency medicine2023年3期
World journal of emergency medicine2023年3期
- World journal of emergency medicine的其它文章
- A 94-year-old patient with severe burns: a case report
- Twelve family members with tetramine poisoning after consumption of vegetables grown in polluted soils
- Resuscitative endovascular balloon occlusion of the aorta in the treatment of severe hemorrhagic shock caused by upper gastrointestinal bleeding
- A rare case of purulent pericarditis secondary to subdiaphragmatic abscess
- Laryngeal mask airway bougie ultrasonography guided intubation in a morbidly obese patient with difficult airway
- Factors associated with the clinical outcomes of adult cardiac and non-cardiac origin cardiac arrest in emergency departments: a nationwide retrospective cohort study from China
