Factors associated with the clinical outcomes of adult cardiac and non-cardiac origin cardiac arrest in emergency departments: a nationwide retrospective cohort study from China
Yue-guo Wang, Cudjoe Obed, Yu-lan Wang, Feng-feng Deng, Shu-sheng Zhou, Yang-yang Fu, Jian Sun, Wenwen Wang,5, Jun Xu, Kui Jin
1 Department of Emergency Medicine, the First Affiliated Hospital of USTC, Division of Life Science and Medicine,University of Science and Technology of China, Hefei 230001, China
2 Department of Microbiology & Immunology, School of Medical Sciences, University of Cape Coast, Cape Coast 00233,Ghana
3 Department of Cardiovascular Medicine, Huangshan City People's Hospital, Huangshan 245000, China
4 Department of Emergency Medicine, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences &Peking Union Medical College, Beijing 100730, China
5 Graduate School of Bengbu Medical College, Bengbu 233000, China
Cardiac arrest (CA) is one of the most common causes of death.[1-3]Despite extensive studies on the management of CA, the global survival rate in adults is only approximately 7%, and 30-day survival is even less than 2% in China.[4]Some studies have shown that CA patients of cardiac and non-cardiac origin may differ in underlying diseases, clinical manifestations,and prognosis, which leads to differences in terms of the pathophysiological mechanism and treatment measure.[5,6]However, little is known about the risk factors in relation to the prognosis of CA across arrest etiologies.
METHODS
Study design and setting
This study was based on the secondary analysis of data obtained from the National Emergency Cardiac Arrest Treatment (NECAT) database, which was initiated by the Department of Emergency Medicine of Peking Union Medical College Hospital in 2013, and a total of 14 tertiary teaching hospitals in 7 provinces throughout China were included.The clinical trial registration number was CHICTR-NCT-01987245.
Study population
Data were entered electronically via a web-based platform (https://redcap.onfile.cn/) to create the national registry of patients suffering from CA in emergency departments.The present study included patients who presented with non-traumatic CA, time from collapse to initiation of cardiopulmonary resuscitation (CPR) >10 min, and patients who did not sign the “do-not-resuscitate(DNR)”order.Patients underwent CPR following the 2020 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.
Study endpoint
The primary endpoint of the study was the return of spontaneous circulation (ROSC) rate after CA, and the secondary endpoints included the 24-hour, 7-day, and 28-day survival of patients.Risk factors associated with ROSC were compared across arrest etiologies.
Statistical analysis
Continuous variables were expressed as the mean and standard deviation (SD) and analyzed by Student’st-test,and categorical variables were expressed as frequencies and percentages and analyzed using Chi-square test and Fisher's exact test.Mann-WhitneyU-test was used for data with unknown distribution.In the multivariable analysis, binary logistic regression models were applied to compare the rate of ROSC, 24-hour, 7-day, and 28-day survival rates after adjusting the potential confounding factors.Subgroup analysis was performed according to the patients’ROSC and compared the risk factors associated with ROSC in these two groups.For the predictors of the outcome deduced from the logistic model, an analysis of receiver operating characteristics (ROC)was carried out.The corresponding ROC curve was obtained and the area under curve (AUC) was estimated by means of a 95% confidence interval (95%CI).A two-tailed value ofP<0.05 was considered statistically significant.Analyses were performed using SPSS 22.0 software and GraphPad Prism 8.0 was used as a drawing tool.
RESULTS
Demographic data and resuscitation characteristics of patients
A total of 535 CA patients aged 18 years or older were finally enrolled in this study.Compared with cardiac origin CA (CCA) patients, demographic data including age (64.28±15.89 years vs.56.40±19.20 years), proportion of males (69.20% vs.59.50%), body weight (70 [60, 75] kg vs.65 [55, 73] kg), and proportion of body mass index (BMI) <25 kg/m2(72.07% vs.63.48%) were significantly lower in non-cardiac origin CA (NCCA) patients (P<0.05).During the resuscitation process, NCCA patients had significantly lower values of resuscitation time (41 [30, 66] min vs.52 [30, 78] min,P<0.05) and peripheral oxygen saturation (SpO2) (70%[53%, 85%] vs.74% [59%, 86%],P<0.05) than CCA patients (supplementary Table 1).
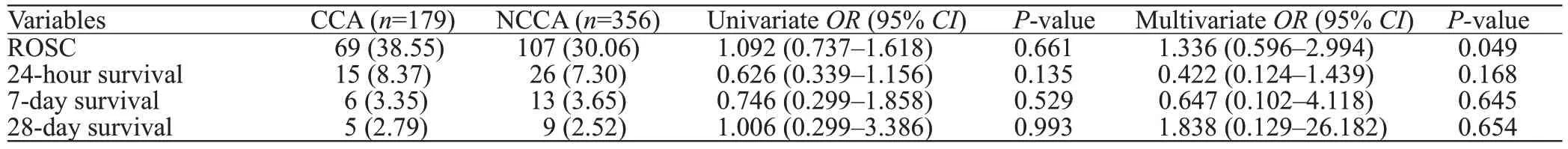
Table 1.The primary and secondary endpoints between CCA and NCCA patients
Endpoints of study patients
Our study suggested that more than 30% of CA patients,regardless of etiology, had ROSC (38.55% in those of cardiac origin and 30.06% in those of non-cardiac origin);however, the majority of ROSC patients did not survive the next 24 h (8.37% vs.7.30%).The 28-day survival rates in both groups were less than 3%.After adjusting for potential confounders such as age, sex, BMI, and underlying diseases including acute coronary syndrome (ACS), hypertension, and chronic obstructive pulmonary disease (COPD), with logistic regression, the primary and secondary endpoints of CCA showed no significant difference compared to those of NCCA(P>0.05) (Table 1 and supplementary Figure 1).
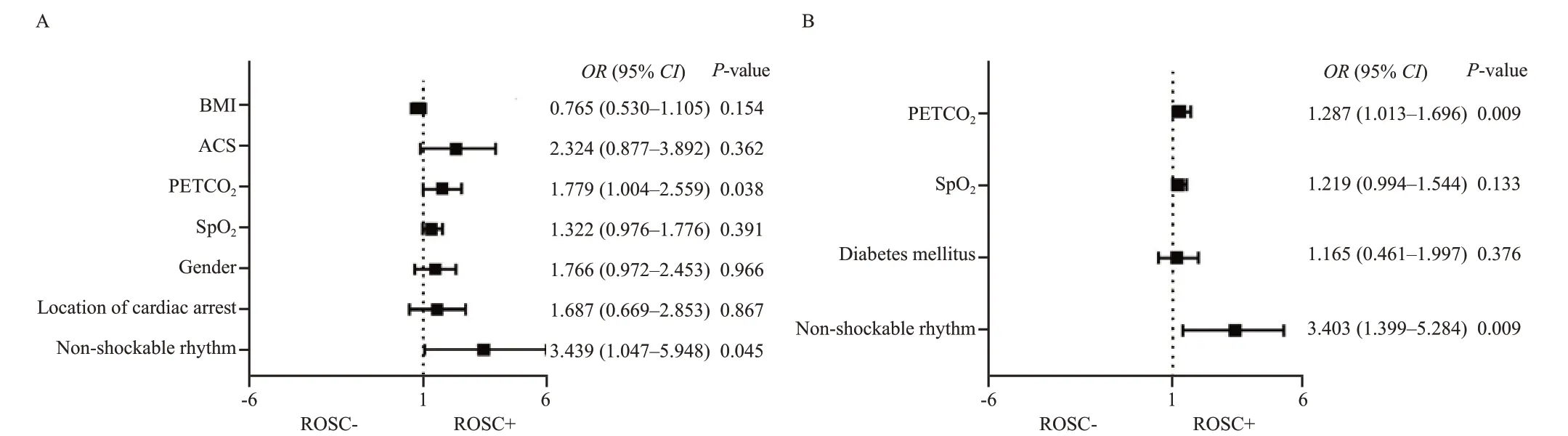
Figure 1.The OR and 95% CI for ROSC in ROSC+ compared with ROSC- in CCA (A) and NCCA (B) patients, stratified by variables associated with ROSC.BMI: body mass index; ACS: acute coronary syndrome; PETCO2: pressure of end-tidal CO2; SpO2: peripheral oxygen saturation; ROSC: return of spontaneous circulation; OR: odds ratio; CI: confidence interval.ROSC+: patients who achieved ROSC; ROSC-: patients who didn't achieve ROSC.
ROSC-related parameters of study patients
For patients with CCA, ROSC+ patients (patients who achieved ROSC) had a lower proportion of males (56.52%vs.73.64%), lower body weight, and BMI than ROSCpatients (patients who didn't achieve ROSC) (P<0.05).Patients with higher levels of SpO2(79% [67%, 97%] vs.71% [56%, 85%]) and pressure of end-tidal CO2(PETCO2)(20 [12, 33] mmHg vs.14 [8, 22] mmHg, 1 mmHg=0.133 kPa) had significantly higher chances to achieve ROSC(P<0.05).In addition, for patients with NCCA, ROSC+patients had a significantly lower proportion of nonshockable rhythm (63% vs.83%) and a higher proportion of diabetes mellitus (DM) (22% vs.14%) than ROSC- patients(P<0.05).The levels of SpO2and PETCO2in ROSC+patients were significantly higher than those in ROSCpatients (P<0.05) (supplementary Table 2).
Additionally, as shown in Figure 1, multivariate logisticregression analysis showed that PETCO2was independently associated with ROSC in both CCA (odds ratio [OR] 1.779,95%CI[1.004–2.559],P<0.05) and NCCA patients (OR1.287, 95%CI[1.013–1.696],P<0.05), suggesting that a low level of PETCO2was a risk factor for ROSC in CA patients.Moreover, the AUC of PETCO2in CCA patients was 0.732,while the cut-off was 18.5 mmHg, the sensitivity was 77.8%,and the specificity was 62.9%.Consistent with this, the AUC of PETCO2in NCCA patients was 0.673, and when the cut-off was 24.5 mmHg, the sensitivity was 46.7%, and the specificity was 83.1% (supplementary Figure 2).
DISCUSSION
Our data showed that the ROSC rate, the 24-hour and 28-day survival rates were higher in CCA patients than in NCCA patients.Factors including non-shockable rhythm,SpO2and PETCO2were associated with the incidence of ROSC in CA regardless of etiology, and PETCO2was an independent risk factor for ROSC in CA patients.
Interestingly, Stankovic et al[7]also indicated that initial non-shockable rhythm remained negatively associated with increased ROSC.In addition, we suggested that high levels of PETCO2and SpO2were associated with achieving ROSC in CA across etiologies.PETCO2acts as the primary physiological variable during CPR and shows a significant correlation with cardiac index, coronary perfusion pressure,and ROSC.[8,9]S pO2, as an indicator that reflects peripheral perfusion, is a vital parameter associated with a better 30-day neurological outcome of out-of-hospital cardiac arrest(OHCA).[10]Javaudin et al[10]indicated that SpO2≥94%was associated with a better prognosis in adult OHCA.Our data showed that for all causes of CA, the PETCO2and SpO2values in ROSC+ patients were significantly higher than those in ROSC- patients.Consistent with our study,Pearce et al[11]showed that initial PETCO2>20 mmHg was associated with ROSC among pulseless electrical activity(PEA) cardiopulmonary arrest patients, suggesting that initial PETCO2acts as a prognostic indicator during CPR.
Additionally, there were several limitations of this study.First, this study was a secondary analysis of data from the NECAT database and included a small number of patients.Although potential confounders were adjusted, the primary and secondary endpoints may still be affected by parameters that were not included.Second, the diagnosis of CCA and NCCA was entirely based on the judgment of clinicians due to a lack of reliable methods.Finally, patients included in this study suffered CA after admission to the emergency room,which may be different from the patients who experienced in-hospital cardiac arrest (IHCA) and OHCA.Attention should be given to the interpretation of the relevant research results.
Funding: Th is study was supported by the Doctoral Scientific Research Foundation of the First Affiliated Hospital of USTC(RC2021023) and Key Research and Development Plan of Anhui Province (S2022e07020194).
Ethical approval:This study was approved by the Ethics Committee of Peking Union Medical College Hospital, Beijing, China (Reference number: S-701).
Conflicts of interest: There are no Conflicts of interest.
Contributors: YGW proposed the study and wrote the paper.All authors contributed to the design and interpretation of the study.
All the supplementary files are available at http://wjem.com.cn.
 World journal of emergency medicine2023年3期
World journal of emergency medicine2023年3期
- World journal of emergency medicine的其它文章
- A 94-year-old patient with severe burns: a case report
- Pregnancy-related spontaneous coronary artery dissection after intravenous ritodrine infusion: a case report
- Twelve family members with tetramine poisoning after consumption of vegetables grown in polluted soils
- Resuscitative endovascular balloon occlusion of the aorta in the treatment of severe hemorrhagic shock caused by upper gastrointestinal bleeding
- A rare case of purulent pericarditis secondary to subdiaphragmatic abscess
- Laryngeal mask airway bougie ultrasonography guided intubation in a morbidly obese patient with difficult airway
