Age-appropriateness of decision for brain CT scan in elderly patients with mild traumatic brain injury
Kasamon Aramvanitch, Korawee Khachornwattanakul, Piraya Vichiensanth, Chetsadakon Jenpanitpong, Ponlawat Kanchayawong, Sorawich Watcharakitpaisan, Chaiyaporn Yuksen
Department of Emergency Medicine, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok 10400,Thailand
Traumatic brain injury (TBI) is a prevalent issue among patients presenting in emergency departments (EDs), with mild TBI being the most common form.[1,2]Mild TBI is characterized by symptoms such as loss of consciousness,amnesia, disorientation, or a Glasgow Coma Scale (GCS)score of 13–15.[3]Although most patients with mild TBI can be safely discharged, Yuksen et al[4]reported that about 14.12% of all mild TBI patients were found to be positive for intracranial hemorrhage on a head CT scan.Computed tomography (CT) scans are widely used as a diagnostic tool for TBI, as they provide a quick and reliable diagnosis.[5]
Clinical factors associated with an increased risk of intracranial bleeding on a CT scan include headache,altered consciousness, neurological deficits, posttraumatic vomiting and amnesia, and signs of skull or basilar skull fractures.[4,6]To determine the appropriate use of CT scans, various clinical guidelines have been evaluated, such as the Canadian CT Head Rules (CCHR),New Orleans Criteria (NOC), National Emergency X-ray Utilization Study II (NEXUS II), and the mild TBI risk score.[6]CCHR has a higher specificity (39.7% vs.5.6%),positive predictive value (PPV), and negative predictive value (NPV) than NOC.[7]
The global population is rapidly aging due to declining birth rates and increased life expectancy.By the year 2050, the proportion of older adults is projected to reach 21.1%.[8]TBI is common in this aging population, with falls being the most common cause.In older adults, there is a higher incidence of subdural and intraparenchymal hematomas due to decreased brain mass, increased stretching and tension of the bridging veins, and brain atrophy, which can allow blood accumulation without initial signs or symptoms.Age is considered a significant predictor of mild TBI.[9]However, guidelines for determining the cut-off age vary,with 65 years being used in the CCHR guideline and 60 years in the NOC guideline.[10]A small study in Canada found that using a cut-off age of 75 years in the CCHR criteria increases specificity while maintaining 100%sensitivity.[11]Therefore, the current cut-off age of 65 years may not be appropriate for this population in terms of screening for TBI.
Using CT scans to diagnose TBI can lead to increased healthcare costs, exposure to radiation for patients, and longer stays in the ED.This study aimed to evaluate the impact of age on the predictive capacity and usage of CT scans for diagnosing TBI in the elderly population.The primary outcome was to determine an appropriate cut-off age for the elderly population presenting with mild TBI.The secondary outcome was to identify the clinical factors that predict mild TBI on CT scans in older adults.
METHODS
Study design
This study was a retrospective, diagnostic, crosssectional study conducted at the Department of Emergency Medicine at Ramathibodi Hospital, a university-affiliated, super-tertiary care facility in Bangkok, Thailand.Data were collected from the hospital’s database and Emergency Medical Records,and informed consent was waived as the data were retrospectively collected and anonymous.The study was approved by the Faculty of Medicine’s Committee on Human Rights Related to Research Involving Human Subjects at Mahidol University’s Ramathibodi Hospital.
Participants and data collection
The study included patients who were over 60 years old and presented at the EDs with a complaint of mild TBI.Eligible criteria for the study included confirmed isolated mild TBI and a CT scan.Patients were excluded if they had a GCS score less than 13, did not have a brain CT scan, had a penetrating skull injury, had a focal neurological deficit, had a post-traumatic seizure, or were using anticoagulation medication.
The characteristics of patients were collected, and the principal diagnosis of the disease was determined using the International Classification of Disease, Tenth Revision Code (ICD-10) codes S099 (unspecified injury of head), S0000 (superficial injury of the scalp), and S0600 (concussion without an open intracranial wound).
Outcomes
The primary outcome of the study was to determine the accuracy of various age cut-offs for performing CT scans in elderly patients with mild TBI.The secondary outcome was to identify factors that predict mild TBI on CT scan in the elderly population.
Statistical analysis
Statistical analysis was performed using STATA version 14.0.Comparisons between the brain-positive CT and brain-negative CT patients using the exact probability test for categorical variables and Student’st-test for normally distributed continuous variables.The Wilcoxon rank sum test was used for non-normally distributed continuous variables.AP-value <0.05 was considered statistically significant.The predictive power of each variable was calculated using univariable and multivariable logistic regression and then presented as the area under the receiver operating characteristic(AUROC) curve with 95% confidence intervals (CIs).Discrimination of the predicted age was presented as sensitivity, specificity, and AUROC curve with 95%CIs for determining an appropriate age for receiving brain CT scan.
RESULTS
Between December 31, 2017, and January 1, 2020, 706 participants met the eligibility criteria.Of these, 63 patients were found to have brain injuries on CT scans.The overall baseline characteristics of the study population are presented in supplementary Table 1.Males represented 32.7% (n=231)of the total population, and the mean age was 76.8±9.4 years.The three most common causes of injuries were falling(88.7%), motor vehicle accidents (5.1%), and syncope(4.7%).The median time from injury to presentation at the EDs was 3 h, and the mean initial GCS score at presentation was 15.The percentage of the admission to the hospital was 1.7%, with mortality of 0.3%.
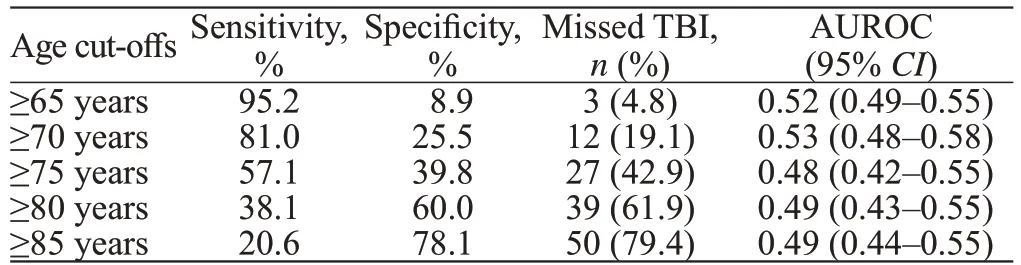
Table 1.Sensitivity, specificity, AUROC and missed acute brain injury on CT according to different age criteria in all elderly with mild TBI (n=706)
The sensitivity and specificity at different age cut-offs are presented in Table 1.The sensitivity of the 65-year-old cut-off was the highest at 95.2%, but the specificity increased from 65 years to 70 years (8.9 to 25.5).
The results of the univariable logistic regression analysis of clinical predictors are presented in Table 2.Of the 706 patients, 593 (84.0%) met only the age criteria (≥65 years).Patients who met the criterion of age and other clinical factors of CCHR had a significantly higherincidence of mild TBI than those who met only the age criteria alone (P<0.001).However, age cut-off s of 65 years or 70 years did not significantly predict mild TBI on CT scans (P=0.347 and 0.289).

Table 2.Univariable analysis of variables for acute brain injury, n (%)
In the multivariable logistic regression in supplementary Table 2, three independent clinical items significantly predicted positive CT scans: amnesia before impact of ≥30 min (odds ratio [OR] 3.83,P<0.001), vomiting ≥2 episodes(OR3.81,P=0.007), and headache (OR3.70,P=0.011).
A new model was developed, incorporating seven clinical factors: vomiting ≥2 episodes,amnesia before impact of ≥30 min, headache, use of antiplatelet medication, suspected fracture of the skull base, dangerous mechanism of injury, and loss of consciousness >5 min.
As shown in Table 3, the AUROC curve of the modified CCHR, which includes an age cut-off of 70 years, was not significantly different from that of the standard CCHR (AUROC 0.68, 95%CI0.61–0.75 vs.0.66, 95%CI0.60–0.73).However, the new CT Head Rule model we established has a higher AUROC (0.72,95%CI0.65–0.78) than the CCHR.
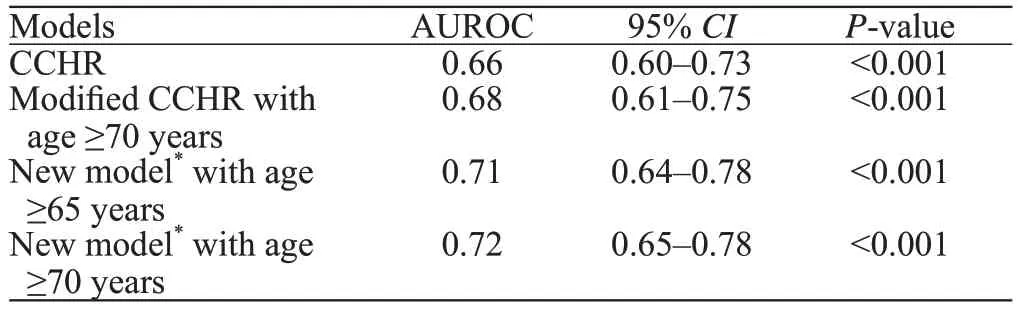
Table 3.Model of CCHR and a modified CCHR to age 70 years old
DISCUSSION
The incidence of mild TBI on CT scans in our study was 8.9%, corresponding with previous research on mild TBI (6%–10%).[3]As the CCHR mandates every patient aged ≥65 years to be tested regardless of their clinical state, this rule has been considered for its low specificity.
Our study demonstrates that age alone is not a reliable predictor of mild TBI.Unlike the previous study conducted in Canada, a modified version of the CCHR with a cut-off age of 75 years retained 100%sensitivity but increased specificity to 13.9%.[11]This can be explained by the fact that in older patients,physicians often cannot obtain an accurate history of the accident, and the mechanism of head injury in the elderly is typically low, with a rare loss of consciousness.Additionally, all previous studies were conducted in Western populations, while our study focused on Asians.Notably, we found that patients with more than onecriterion other than age were directly related to mild TBI.Therefore, elderly patients with mild TBI without other clinical factors could be safely discharged regardless of age.
The leading mechanism of injury among the elderly is falling, and a dangerous mechanism is associated with mild TBI.[12]Our study found that specific criteria, such as amnesia before impact of ≥30 min and vomiting ≥2 episodes, significantly predict mild TBI.In contrast to the CCHR criteria, our study shows that signs of skull base fracture or suspected depressed skull fracture are not associated with brain injury.[13,14]This discrepancy may be attributed to the small population size of our study and the fact that these signs are dependent on physician observation and can be similar to other signs,such as periocular ecchymosis.Additionally, we found that patients reporting headaches also predict brain injury on CT scans; this clinical item is not included in the CCHR criteria but is part of the New Orleans criteria.Furthermore,our study found that antiplatelet use, common among the elderly and a concern for physicians,[15]was associated with mild TBI in our study, which may be due to the small population size of our study.
In our study, we evaluated the performance of a new model that included eight clinical factors: age ≥65 years,dangerous mechanism of injury, vomiting ≥2 episodes,amnesia before impact of ≥30 min, loss of consciousness>5 min, headache, use of antiplatelet medication, and suspected fracture of the skull base.This new model demonstrated improved accuracy in predicting mild TBI,as measured by the AUROC (0.71), compared to the standard CCHR (AUROC 0.66).
We also found that none of the patients required surgical treatment.However, two patients passed away due to their decision to decline resuscitation or any invasive procedures.The admission rate was 1.7%,which is significantly lower than the rate reported in a previous study (8%).This difference can be attributed to the fact that our hospital is a tertiary care center, which allows patients to be observed overnight for neurological signs and to undergo follow-up CT scans in the ED.
This study has several limitations.First, it was a retrospective study, which may have resulted in missing data for some clinical items that were not recorded, and we treated them as absent.Additionally, we used ICD codes to enroll the population.Most patients in the study had an initial GCS of 15, which may not reflect the full spectrum of mild TBI in elderly individuals.Furthermore, certain factors, such as a GCS score <15 at 2 h after injury, were only present in a subgroup of mild TBI.Finally, the study only compared the results to the CCHR criteria.
CONCLUSIONS
The criterion of age alone does not accurately predict mild TBI.Using the CCHR with modified age criteria of 70 years old did not result in a significant difference compared to the standard CCHR.Elderly patients with mild TBI who do not have any other clinical factors could be safely discharged regardless of age.
When considering other clinical factors, such as use of antiplatelet medication, loss of consciousness >5 min,and the presence of headache in addition to the factors from the CCHR, this combination performed better in predicting mild TBI on CT scans.This approach could be safer and reduce unnecessary CT scans.
Funding:None.
Ethical approval:The study was approved by the Faculty of Medicine’s Committee on Human Rights Related to Research Involving Human Subjects at Mahidol University’s Ramathibodi Hospital.
Conflicts of interest: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributors:KA proposed the study and wrote the first draft.All authors contributed to the design and interpretation of the study and to further drafts.
 World journal of emergency medicine2023年3期
World journal of emergency medicine2023年3期
- World journal of emergency medicine的其它文章
- Most patients with non-hypertensive diseases at a critical care resuscitation unit require arterial pressure monitoring: a prospective observational study
- Over-expression of programmed death-ligand 1 and programmed death-1 on antigen-presenting cells as a predictor of organ dysfunction and mortality during early sepsis: a prospective cohort study
- Effects of continuous renal replacement therapy on inflammation-related anemia, iron metabolism and prognosis in sepsis patients with acute kidney injury
- Effects of early standardized enteral nutrition on preventing acute muscle loss in the acute exacerbation of chronic obstructive pulmonary disease patients with mechanical ventilation
- Development and validation of a predictive model for the assessment of potassium-lowering treatment among hyperkalemia patients
- The relationship between physical activity in early pregnancy and hypertensive disorders of pregnancy:a cohort study in Chinese women
