Effectiveness of resilience-promoting interventions in adolescents with diabetes mellitus: a systematic review and meta-analysis
Yi Wu · Yi-Yun Zhang · Ya-Ting Zhang · Hui-Jing Zhang · Tian-Xue Long · Qi Zhang ·Jing Huang · Ming-Zi Li
Abstract Background This study aimed to analyze the efficacy of resilience-promoting interventions among adolescents and youth aged 10-24 years with any type of diabetes.Methods A systematic literature search was performed using the PubMed,Web of Science,Embase,Cochrane Library,CINAHL,and PsycINFO databases from inception to May 25,2022.The Cochrane risk of bias tool (version 2) was used to assess the quality of the included studies.A meta-analysis was performed to calculate the pooled effects of resiliencepromoting interventions.Results Nineteen articles were included covering an overall sample of 2048 adolescents with diabetes.When analyzing the effectiveness of resilience-promoting interventions,hemoglobin A1c (HbA1c) at six months [mean difference=-0.47,95% confidence interval (CI)=-0.83 to -0.12,P =0.009] after the intervention was improved.However,long-term(≥ 12 months) improvement in HbA1c was not significant.In addition,comparing the control group,there were significant differences in the effect size for stress [standardized mean difference (SMD)=-0.87,95% CI=-1.25 to -0.48,P < 0.05],self-efficacy (SMD=0.50,95% CI=0.02-0.98,P =0.04) and quality of life (SMD=0.27,95% CI=0.03-0.51,P =0.03).Conclusions Resilience-promoting intervention is a promising way for adolescent diabetes management to improve HbA1c,stress,self-efficacy,and quality of life.Incorporating resilience-promoting components into diabetes education and reenforcing these contents every six months are recommended for implementation in clinical practice.
Keywords Adolescents · Diabetes mellitus · Intervention · Meta-analysis · Resilience
Introduction
Diabetes mellitus (DM),especially type 1,is the most common endocrine-metabolic disorder in adolescence [1].According to the 10th edition of the International Diabetes Federation Diabetes Atlas,globally,there were 1.2 million people aged 0-19 with type 1 diabetes (T1DM) in 2021 [2].Although the type of diabetes in adolescents is mainly type 1,the number of adolescents with type 2 diabetes (T2DM)cannot be ignored [3,4].A review of the incidence of T2DM in children and adolescents found that there were approximately 41,600 new cases of diagnosed T2DM among children and adolescents in 2021 worldwide [5].Adolescence is a period of intense physiological,psychological,and social change [6].In addition to the developmental challenges during adolescence,care and close supervision of diabetes management are increasingly shifted from parents and other primary caregivers to youth with T1DM or T2DM throughout adolescence [1].The American Diabetes Association guidelines mention the need for interventions to help adolescents with diabetes adapt to their self-management responsibilities[1].Sustaining these self-management behaviors and mental health can be challenging for young people.Research has suggested that self-care behaviors during this critical period may set the stage for enduring adult health outcomes [7,8].

Fig.1 Mechanism of resilience intervention
However,deteriorating glycemic control is common in adolescence and is associated with more complications and higher mortality in adulthood.Research evidence has shown that many adolescents experience declines in diabetes self-management behaviors and worsening glycemic control,as indicated by increases in hemoglobin A1c (HbA1c) [9,10].Globally,only 17%-22% of adolescents with T1DM currently meet glycemic targets [1,11,12].Again,evidence from SEARCH,an observational longitudinal study of youth with diabetes diagnosed before the age of 20 years in the United States,showed that the mean HbA1c of youth with T2DM changed from 7.3%within the first year of diagnosis to 8.8% five years later,which is similar to the trajectory of glucose deterioration in patients with T1DM [13].Since diabetes is a disease that requires life-long management,when blood glucose control is sub-optimal in adolescence,a series of complications will occur in adulthood,such as hypertension,nephropathy,retinopathy,and neuropathy [1].In addition to physical illnesses,after receiving a diagnosis,youth might experience high levels of mental distress,and some report feeling isolated,having a sense of grieving for their former lives,or having trouble accepting the diagnosis[14].As the coronavirus disease 2019 (COVID-19) pandemic spreads around the world,the psychological health of adolescents,especially those with chronic diseases,is getting worse [15].In turn,adverse psychological problems can make adolescents slack in diabetes self-management.This vicious cycle poses enormous challenges to the management of diabetes.Despite significant challenges,some resilient teenagers are able to comply with recommended diabetes care behaviors,achieve glycemic targets,and experience less distress [16,17].
Resilience has been broadly regarded as the ability to overcome or rebound from adversity [18-20].Resilience refers to protective skills and assets that contribute to great health and psychological outcomes when exposed to adversity [16].According to Hilliard's diabetes resilience model (this model describes the resilience process that leads to health outcomes in patients with diabetes),aspects of behavioral resilience in diabetes (e.g.,more frequent blood glucose monitoring) influence aspects of health resilience (e.g.,HbA1c within the target range)[16].The results from observational studies also showed that better psychological resilience could improve blood glycemic control by promoting self-management behaviors in adolescents with T1DM or T2DM [21,22].Reviews have identified that an individual's resilience is malleable,with resilience improving following resilience-promoting training [23,24].Resilience-promoting intervention has been primarily developed as therapeutic for individuals with clinical symptoms or preventive for healthy or at-risk populations [25].Figure 1 shows the mechanism of resilience training for promoting resilience from the American Psychological Association (APA)'s handbook[20,25].Several existing resilience-based interventions have largely situated their training on psychosocial factors,targeting the personal and relational levels [2,20,26].Being diagnosed with diabetes is a major adverse condition for teens throughout adolescence.Although the type of diabetes varies,adolescents all need to engage in similar disease management behaviors,such as maintaining a healthy diet,regular outpatient follow-up,daily blood glucose monitoring,and taking medications or insulin as prescribed,to achieve glycemic control goals when they face the adversity of diabetes.Accordingly,it is necessary to improve the psychological resilience of adolescents with diabetes through resilience training.Guidelines also recommend resilience interventions for adolescents with diabetes [27].
To date,some resiliency-promoting programs have been developed to help adolescents with diabetes improve their psychosocial well-being as a key factor in improving their overall health [28-31].However,the results of these interventions in improving patient health-related outcomes have been unstable.Some studies showed that these interventions could improve HbA1c [28,32-34],but other studies confirmed that the improvement in HbA1c was not significant [35-37].It is well-known that HbA1c is the standard indicative variable for blood glucose control.Thus,it is necessary to further quantitatively synthesize the available evidence.After reviewing the literature,we did not find any systematic review of interventions for resilience promotion in adolescents with diabetes.Thus,there remains a gap in the effectiveness of resilience-promoting interventions for adolescents with diabetes.Taking what is aforementioned into consideration,we conducted this meta-analysis of randomized controlled trials (RCTs) to evaluate the effectiveness of resilience-promoting interventions in adolescents with diabetes.
Methods
We designed and conducted this systematic review according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) [38].The protocol of this study was recorded in PROSPERO (No.CRD42022345189).
Search strategies and sources
To capture all eligible studies,we systematically searched PubMed,Web of Science,Embase,Cochrane Library,CINAHL,and PsycINFO from their inception to May 25,2022.A combination of medical subheading (MeSH) terms was used to develop the search procedure,including resilience,intervention,adolescent,and diabetes mellitus (Supplementary Table 1).The reviewers developed the search parameters for one database,which was later modified for all other databases.Two researchers (WY and ZYY) independently completed the literature search,and discrepancies were resolved by a third researcher (LMZ).We also conducted a hand-search of the reference list for potential missing eligible studies.
Eligibility criteria
We used the PICOS (Population,Intervention/issue of interest,Comparison,Outcome,and Study design) system to frame the inclusion and exclusion criteria [39].We included all studies in which (1) the inclusion of people was aged 10-24 years adolescents and youth with any type of DM;(2) interventions were designed based on the components of resilience intervention recommended by the APA [25],such as problem-solving,coping skills,self-regulation,and cognitive flexibility;(3) the reporting of clinical outcomes included HbA1c,quality of life,self-efficacy,diabetes distress,depression,anxiety,and stress;(4) the study design was an RCT;and (5) the study was published in the English and Chinese languages.Exclusion criteria included (1) conference proceedings,guidelines,dissertations,commentaries,reviews,animal model studies,and letters;(2) articles for which there was no full text or raw data;and (3) protocol and pilot studies.
Data extraction
The data extraction was performed by the same two independent authors (WY and ZYY) using a self-designed Excel spreadsheet.This predesigned data extraction spreadsheet summarizing information about study characteristics (first author,year,study design),participant characteristics,intervention characteristics,comparison characteristics,and outcome measures (outcomes,follow-up time point,and measurement tools) was employed for all included studies.
Critical appraisal
The Cochrane Risk of Bias Tool (RoB) 2.0 was used to assess the quality of the included studies [40].The following domains were assessed: randomization process,deviations from intended interventions,missing outcome data,measurement of the outcome,and selection of the reporting results.Response options from low risk of bias,some concerns to high risk of bias.The study showed low bias only when all the domains were judged to have a low risk of bias.Two researchers (WY and ZYY) independently assessed the RoB.After the independent evaluation by the two researchers,we discussed and consulted with the third researcher(LMZ) about the questionable results.
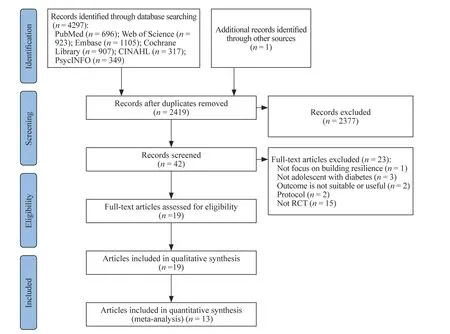
Fig.2 Flow diagram of the study selection process based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses statements. RCT randomized controlled trial
Statistical analysis
Meta-analysis was conducted using Review Manager software (Version 5.4.The Cochrane Collaboration,2020).For HbA1c,we calculated the mean difference(MD) and 95% confidence intervals (CI).Considering that the outcomes (such as self-efficacy,quality of life,diabetes distress,etc.) were measured with different validated scales,we calculated the standardized mean difference (SMD) and 95% CI.APvalue < 0.05 was considered to be statistically significant.Statistical heterogeneity was estimated usingPvalue andI2tests.P≤ 0.05 orI2≥ 50% was considered heterogeneous,and random effects models were used for statistical analysis.P≥ 0.05 andI2≤ 50% were considered not heterogeneous,and fixed effects models were used.We conducted a sensitivity analysis to test the reliability and stability of the results by excluding the included studies one by one and then recalculating the combined effects of the remaining studies.Considering the duration of the intervention effect,we performed different analyses by follow-up time point.We did not perform the publication bias assessment in this review because the number of included studies was small.
Results
Search results
According to the search strategies,4297 articles were initially obtained.After excluding duplicate articles,we screened 2418 articles for titles and abstracts.After an initial screening,the remaining 41 published studies were screened by full text;23 were excluded after the screening of the full text (reasons outlined in Fig. 2).The remaining 18 articles met our eligibility criteria [28-35,37,41-49].In addition,according to the manual search,we found one eligible article[36].Finally,nineteen articles (describing 17 studies) were included in this review (Fig. 2).
Study characteristics
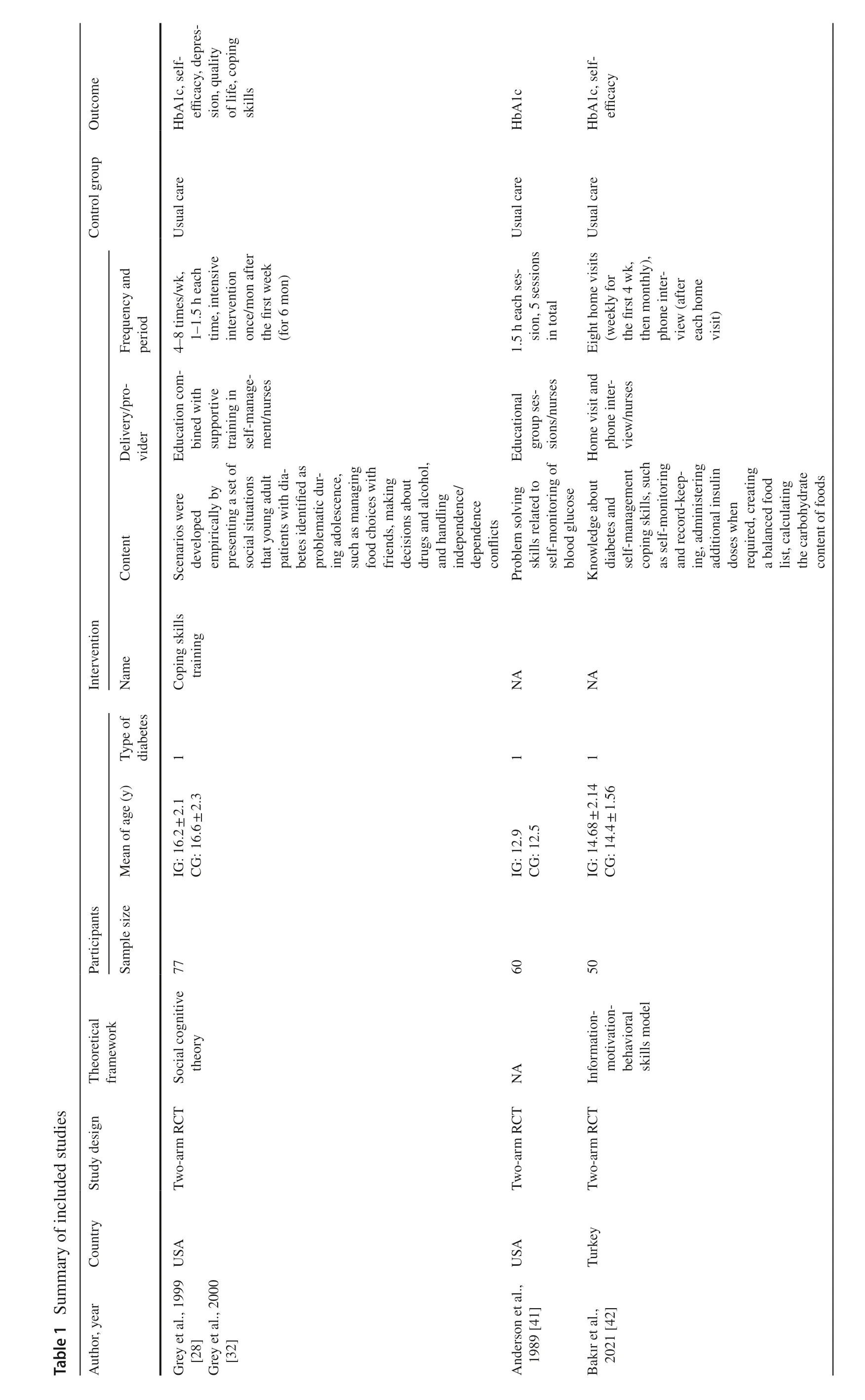




All 19 articles included in this review described 17 RCT studies.Table 1 summarizes the characteristics of the 17 studies.Nine studies were conducted in the US,two studies were conducted in the UK,and one study each was conducted in Turkey,Sweden,Iran,China,Canada,and Australia.A total of 2048 adolescents with diabetes were included in the final analysis.T1DM was primarily targeted in the included studies (16 studies).The mean ages of the participants ranged from 12-23.3 years.Eight studies followed the theoretical framework at the design stage.The most commonly used theoretical framework is social cognitive theory (n=4).For the characteristics of the intervention,the main form of intervention was face-to-face educational sessions (n=12),and two studies used interviews [42,46].Only three studies used online or remote interventions [35,36,45].The most common frequency of intervention was once a week (n=6).The intervention providers were nurses and psychologists (n=11),endocrinologists (n=4),and researchers (n=3),
Critical appraisal
The RoB results are presented in Supplementary Figs.1 and 2.The quality of the included studies was variable,and 12 of them had some concerns about the overall risk of bias[28-32,36,37,44,46-49],while two each had low [33,34]and five had a high risk of bias [35,41-43,45].Because such interventions cannot be blinded to participants,all of the studies we assessed had a low risk of bias in the blinding of participants.In addition,most studies had a low risk of bias in the measurement of outcomes and selection of reported results.The most common methodological limitations were the lack of a detailed description of the randomization and allocation concealment process and the inappropriate handling of missing data.
The components of resilience interventions and the measurement of resilience
Regarding the components of resilience-promoting interventions,training in problem solving is the most commonly reported component (n=16),and only one study did not consider problem solving as the component of the intervention [46].Other common components include self-regulation and coping (n=10) [17,28-30,34-36,42,44,48];cognitive flexibility (n=8) [17,28,30,36,42,44,48,49];building relationships (n=8) [17,28,29,33-36,44];and self-effi-cacy (n=5) [33,42-44,46].Only Bisno et al.'s study used resilience as an outcome measure,and the measuring tool is “The Diabetes Strengths and Resilience Scale (DSTARTeen)” [35].
Meta-analysis
Hemoglobin A1c
Thirteen studies reported HbA1c that could be used for integrated analysis [28,30,32-36,41-43,46-49].Considering the persistent effect of interventions on HbA1c,we performed an analysis of HbA1c at different follow-up time points.Figure 3 shows the effectiveness of promoting resilience intervention on HbA1c.The meta-analysis revealed a statistically significant difference in the pooled MD at 6 months (MD=-0.47,95% CI=-0.83 to -0.12,Z=2.62,P=0.009).However,there was moderate heterogeneity (I2=60%,P=0.02) between studies.Sensitivity analysis pointed to Bakır et al.'s study [42]as an outlier that potentially may have biased the effect size and heterogeneity,so further analysis excluding this study was performed.In the meta-analysis without outliers,the 6-month result was still statistically significant with little heterogeneity (MD=-0.30,95% CI=-0.55 to -0.05,Z=2.32,P=0.02,I2=18%,P=0.3) (Supplementary Fig.3).

Fig.3 Forest plot of the effectiveness of all resilience-promoting interventions on hemoglobin A1c. SD standard deviation,CI confidence interval

Fig.4 Forest plot of the effectiveness of promoting resilience intervention on psychological measurements. SMD standardized mean difference,SD standard deviation,CI confidence interval

Fig.5 Forest plot of the effectiveness of promoting resilience intervention on self-efficacy (a) and quality of life (b). SMD standardized mean difference,SD standard deviation,CI confidence interval
For the long-term effectiveness of HbA1c,the meta-analysis showed no statistically significant differences (Z=1.22 and 0.67,P=0.22 and 0.50,for 12 months and 18 months,respectively).Sensitivity analysis revealed that no individual study was able to change the results.
Psychological measurements
We analyzed measurements from four psychological outcomes (depression,anxiety,stress,diabetes distress)reported in seven studies (Fig. 4) [28,30,33-35,44,49].For depression,there was no statistically significant difference between the experimental and control groups(Z=1.69,P=0.09).However,when we excluded Wei et al.'s study [49],resilience-promoting interventions significantly improved depressive symptoms (SMD=-0.33,95% CI=-0.60 to -0.06,Z=2.4,P=0.02),although moderate heterogeneity existed between each study (I2=54%,P=0.07).In addition,although only two studies were included in the analysis,resilience-promoting interventions could significantly improve stress perception (SMD=-0.87,95% CI=-1.25 to -0.48,Z=4.40,P< 0.05),and there was no heterogeneity between studies(I2=0,P=0.39).
Self-efficacy
Six of the included studies examined the effects of resilience-promoting intervention on self-efficacy,including 407 participants made up of 204 in intervention groups and 203 in control groups [28,34,35,43,44,49].The combined effects reflected that the effect size was SMD=0.50,95% CI=0.02-0.98 (Z=2.03,P=0.04),which implied that resilience-promoting interventions could increase self-efficacy (Fig. 5 a).However,there was statistically significant heterogeneity in the combined studies (I 2=82%).Sensitivity analysis demonstrated that the result was stable.
Quality of life
Seven studies reported HbA1c that could be used for integrated analysis,including 828 participants made up of 413 in intervention groups and 415 in control groups [33-36,43,46,47].The meta-analysis revealed a statistically significant difference in pooled SMD on quality of life (SMD=0.27,95% CI=0.03-0.51,Z=2.2,P=0.03) (Fig. 5 b).Sensitivity analysis pointed to Brorsson et al.'s study [43] as an outlier that potentially may have biased the effect size and heterogeneity,so analysis excluding this study was performed.In the meta-analysis without outliers,the results showed that resilience-promoting interventions could significantly improve quality of life (SMD=0.17,95% CI=0.03-0.31,Z=2.36,P=0.02),and there was no heterogeneity between studies (I2=0,P=0.74).
Discussion
To our knowledge,the present study is the first systematic review and meta-analysis examining the effectiveness of resilience-promoting interventions on adolescents with diabetes.Finally,a total of 19 articles,including 17 studies,were included in the current study.This meta-analysis identified the meaning of resilience-promoting interventions for improving clinical health-related outcomes among adolescents with diabetes.It is worth noting that compared with the control group,these interventions significantly improved HbA1c within six months.In addition,improved stress,selfefficacy,and quality of life were also significant findings.Resilience-promoting intervention is a promising approach to the disease management of adolescents with diabetes.
According to our study,it is a meaningful result that resilience-promoting interventions could improve short-term(< 6 months) glycemic control for adolescents with diabetes.Glycemic control in adolescence has been a challenge in clinical diabetes management [50].During this period,in addition to the pubertal increase in insulin resistance,lack of adherence to therapeutic regimens,insufficient self-control,psychosocial factors,lack of family support and parental supervision,and incompetent transition from pediatric to adult care are also key causes of deteriorating glycemic control in teenagers [50].The mechanism of resiliencepromoting intervention (regarding resilience as a set of competencies) is mainly to build or improve the assets and protective factors of adolescents [16,25].For example,a key protective factor is self-efficacy or a belief in one's ability to influence certain aspects of his or her life.Adolescents learn through resilience-promoting interventions that allow them to better adapt to adversity and deal with other problems in their lives.Therefore,adolescents' treatment adherence,psychological problems,and diabetes self-management abilities could improve with resilience.After the analysis,it was surprising that,compared to the control group,the resilience-promoting intervention group changed HbA1c by -0.47 (95% CI=-0.83 to -0.12,Z=2.62,P=0.009)at 6 months.After removing an outlier,the heterogeneity almost disappeared,and the result was stable.Diabetes is a disease that requires life-long management for patients,and long-term glucose control is a crucial part.Although the currently available evidence does not support the longterm effect on HbA1c,given the characteristics of glycemic control in adolescence,we believe that the short-term effect is very significant in adolescents.Accordingly,for clinical diabetes practice,we strongly recommend incorporating resilience-promoting elements into daily diabetes education during adolescence and re-enforcing these contents every six months.Of course,due to the lack of long-term followup studies in this review,it is also recommended to extend the follow-up time when resilience-promoting interventions would be implemented in the future to explore long-term effects on HbA1c.
In this review,resilience-promoting interventions improved stress,self-efficacy,and quality of life.These results were expected.Self-efficacy is a key factor in social cognitive theory [51] and is defined as individuals' belief in their ability to establish motivational,cognitive,and behavioral resources to complete situational demands.Self-efficacy directly or indirectly affects the behaviors of people,their level of endurance against worries and failures,and the stress they face while dealing with environmental difficulties [52].Evidence has shown that people who have high levels of self-efficacy have to control their thoughts and show more stability,and self-efficacy could offer psychological resilience in achieving goals [53].For adolescents with diabetes,diabetes-specific self-management behaviors and glycemic control are also improved as self-efficacy increases [54].Studies have identified proactive orientation or self-efficacy (i.e.,taking initiative in one's own life and believing in one's own effectiveness) as a primary characteristic defining resilience [25].There is much evidence that resilience-promoting interventions can improve self-efficacy in adolescents [55-57].Through an increase in self-efficacy,teens become increasingly confident when dealing with adversity or challenges.As a result,the patient's negative emotions would decrease,and their quality of life would increase.A previous cross-sectional survey of patients with diabetes showed that increased self-efficacy could improve quality of life by improving negative emotions [58].Therefore,considering the above,we believe that the application of resilience-promoting interventions in adolescents with diabetes could effectively improve self-efficacy,quality of life,and some psychological measurements.However,due to insufficient evidence,it remains unclear which of the remaining psychological measurements could be significantly influenced by resilience-promoting interventions.
Apart from the above,we found that most of the included studies were conducted in economically developed Western countries.According to the handbook from the APA,resilience-based intervention must take into account different regional,national,and ethnic cultural contexts [25].Adolescents in low-and middle-income countries have worse glycemic control due to factors such as restricted access to insulin and inadequate diabetes education [50].We believe that it is necessary to carry out resilience-promoting programs in these areas.Therefore,the effectiveness of these developed interventions in low-and middle-income countries needs to be further validated.
Additionally,only three of the studies we included used online or remote interventions [35,36,45].All three studies included in this review showed that online or remote intervention did not worsen HbA1c compared with the control group [35,36,45],which indicated that online or remote interventions may be an alternative to face-to-face psychological support.Previous studies have reported that approximately 70%-80% of teens have turned to Internet sources for psychological health information or help with emotional problems [59,60],preferring privacy,easy access,and greater control over help-seeking afforded by virtual mental health care [61].Apart from the fact that almost all young people use the Internet [62,63],the emergence of the pandemic has made remote or online intervention a necessary means of health services.As the COVID-19 pandemic spreads around the world,economic hardship,diabetes educational needs,neurodevelopmental disorders,parental stress,and adolescent (especially those with chronic diseases) mental health are closely related [64,65].Research has shown that some young people appear to be less likely to bounce back as restrictions have eased,bringing further cause for concern [66].Hence,online or remote psychological interventions are very valuable programs for adolescents.Evidence indicates that online interventions can improve self-management and glycemic control in adolescents with diabetes [67-69].A systematic review found that digital resilience-based interventions could improve health-related outcomes for patients [20].Considering the above evidence,we believe that online resilience-promoting interventions would be effective.Considering the characteristics of the adolescent population,to better improve HbA1c,we suggest that future research develop an online format that is more appealing to these individuals,such as serious games and social platforms.
Based on our systematic review and meta-analysis,some implications for clinical practice and recommendations for further research are as follows.First,for clinical practice,we believe it makes sense to incorporate resilience-promoting elements into the management of adolescent diabetes and to repeat them over a period of time.Second,since the evidence in this paper is insufficient to support the long-term effect of these interventions on glycemic control,it is suggested that the follow-up time of RCTs should be extended in the future to observe the long-term effects of the interventions.Third,future research could examine which psychological measurements are sensitive to resilience-promoting intervention.Fourth,the intervention format can be made more attractive to adolescents,such as online serious games with more interactive elements.
Diabetes management in adolescence has always been a challenge in clinical practice.Complex factors not only lead to poor blood glucose control in adolescents but also bring about a series of mental health problems.Guidelines encourage routine screening and prevention of psychological problems in adolescents with diabetes [1,27].It is well proven that resilience-promoting intervention not only improved self-efficacy and stress but also improved glycemic control.Accordingly,the results of the current study contribute to clinical diabetes management by providing evidence on resilience-promoting interventions for improving short-term HbA1c,self-efficacy,and quality of life and indicate directions for future clinical practice and research on the management of diabetes in adolescence.
This review has several limitations.First,we searched only six large electronic databases and restricted our search to articles published in English and Chinese,which could lead to missing some relevant articles.Second,heterogeneity existed in some comparisons,and some of the included studies had low methodological quality.Third,due to the small number of included studies,we were unable to compare remote or online interventions with face-to-face forms of intervention,but that should be considered as a potential area of importance for future studies.Finally,in this review,we did not analyze the effects of resilience-promoting interventions in adolescents with different types of diabetes due to the limited number of studies included with T2DM.
In conclusion,resilience-promoting intervention is a promising method for the disease management of adolescents with diabetes.The present systematic review and meta-analysis provides evidence that resilience-promoting intervention could improve short-term HbA1c,stress,selfefficacy,and quality of life in adolescents with diabetes.However,current evidence is insufficient to demonstrate that these interventions improve long-term HbA1c levels.Incorporating resilience-promoting components into diabetes education in clinical practice and re-enforcing these contents every six months might improve glycemic outcomes,reduce complications and be the better transition to adult care in adolescents with diabetes.
Supplementary InformationThe online version contains supplementary material available at https:// doi.org/ 10.1007/ s12519-022-00666-7.
AcknowledgementsWe would like to thank faculty from Peking University Health Science Center for Evidence-Based Nursing,A Joanna Briggs Institute Affiliated Group,contributed to the editing of this article
Author contributionsWY contributed to the concept,search strategies,literature retrieval,discussion in the retrieval process and data extraction,critical appraisal,data analysis and interpretation,and revision to the original of manuscript.ZYY contributed to concept,search strategies,and literature retrieval,discussion in the retrieval process and data extraction.ZYT and ZHJ contributed to concept and search strategies.LTX and ZQ contributed to concept,literature retrieval,discussion in the retrieval process and data extraction,and critical appraisal,data analysis and interpretation.HJ contributed to concept,critical appraisal,data analysis and interpretation,and revision to the original of manuscript.LMZ contributed to concept,revision to the original of manuscript,and supervision of the study.WY and LMZ had full access to the data in the study and take responsibility for the integrity of the data and accuracy of the analysis.Manuscripts have been reviewed by all authors.The final manuscript version was confirmed by all authors.
FundingThis work was supported by the National Natural Science Foundation of China (No.72074008),King's College London-Peking University Health Science Center Joint Institute for Medical Research(No.BMU2021KCL003) and the Fundamental Research Funds for the Central Universities.
Data availabilityThe protocol can be accessed on PROSPERO (registration ID: CRD42022345189).Data can be accessed upon request by emailing the first author (jiyuanwuyi2@163.com).
Declarations
Ethical approvalEthical approval for this research was waived by its nature.
Conflict of interestNo financial or nonfinancial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.The authors have no conflict of interest to declare.
 World Journal of Pediatrics2023年4期
World Journal of Pediatrics2023年4期
- World Journal of Pediatrics的其它文章
- Effect of maternal pregestational diabetes mellitus on congenital heart diseases
- Psychiatric comorbidities in children and adolescents with chronic urticaria
- Addition of respiratory exercises to conventional rehabilitation for children and adolescents with cerebral palsy: a systematic review and meta-analysis
- Effects of synbiotic supplementation on anthropometric indices and body composition in overweight or obese children and adolescents: a randomized,double-blind,placebo-controlled clinical trial
- Estimated prevalence and trends in smoking among adolescents in South Korea,2005-2021: a nationwide serial study
- Factors of heavy social media use among 13-year-old adolescents on weekdays and weekends
