Addition of respiratory exercises to conventional rehabilitation for children and adolescents with cerebral palsy: a systematic review and meta-analysis
Thálita Raysa de Lima Crispim ·Mansueto Gomes Neto · Tafnes Rayane Lima Crispim ·Renivaldo Batista Dias · Maria Déborah Monteiro de Albuquerque · Micheli Bernardone Saquetto·Paulo André Freire Magalhães
Abstract Background Respiratory dysfunctions are an important cause of morbidity and death in cerebral palsy (CP) populations.Respiratory exercises in addition to conventional rehabilitation have been suggested to improve respiratory status in CP patients.The objective of this systematic review and meta-analysis was to verify the effects of the addition of respiratory exercises to conventional rehabilitation on pulmonary function,functional capacity,respiratory muscle strength,gross motor function and quality of life in children and adolescents with CP.Methods We searched for randomized controlled clinical trials in PubMed/Medline,Lilacs,SciELO,EMBASE and Physiotheraphy Evidence (PEDro) from their inception until July 2022 without language restrictions.Studies that included respiratory exercises (breathing exercise program;feedback respiratory training;incentive spirometer exercise;inspiratory muscle training;and combination of respiratory exercises+incentive spirometer exercise) in combination with conventional rehabilitation for children and adolescents with CP were evaluated by two independent reviewers.The mean difference (MD)and 95% confidence interval (CI) were estimated by random effect models.Results Ten studies met the eligibility criteria,including 324 children aged from 6 to 16 years.The meta-analysis showed an improvement in inspiratory muscle strength of 22.96 cmH2O (18.63-27.27,n =55) and pulmonary function of 0.60(0.38-0.82,n =98) for forced vital capacity (L);0.22 (0.06-0.39,n =98) for forced expiratory volume at 1 second (L);and 0.50 (0.05-0.04,n =98) for peak expiratory flow (L/min).Functional skills in daily living activities improved in the intervention group.Caregivers' assistance of daily living activities,functional capacity,gross motor function and expiratory muscle strength showed a nonsignificant improvement.Social well-being and acceptance and functioning domains improved in only one study.Conclusions Emerging data show significant enhancements in inspiratory muscle strength and pulmonary function in CP patients after respiratory training in addition to conventional rehabilitation.There is no consensus on the frequency,type or intensity of respiratory exercises for children with and adolescents with CP.
Keywords Breathing exercises · Cerebral palsy · Inspiratory muscle training · Pediatrics · Rehabilitation · Respiratory exercise
Introduction
Cerebral palsy (CP) describes a set of permanent disorders related to mobility and postural development,and these disorders can affect respiratory status [1].Recurrent aspiration,impaired airway clearance and lung function,spine and chest wall deformities,poor nutritional status and recurrent respiratory infections are the main causes of respiratory complications [2].Alarmingly,respiratory dysfunctions are an important cause of morbidity and death in CP populations[2,3].
Respiratory status is not directly affected by CP but due to secondary problems (e.g.,decreased physical activity level,scoliosis) [3].To better understand this context,Wang et al.[4] and Know and Lee [5] demonstrated that respiratory muscle strength in children with CP is lower than that in children with typical development and positively correlated with their capability levels of daily living,self-care and social function.In addition to respiratory muscle strength,another important concern is chest mobility.In contrast,children with CP commonly present restrictive pulmonary dysfunction due to reduced chest mobility,which can decrease lung expansion and compliance[6].The above-mentioned disorders can modify the respiratory breathing pattern,which leads from irregular breathing to respiratory failure,directly affecting overall daily needs and quality of life [4].These findings suggest that early initiation of respiratory exercises for children with CP should be considered,as it may improve and maintain chest mobility and respiratory function.
Pulmonary rehabilitation in children with chronic lung diseases has been extensively studied and points out protocols with respiratory exercises aimed at chest mobility and abdominal muscle strengthening,which lead to improved chest expansion and increased lower thoracic mobility,thus suggesting better diaphragmatic work and increased quality of life and exercise capacity [7-11].Some of these exercises were also proposed for children with CP [12,13].However,available rehabilitation strategies to target the respiratory functioning of the population with CP are not addressed in the literature;protocols are not standardized,and there is no consensus on the optimal training modalities.
Rehabilitation strategies in CP can include aerobic and/or breathing exercises.Aerobic exercises are commonly performed over a long period of time with light to moderate intensity (e.g.,running and cycling),limiting their application.Alternatively,respiratory exercises are increasingly regarded as an essential part of the overall physiotherapy in the management of CP and can be defined as techniques with or without the use of mechanical devices that encourage inspiration (e.g.,incentive spirometer) and expiration [e.g.,positive expiratory pressure (PEP)] [12,13].
Respiratory training has been proven to be a safe and effective behavioral intervention for the prevention and rehabilitation of chronic conditions,in which,despite presenting different pathophysiology from CP,also have restrictive mechanisms [9-11].However,evidence to date is scarce about the effectiveness of respiratory exercises in the population with CP [13].In view of the above,this systematic review and meta-analysis aimed to analyze published randomized controlled clinical trials (RCTs) that investigated the effect of the addition of respiratory exercises to conventional rehabilitation on pulmonary function,functional capacity,respiratory muscle strength,gross motor function and quality of life in children and adolescents with CP.
Methods
This systematic review was completed in accordance with Cochrane Collaboration recommendations and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines[14,15].The protocol of this review was registered in the PROSPERO international prospective register of systematic reviews (reference number: 219302).
This systematic review included articles classified as randomized controlled trials that studied the effects of any form of respiratory exercise in children and adolescents with CP.All studies should explicitly report that at least one of the treatment groups received the addition of respiratory exercise to conventional rehabilitation as an intervention.We excluded studies that included children and adolescents presenting other cardiac and pulmonary diseases associated with CP or adults.
The main outcomes were pulmonary function [forced vital capacity (FVC);forced expiratory volume at one second (FEV1);peak expiratory flow (PEF)];functional capacity [six-minute walk test (6MWT)];respiratory muscle strength [(maximum inspiratory pressure (Pimax)and maximum expiratory pressure (Pemax)];Gross motor function measure (GMFM),exercise capacity,daily living activities and quality of life were additional outcomes [Cerebral Palsy Quality of Life Questionnaire for Children (CP QOL-Child)].
We searched for literatures in the PubMed/Medline,Physiotherapy Evidence (PEDro),Scientific Electronic Library Online (SciELO),EMBASE,Latin American and Caribbean Literature in Health Sciences (Lilacs) databases from their inception until July 2022 without language restrictions.We used a standard protocol for literature search and controlled vocabulary whenever possible (DeCS/MeSH term for MEDLINE) [14].We used three groups of keywords and their synonyms in the search strategy: study design,participants,and interventions.
The strategy developed by Higgins and Green [14]was used to identify RCTs in PUBMED.The search strategy for MEDLINE via PUBMED is presented in Supplementary Table 1.We adopted a search strategy using similar terms to identify the RCTs in the other databases.We checked the references of the articles included in this systematic review to identify other potentially eligible studies.The authors of ongoing studies were contacted by e-mail to confirm any data or obtain additional information.

Table 1 Study quality on the PEDro scale






Two authors independently evaluated the list of titles and abstracts from each database.If at least one of the reviewers considered one study eligible,the full text was obtained for complete assessment.Then,two reviewers independently assessed the full text of the selected studies to verify whether they met the eligibility criteria.Two authors independently extracted data from the studies using standard data extraction forms adapted from the Cochrane Collaboration [14].
Aspects of the study population,forms of respiratory exercises,follow-up period and rates of missing data,outcome measures,and results were verified.The quality of the included studies was scored by two authors using the PEDro scale,which is based on important criteria such as concealed allocation,intention-to-treat analysis,and the adequacy of follow-up [16,17].These characteristics make the PEDro scale a useful tool for assessing the quality of rehabilitation of RCTs.A third reviewer resolved any disagreements in rating the studies.
Pooled effect estimates were obtained by comparing the least square mean change from baseline to endpoint for each group and were expressed as the mean difference (MD)between groups.We converted the confidence interval (CI)to standard deviation (SD) when the SD of change was not available,as per Higgins and Green [14].
Only data closest to the end points of the exercise program were included.Size effects in crossover trials were only extracted at the first crossover point.Only one comparison was made: respiratory exercise combined with conventional rehabilitation versus conventional rehabilitation.Calculations were performed using a random effects model.Heterogeneity among studies was examined with Cochran'sQandI2statistics,in which values greater than 40% were considered indicative of high heterogeneity [18].An α value ≤ 0.05 was considered statistically significant.Analyses were performed with Review Manager (Version 5.3) [19].
The quality of evidence for the outcomes pain and disability was assessed using the Grading of Recommendations Assessment,Development and Evaluation (GRADE)approach to interpret result findings and using GRADEpro GDT 2015 to import data from Review Manager to create a “Summary of findings table.” The assessment involved five items: risk of bias,imprecision,inconsistency,indirectness,and publication bias [14].The quality of evidence was downgraded by one level for risk of bias when more than a quarter of the studies included in the meta-analysis were considered at high risk of bias (studies without allocation concealment,random allocation,and/or sample size calculation).The results were considered imprecise if the pooled sample size was < 300 for dichotomous or < 400 for continuous outcomes and inconsistent if the heterogeneity between RCTs was substantial (i.e.,I2> 40%).When possible,publication bias was assessed by visual inspection of funnel plots (scatterplot of the effect size from individual studies against its effect size) for the meta-analysis with 10 or more trials [14,20].Decisions to downgrade the quality of studies were justified using footnotes and making comments,when necessary,to aid readers' understanding of the review.
Results
The initial research led to the identification of 195 studies,of which 181 studies were excluded based on the initial screening of the title and abstract,and 14 were considered potentially relevant and then retrieved for detailed analysis.Ten RCTs met the eligibility criteria and were included(Fig. 1) [21-30].The ten randomized controlled trials were fully analyzed and approved by both reviewers,and the data were extracted.The mean quality of the studies was low-tomoderate (Table 1).After assessing methodological aspects with the PEDro scale tool,we found that all of the studies used random allocation,and only four studies performed concealed allocation [23,24,26,29].None of the studies blinded the patients or therapists,and only three studies blinded the assessors [23,24,29].None of the studies used the principle of intention-to-treat analysis.
The characteristics of the randomized controlled trials are summarized in Table 2.The number of participants in the included studies was 324 children and adolescents.The age of participants ranged from 6 to 18 years [21-30].Randomized clinical trials included children and adolescents of both sexes.
The respiratory exercises differed between studies;the duration of programs ranged from four to eight weeks and were considered to be a combination of eight respiratory exercises called the “breathing exercise program”,feedback respiratory training,incentive spirometer exercise,inspiratory muscle training (IMT) with a threshold device,and a combination of respiratory exercises and incentive spirometer exercise [21-30].

Fig.1 Flow diagram of included studies
The main outcomes analyzed in the included studies were pulmonary function (FVC,FEV1,and PEF);functional capacity (6MWT);respiratory muscle strength (Pimax and Pemax),GMFM,daily living activities and quality of life[CP QOL-Child,and Pediatric Quality of Life Inventory(PedsQL)].
The posology used was reported in most studies.There was a variation regarding the session time from 5-7 minutes [21] to 15 minutes [23,25].The frequency of the sessions ranged from two times a week in one study [22],three times a week in another study [23],five times a week in one study [25],and seven times a week in two studies [21,24].The characteristics of respiratory exercise intervention in the included studies are provided in Table 3.
Respiratory exercise plus conventional rehabilitation versus conventional rehabilitation
Pulmonary function
Totally eight studies evaluated FCV [22-28,30].Metaanalysis was performed by grouping studies that evaluated the results in liters and % in the assessment of FVC.The meta-analysis showed a pooled effect of 0.60 L (95% CI 0.38-0.82,n=98,P< 0.001) and a significant effect of 5.2(% of predicted,95% CI 0.2-10.2,n=243,P=0.040) for respiratory exercise plus conventional rehabilitation group participants compared with the usual care group (Fig.2 a,b,respectively).
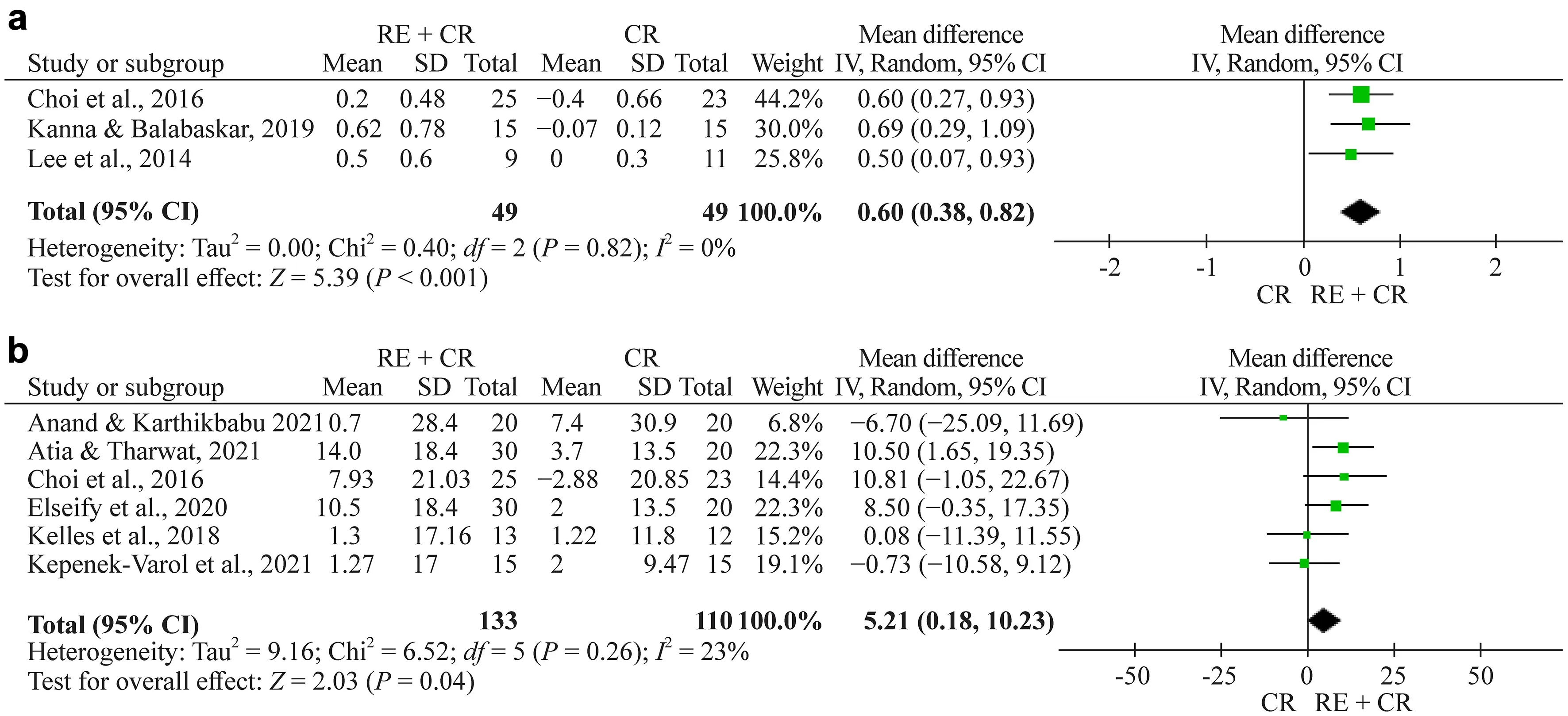
Fig.2 a Forest plot of FVC (forced vital capacity) (L) after respiratory exercise plus conventional rehabilitation versus conventional rehabilitation. b Forest plot of FVC (%) (L) after respiratory exercise plus conventional rehabilitation versus conventional rehabilitation.RE respiratory exercise,CR conventional rehabilitation,SD standard deviation,CI confidence interval

Fig.3 a Forest plot of FEV1 (forced expiratory volume at 1 s) (L)after respiratory exercise plus conventional rehabilitation versus conventional rehabilitation. b Forest plot of FEV1 (%) after respiratory exercise plus conventional rehabilitation versus conventional rehabilitation. RE respiratory exercise,CR conventional rehabilitation,SD standard deviation,CI confidence interval

Fig.4 a Forest plot of PEF (peak expiratory flow) (L/min) after respiratory exercise plus conventional rehabilitation versus conventional rehabilitation. b Forest plot of PEF (%) after respiratory exercise plus conventional rehabilitation versus conventional rehabilitation. RE respiratory exercise,CR conventional rehabilitation,SD standard deviation,CI confidence interval

Fig.5 Forest plot of functional capacity after respiratory exercise plus conventional rehabilitation versus conventional rehabilitation. RE respiratory exercise,CR conventional rehabilitation,SD standard deviation,CI confidence interval

Fig.6 Forest plot of Pimax (maximal inspiratory pressure) after respiratory exercise plus conventional rehabilitation versus conventional rehabilitation. RE respiratory exercise,CR conventional rehabilitation,SD standard deviation,CI confidence interval

Fig.7 Forest plot of Pemax (maximal expiratory pressure) after respiratory exercise plus conventional rehabilitation versus conventional rehabilitation. RE respiratory exercise,CR conventional rehabilitation,SD standard deviation,CI confidence interval

Fig.8 Forest plot of GMFM (Gross Motor Function Measure) after respiratory exercise plus conventional rehabilitation versus conventional rehabilitation. RE respiratory exercise,CR conventional rehabilitation,SD standard deviation,CI confidence interval
Totally eight studies evaluated FEV1 [22-28,30].Metaanalysis was performed by grouping studies that evaluated the results in liters and % in the assessment of FEV1.The meta-analysis showed a nonsignificant effect of 0.22 L (95% CI 0.06 to 0.39,n=98,P< 0.009) and a nonsignificant effect of 3.84 (% of predicted,95% CI -0.7 to 8.4,n=243,P=0.100) for the respiratory exercise plus conventional rehabilitation group participants compared with the conventional rehabilitation group (Fig. 3 a,b,respectively).
There are eight studies evaluating PEF [22-28,30].Metaanalysis was performed by grouping studies that evaluated the results in liters and % in the assessment of PEF.The meta-analysis showed a pooled effect of 0.50 (95% CI 0.05-0.04,n=98,P=0.030) in PEF (L/min) and a nonsignificant effect of 4.02 (% of predicted,95% CI -0.8 to 8.9,n=195) for the respiratory exercise plus conventional rehabilitation group participants compared with the conventional rehabilitation group (Fig. 4 a,b,respectively).
Functional capacity
Totally three studies evaluated functional capacity,all with the 6MWT [24,26,27].The total number of children and adolescents in the respiratory exercise plus conventional rehabilitation group was 48,whereas 47 children and adolescents were included in the conventional rehabilitation group.The meta-analysis showed a nonsignificant effect of 30.4 m(95% CI -5.2 to 68.9,n=95) for the respiratory exercise plus conventional rehabilitation group participants compared with the conventional rehabilitation group (Fig. 5).
Respiratory muscle strength
Totally four studies evaluated Pimax using manovacuometry [24,26,27,29].The total number of children and adolescents in the respiratory exercise plus conventional rehabilitation group was 60,whereas 61 children and adolescents were included in the conventional rehabilitation group.The meta-analysis showed a significant effect of 15.9 cmH2O (95% CI 3.3 to 28.5,n=121) for the respiratory exercise plus conventional rehabilitation group participants compared with the conventional rehabilitation group (Fig. 6).
There are four studies evaluating Pemax using manovacuometry [24,26,27,29].The total number of children and adolescents in the respiratory exercise plus conventional rehabilitation group was 61,whereas 60 children and adolescents were included in the conventional rehabilitation group.The meta-analysis showed a significant effect of 21.4 cmH2O (95% CI 1.01-41.7,n=121) for the respiratory exercise plus conventional rehabilitation group participants compared with the conventional rehabilitation group (Fig. 7).
Gross motor function measure (GMFM)
Totally two studies evaluated GMFM [22,29].The metaanalysis showed a nonsignificant effect of -1.8 (95%CI -10.9 to 7.3,n=74) for the respiratory exercise plus conventional rehabilitation group participants compared with the conventional rehabilitation group (Fig. 8).
Daily living activities
Kelles [24] assessed the effect of inspiratory muscle training on daily living activities.Daily living activities were assessed using the Pediatric Evaluation of Disability Inventory-Functional Skill Scale (PEDI-FSS) and Caregiver Assistance Scale (CAS).The PEDI-FSS self-care(1.86;95% CI 0.68-3.04;P=0.007),PEDI-FSS mobility(2.78;95% CI 1.72-3.84;P=0.001) and social function(3.95;95% CI 3.00-4.90;P=0.015) domain scores significantly improved in the treatment group compared with the control group.No difference was observed between the groups in the PEDI-CAS subscale scores.
Quality of life
Kelles [24] assessed the effect of inspiratory muscle training on the quality of life using CP QOL-Child.The CP QOLChild social well-being and acceptance (13.73,95% CI 12.86-14.60,P< 0.001) and functioning domain (5.09,95%CI 2.09 to 8.09;P=0.004) scores significantly improved in the treatment group compared with the control group.No difference was observed between the groups in the other domains of the CP QOL-Child.
El-Refaey et al.[29] assessed the effect of feedback respiratory training on the quality of life using the Pediatric Quality of Life Inventory (PedsQL).The comparison PedsQL revealed a nonsignif ciant difference between the groups.
Quality of evidence
The quality of evidence according to the GRADE system is presented in Supplementary Table 2.The quality of evidence for the functional outcomes was determined to be low for FEV1,PEF and Pimax and moderate for FVC,functional capacity and Pemax.
Discussion
Considering that breathing training in children with cerebral palsy can increase functionality,the findings of this study may contribute to clinical decision making.According to the meta-analysis results,respiratory exercises plus conventional rehabilitation were associated with improvements in pulmonary function and respiratory muscle strength when compared to conventional rehabilitation.Respiratory exercises have not been shown to be effective in improving gross motor function,and only one study demonstrated improvement in social well-being and acceptance and functioning domains of quality of life in individuals performing IMT.The quality of evidence for the FVC,FEV1 and quality of life outcomes were determined to be low to moderate.
Dystonia,spasticity,poor movement and lack of experience of certain postures can hinder the natural muscle development of children with CP,as well as disabling proper development of the chest and respiratory system [24].Significant postural impairments and muscle disorders could lead to inadequate development of the rib cage during childhood with little use of the diaphragm,mobilizing small amounts of air during inspiration [25].
Thus,in thinking that hypoventilation negatively affects respiratory status,strategies to improve respiratory muscle strength and activation in people with CP should all be addressed [24].Pulmonary rehabilitation in children and adolescents with asthma and chronic lung disease demonstrated that respiratory exercises of chest expansion increase thoracic mobility,suggesting better diaphragmatic contraction and increased quality of life and functional capacity[9-11].Improvements in functional capacity were also noted in this review.
Lee et al.[23] related just a small increase in PEF compared to pretraining values.Keles [2 4] explained that the increase in PEF is probably related to the improvement in Pemax,since PEF is influenced by expiratory muscle strength.These results suggest that exercises that involve activating the expiratory muscles should be encouraged in pulmonary rehabilitation programs to better enhance PEF.
The samples in the studies included in this review consisted of children or adolescents between levels (I to IV) of the Gross Motor Function Classification System (GMFCS),while those with classification V who are totally dependent on daily life activities and locomotion were not tested.We observed that the studies whose samples were of children classified as I and II revealed minor changes in respiratory function or no differences compared to the control group.Know and Lee [31] investigated the difference in lung capacity and muscle strengthening related to respiration depending on the level of the GMFCS in children with CP through tests of respiratory function and respiratory pressure.Once both lung function and respiratory muscle strength are positively correlated with mobility,the findings indicated that a decrease in functional motor ability as classified by the GMFCS could be accompanied by respiratory dysfunction,reinforcing that the greater the severity is in the progression of GMFCS levels,the greater the energy expenditure and inefficient ventilatory behaviors are during breathing.
In addition,children have to present preserved cognitive and cooperative function for breathing exercises to be effective.These findings are relevant to clinical practice,as they discuss the need to develop protocols designed beyond overall development but also to focus on pulmonary function,respecting the condition of each patient and their specific needs of therapy.In general,the studies have a great variation in relation to the number of sessions and session time.We observed that the optimal level of intensity in intervention programs for CP is not clear [13].
The COVID-19 pandemic also emphasizes the importance of pulmonary functions among individuals with neurological disabilities,and further investigations into the prescription of breathing exercise variables (e.g.,modality,load,frequency,duration) are recommended to enhance our understanding of the real positive effects of breathing exercises in children and adolescents with CP.Moreover,the relationship between posture and breathing has become an important topic for continuing education courses within the therapy community but is still little investigated [32-34].Interest will likely increase as the physical therapy community focuses more on performance (what patients are doing within their living environments) than capacity (what patients demonstrate in the therapy session).
This study has limitations.One of them concerns the methodological quality of the study as observed in the PEDro scale.Although all studies affirmed allocation to the treatment groups,only three studies indicated a computerized allocation method [22-24] by researchers not involved with the project.Furthermore,only one study reported blind allocation and data collection [24];both parents and raters in another study were blinded to group separation [23],and the rest of the studies presented no open reference to any blinding.
In conclusion,further investigations on respiratory exercises related to quality of life,functional and lung capacity,as well as the prescription of variables of these training protocols,are recommended to improve our understanding of the real positive results of respiratory exercises in children and adolescents with CP.Future well-controlled RCTs are required to reinforce the recommendation of respiratory exercise as an important rehabilitation treatment in people with cerebral palsy.Successful propositions of breathing exercises with other populations may provide a new direction for exercise prescription,such as lung volume recruitment [35].In addition,it will be important to match exercise prescription to clinical/treatment characteristics of a patient subgroup or individual patient.
Supplementary InformationThe online version contains supplementary material available at https:// doi.org/ 10.1007/ s12519-022-00642-1.
Author contributionsLCTR,CTRL,DRB,AMDM contributed to conceptualization,data aquisition,formal analysis,writing-original draft.MPAF,NMG,SME contributed to conceptualization,writing-original draft,writing-review and editing.All authors read and approved the final manuscript.
FundingThe authors declare that no funding,exceptionally,or other support was received during the preparation of this manuscript.
Declarations
Conflict of interestNo financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethical approvalNot needed.
 World Journal of Pediatrics2023年4期
World Journal of Pediatrics2023年4期
- World Journal of Pediatrics的其它文章
- World Journal of Pediatrics
- Instructions for Authors
- Clinical profile,etiology,and outcome of hemophagocytic lymphohistiocytosis associated with histiocytic necrotizing lymphadenitis
- Food allergy among Mexican infants and preschoolers: prevalence and associated factors
- A predictive model of response to metoprolol in children and adolescents with postural tachycardia syndrome
- Factors of heavy social media use among 13-year-old adolescents on weekdays and weekends
