Food allergy among Mexican infants and preschoolers: prevalence and associated factors
Martín Bedolla-Barajas · Jaime Morales-Romero · Rafael Sánchez-Magallón · Jorge Alejandro Valdez-Soto ·Tonatiuh Ramses Bedolla-Pulido · Carlos Meza-López
The number of people with food allergy (FA) has increased in recent decades,as has the number of foods to which they are allergic.Estimates of FA prevalence vary widely,likely because of different definitions,evaluated foods and geographic variations.In developed countries,overall prevalence estimates range from 1.9% to 7.2% [1,2].In Latin America,the prevalence of FA in children is between 1.4%and 5.3% [3-6],with important age-based variations (from 1.9% in infants to 0.4% in preschoolers) [7].FA is a complex trait in which the interplay of genetic and environmental factors results in disease expression.Well-known factors that increase atopic susceptibility include sex [8,9],age [10],and socioeconomic status [11-13].Furthermore,the association between family history of allergies and childhood FA has been consistently reported in recent years.Overall,a maternal history of allergic disease appears to be more strongly associated with FA than paternal history of atopy[14].
With the recent research activity in FA,more data are emerging from developed countries.However,epidemiological studies are relatively few in Latin American countries.Therefore,the objective of the present study is to determine off ending foods and describe the prevalence and risk factors for FA in infants and preschool children of Guadalajara,Mexico.This was an observational,cross-sectional study of patients younger than six years old (infants 1 to 2 years old;preschoolers 3 to 5 years old) who attended an organized preschool or daycare facility in Guadalajara,Jalisco,Mexico.The sample size was determined with a formula for estimating proportions in infinite population;for a 99% confidence,an expected FA proportion of 5.0% [3],a precision of 3%,the sample size was 350,adjusted for 20% losses,so the final size was 438 children;for the purposes of this study,one sample was calculated for the infant group and another for the preschool group.Data collection was performed during the period from October 1,2021,to November 15,2021.The city of Guadalajara has historically been divided into four sectors according to its geographical location;therefore,to achieve greater external validity,preschools and nursery schools were randomly selected within each sector.Therefore,for the purposes of the study,we divided the total sample size accordingly.
This study was approved by the Research Committee and the Research Ethics Committee of the Hospital where the researchers are affiliated,which depends on the University of Guadalajara.The mentioned schools did not participate in the methodological approval of this study.Teachers agreed to allow access to school facilities,and the children's parents gave their informed consent in writing.After explaining the aim of the study,first to the teachers/caregivers and then to the children's parents,who agreed to have their off spring participate in the research,they proceeded to answer a standardized questionnaire.The questions included age,sex,public or private school attendance,family history of atopy,and the presence of any current FA.For those who indicated the presence of FA,further details regarding the appearance of symptoms were requested.The time between food ingestion and the onset of symptoms and symptoms associated with food exposure were used to detect food hypersensitivity.To differentiate between food hypersensitivity and FA,the following question was included: does your son or daughter suffer from allergic reactions after eating food or drinking beverages? Then,from there,the clinical manifestations were considered as follows: allergic reaction to food was when the organs and symptoms were those typical of allergic reactions (urticaria and angioedema,difficulty breathing,wheezing,throat tightness or vomiting and diarrhea) and occurred within two hours after ingestion of the off ending food [15].
Continuous and categorical variables are presented as absolute values and percentages.Comparison of proportions between groups (with or without FA) was performed using the Chi-square test or Fisher's exact test.Crude odds ratios(ORs) and confidence intervals (CIs) were calculated in a simple 2 × 2 table.We used a multivariable logistic regression model to examine the association between the following covariates and the prevalence of FA: sex,age,public or private school attendance,parental history of atopy,and current atopy.The results were expressed as ORs with 95%CIs.IBM SPSS Statistics software Version 23 (Chicago,IL,United States) was used for statistical analyses.
A total of 810 children were included in this report;overall,54% (437) were male.A total of 373 (46%) patients were infants attending daycare facilities,and 437 (54%) were preschool children;the participation rates were 85.1% and 99.8%,respectively.Public school attendance was 53.6%.The estimated prevalence of food hypersensitivity was 12.5% and 3.2% for FA;girls had a higher prevalence of FA (3.8%) than their male counterparts (2.7%) (P=0.418).The prevalence of FA was 2.7 times higher in private versus public school children (4.8% versus 1.8%;P=0.018).The predominant symptoms reported by the study population were oral allergy syndrome (1.5%),urticaria (1.0%),and allergic systemic reaction (0.7%).No differences were found between the infant group and the preschool children group in this regard (P> 0.05) (Table 1).A personal history of atopy,private school attendance and maternal history of allergic rhinitis/atopic dermatitis were all associated with an increased risk of FA (Table 2).
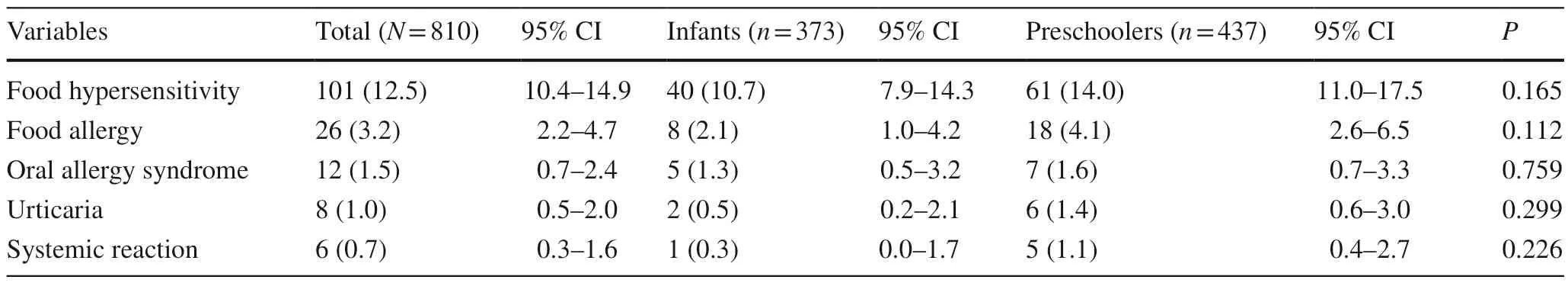
Table 1 Prevalence of hypersensitivity and food allergy in infants and preschoolers
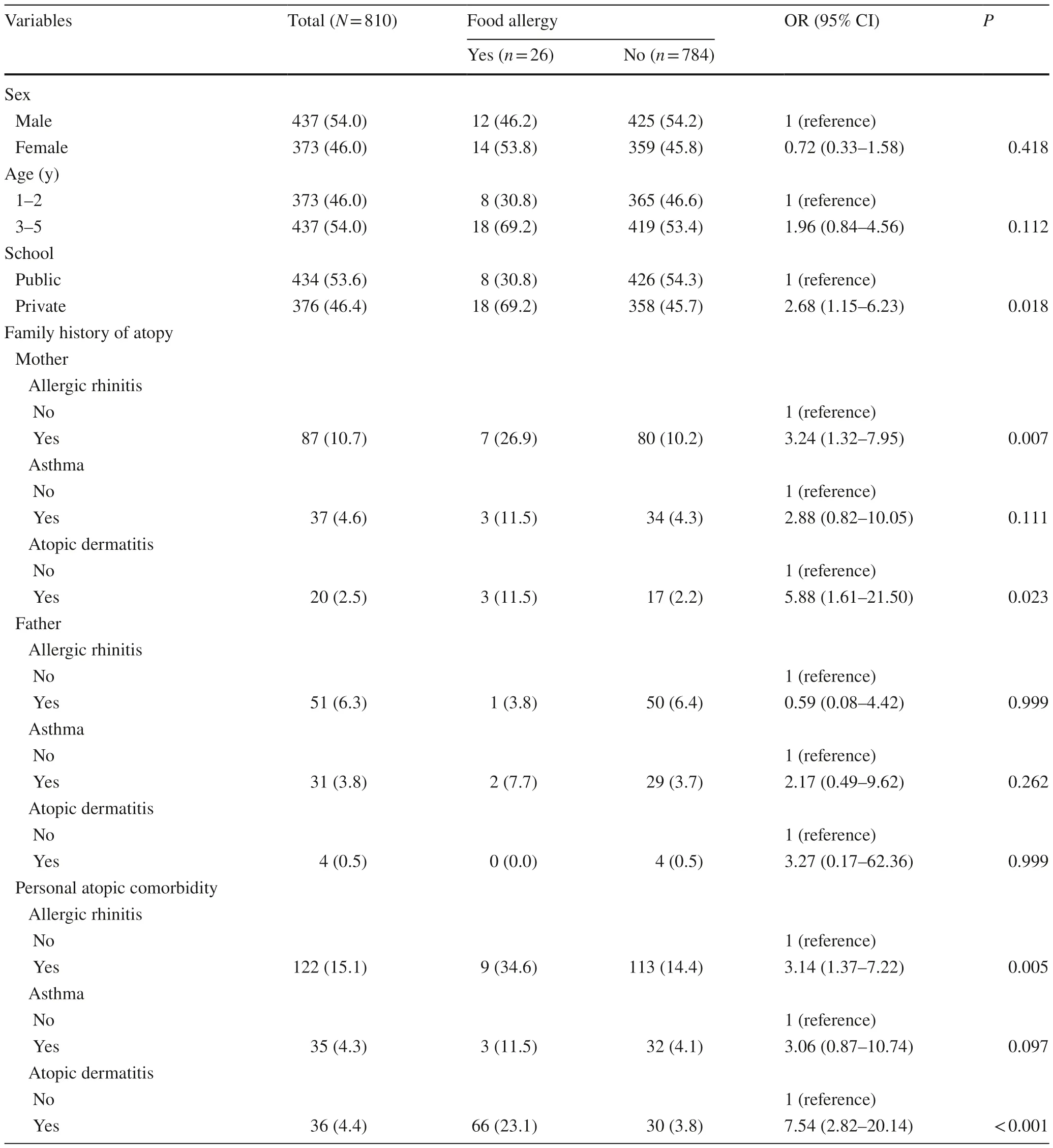
Table 2 Characteristics of infants and preschoolers with food allergy
The main symptoms of FA were itching of the mouth(65.4%),rash (42.3%),hives (42.3%),and itchiness of the face (38.5%) and skin (26.9%).The foods most frequently reported by parents as causing FA were 1.0% milk;1.0%fruits and vegetables;1.0% fish and shellfish;0.5% meats;0.5% cereals;0.5 nuts;0.2% legumes;and 0.1% oilseeds.The reported allergies to clams,hazelnut,walnuts,peanut,and cow's milk mainly evoke oral allergy syndrome;f sih and pork meat evoke wheals and hives (urticaria),and cheese,shrimp,egg,and soy are associated with full blown allergic systemic reactions.In multivariable analysis,private school attendance was associated with FA in both infants and preschool children (OR=3.10,P=0.011).We also observed a significant association between a maternal history of allergic rhinitis (OR=2.99,P=0.023) and a personal history of atopic dermatitis (OR=7.08,P< 0.001) with FA (Table 3).In this study,the prevalence of FA among children younger than six years was 3.2%.Cow's milk,fruits,vegetables,fish,and shellfish were among the top foods causing FA.We also observed a significant association of FA with atopic dermatitis,maternal history of allergic rhinitis,and private school attendance.
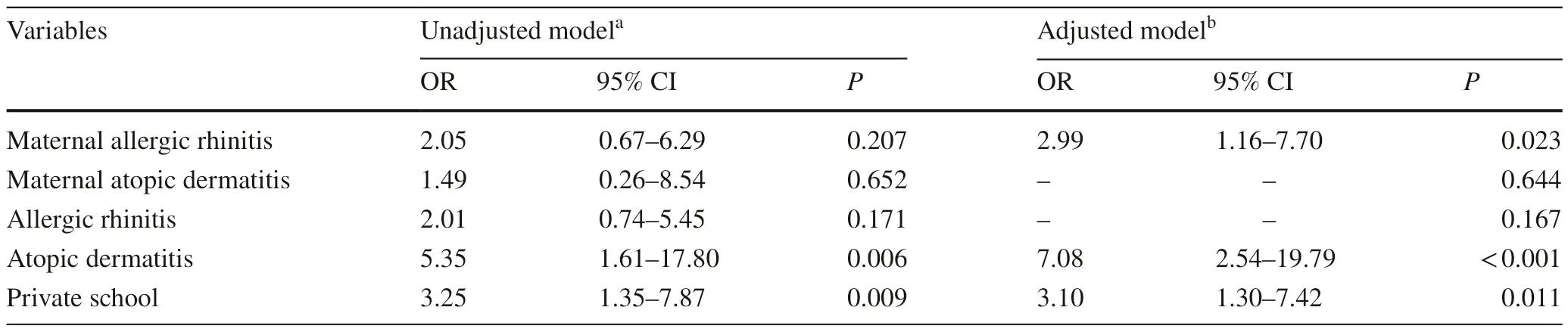
Table 3 Multivariable analysis of factors associated with food allergy in infants and preschoolers
To our knowledge,this is the first epidemiologic study to evaluate the prevalence of FA in Mexican preschool children.Ontiveros et al.,in a population-based study of Mexican schoolchildren,found a parent-reported prevalence of FA of 3.5% [3].Compared to the previously reported prevalence of FA in countries of Latin America,FA in Mexican schoolchildren is common,with the highest prevalence found to be 5.5% in Chile [16],followed by El Salvador [4],Mexico [3],Colombia [6],and finally Argentina at 1.4% [5].
Similar studies conducted in preschool children have reported higher prevalence rates than those reported in the present study (10% and 5.6%,respectively) [1,2].These differences in FA prevalence between age-matched groups could be explained by socioeconomic aspects and feeding patterns.In summary,the differences in the prevalence of FA among different populations could be explained by the availability of foods,the habits and customs of preparation and their frequency of consumption,along with ethnic differences and family or personal history of atopy.Unlike other studies,only a maternal history of allergic rhinitis was associated with an increased risk of FA.The relationship between maternal history of atopy and childhood FA has previously been considered in population-based studies.One such study reported that maternal asthma was associatedwith an increased risk of atopic dermatitis and wheezing in children [17].FA prevalence was found to be more frequent among atopic children than in nonatopic children,as we observed a significant association with atopic dermatitis.This is in line with the theory of “atopic march”,a term that describes the time-based progression of allergic diseases:from atopic dermatitis and FA in infants and preschoolers to gradual development into allergic rhinitis and allergic asthma in older children [18].Finally,children from private schools had a higher prevalence rate of parent-reported FAthan those from public schools.This finding is consistent with previously published studies [12,13,19] and could be attributed to socioeconomic aspects such as financial wealth and access to health services.[20].
This study has limitations that should be addressed,including its cross-sectional design.First,our study is based on parental reports,which may overestimate the prevalence of FA.Second,FA cases were not confirmed with clinical tests (oral challenges,skin prick test,etc.).Both could have constituted a possible information bias.Third,socioeconomic status was determined indirectly according to school attendance (public versus private).It should also be taken into account that although the sample size in this study was sufficient to identify the prevalence of FA (n=810),it may not be suitable for subgroup comparison,especially to explore secondary hypotheses.In this sense,caution is recommended when interpreting the results.Finally,we should mention that our results are based on a sample of children from an emerging economy and that they may differ markedly from those observed in developed economies.
In conclusion,the present study is the first to report the prevalence of FA in Mexican preschool children.Cow's milk was one of the main allergens in this population.We also observed an association between FA and atopic dermatitis,maternal history of allergic rhinitis,and private school attendance.
Author contributionsBBM contributed to conceptualization and methodology,formal analysis,investigation,writing of the original draft,review and editing,and project administration.MRJ contributed to methodology,formal analysis,investigation,writing of the original draft,review and editing,and project administration.SMR contributed to conceptualization and methodology,investigation,reviewing and editing,and project administration.VSJ contributed to methodology,investigation,reviewing and editing.BPTR contributed to conceptualization and methodology,investigation,and writing of the original draft.MLC contributed to investigation,writing of the original draft,and reviewing and editing.All authors critically revised the manuscript,agree to be fully accountable for ensuring the integrity and accuracy of the work,and read and approved the final manuscript.
FundingThe authors declare that no funds,grants,or other support were received during the preparation of this manuscript.
Data availabilityThe datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethical approvalAll procedures involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.The study was approved by the human ethics committee (Nuevo Hospital Civil de Guadalajara “Dr.Juan I.Manchaca”;No.00117).Written informed consent was obtained from parents.
Conflict of interestNo financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.The authors have no conflict of interest to declare.
 World Journal of Pediatrics2023年4期
World Journal of Pediatrics2023年4期
- World Journal of Pediatrics的其它文章
- World Journal of Pediatrics
- Instructions for Authors
- Clinical profile,etiology,and outcome of hemophagocytic lymphohistiocytosis associated with histiocytic necrotizing lymphadenitis
- A predictive model of response to metoprolol in children and adolescents with postural tachycardia syndrome
- Factors of heavy social media use among 13-year-old adolescents on weekdays and weekends
- Estimated prevalence and trends in smoking among adolescents in South Korea,2005-2021: a nationwide serial study
