Ocular manifestations of children with atopic dermatitis in Saudi Arabia
Lina Hassan Raffa, Tala Musa Roblah, Nasser Talal Balbaid, Bader Sameer Zimmo,3,Mahmood Jameel Showail
1Department of Ophthalmology, King Abdulaziz University Hospital, Jeddah, Saudi Arabia
2Faculty of Medicine, King Abdulaziz University, Jeddah,Saudi Arabia
3Department of Dermatology, King Abdulaziz University Hospital, Jeddah, Saudi Arabia
Abstract
INTRODUCTION
Atopic dermatitis (AD) is a common chronic condition of the skin that is characterized by inflammation and an erythematous patch pattern with exudation and crusting at early stages and scaling at later stages[1-2].Atopic dermatitis typically appears before the age of two[3].Although the pathogenesis of the disorder is complex, it caused by the interactive effects of genetic factors, abnormalities in skin barrier function and the skin microbiome, and immune dysfunction[1,4].The International Study of Asthma and Allergies in Childhood reported that AD has an incidence of 15%-20% in children and 1%-3% in adults in developed countries[5].However, the prevalence in Saudi Arabia is higher, as it was found to be 24% in a sample of 29 244 patients according to a systematic review[6].Another systematic review of the prevalence of AD in children in the Arabian Peninsula reported ranges between 7.5% and 22.5%[7].
AD can lead to various complications, including psychiatric,autoimmune and ophthalmic manifestations[8].Some examples of the ophthalmic manifestations of AD include blepharitis,eyelid dermatitis, conjunctivitis, uveitis, cataract, keratoconus,retinal detachment, ocular abnormalities caused by therapeutic agents used in AD and ophthalmic herpes simplex virus infections[6,9-11].The onset of ocular complications can be acute or chronic, and the majority of these complications could eventually lead to visual impairment if they are not promptly diagnosed and treated[9].Ocular complications are associated with several factors, including immune dysregulation, genetics,frequent eye rubbing, and side effects of medications[12].In a study that was conducted in Tokyo among 70 patients who visited the clinic from 2012 to 2015, half of AD patients had ocular abnormalities[11].Epidemiological studies have reported a higher prevalence of ophthalmic complications in AD subjects in a severity-dependent manner compared to the general population[9].Further, Carmiet al’s[12]study on AD in children (age 2mo to 15y) found that 25.4% had ocular symptoms, including conjunctivitis, nuclear cataract,blepharitis, and amblyopia.Among AD patients, the incidence of ocular manifestations is reported to be higher in AD cases with severe lesions on the skin, facial involvement, and longer duration of facial rash than in cases without these presentations[11].However, Pietruszyriskaet al[13]reported that serious ophthalmic complications could occur even in patients with mild skin changes; therefore, it was proposed that individuals with AD should be examined regularly for ocular abnormalities.It is not clear if the occurrence of ocular complications is associated with the severity of AD, as the studies so far have reported controversial results[11-12,14].Moreover, to our knowledge, the incidence of ocular complications in children with AD in Saudi Arabia has not been investigated so far.Therefore, the aim of this study is to assess the frequency of ocular manifestations in children with AD in the dermatology outpatient clinic at King Abdulaziz University Hospital and to determine if the occurrence of ocular complications is related to the SCORing Atopic Dermatitis (SCORAD) severity scores.Apart from this being the first such study to be conducted in Saudi Arabia,it is also the first study to report corneal topographic and pachymetric parameters for children with AD.
SUBJECTS AND METHODS
Ethical ApprovalThis study was conducted by the Departments of Ophthalmology and Dermatology and received the approval of the Research Ethics Committee of King Abdulaziz University Hospital (Approval number 481-21).The study was conducted in accordance with the tenets of the Declaration of Helsinki, and all the patient records and data generated were managed under strict confidentiality.Written consent was taken from the children’s guardians.
Patient RecruitmentThis is a cross-sectional study that reviewed 656 records of AD patients who visited King Abdulaziz University Hospital between 2005 and 2017.The exclusion criteria were age less than 4y for their lack of cooperation in undergoing the ophthalmic investigations or subjects older than 16y (n=170) and dermatitis caused by other diseases (n=247).After the exclusion criteria were applied, 239 children met the inclusion criteria, among whom 51 accepted the invitation and successfully completed the examination.However, one child was uncooperative and did not undergo the ocular examinations, and was thus, excluded.Therefore, the final cohort included 50 patients.The 50 children were assessed by the SCORAD scoring system for AD and the assessment was conducted between October 2021 and February 2022.In addition, the children were evaluated using a standardized protocol.Detailed demographic parameters were recorded, including past history of atopy,family history of atopy, and topical and systemic treatment of AD.AD severity was assessed with the help of the SCORAD index, which includes objective signs (extent and intensity)and subjective signs (pruritis and sleep disturbance) by a consultant dermatologist (Zimmo B).The extent is calculated using the rule of nines, and the intensity is evaluated by the presence of erythema, edema, papulation, oozing, excoriations,lichenification, and dry skin (0 to 3 points for each item).The patients were classified into mild AD patients (SCORAD score, <14), moderate AD patients (SCORAD score, 14-40),or severe AD patients (SCORAD score, >40).
Ophthalmological ExaminationsThe children underwent a slit lamp exam for inspection of the eyelids, conjunctiva,cornea, anterior chamber, iris, lens, and pupil.The presence of lid abnormalities, such as allergic shiners, Dennie-Morgan folds, eyelid thickening, ptosis, loss of the eyelashes,blepharitis, and ectropion, conjunctival abnormalities such as conjunctival papillary reaction, corneal abnormalities such as keratitis and corneal abrasions, uveitis, and cataracts,was recorded.Furthermore, visual acuity was assessed with Snellen’s chart (TOPOCON ACP7, Japan) and presented as logMAR values.Subnormal visual acuity was considered as a visual acuity worse than 20/30 in either eye.Amblyopia was diagnosed based on a two-line difference in visual acuity between the eyes.Spherical refractive error and total astigmatism were measured with an auto refractometer(TOPCON Autokerato-refractometer; TOPCON, Japan).A dilated retinal exam was conducted on the patients, and intraocular pressure was measured by an air puff (Carl Zeiss Meditec AG, Germany) if patients were cooperative.Oculus Pentacam Scheimpflug tomography (Oculus Optikgerate GmbH, Germany) was utilized to measure corneal parameters.We obtained data on pachymetry measurements at the thinnest and central points of the cornea, astigmatic power, irregularity indices, the distance between the thinnest point of the cornea and its center, anterior and posterior elevation values, distance of the anterior and posterior elevation points from the center of the cornea, corneal density, and mean keratometry values.Further, pachymetry, cornea volume, anterior chamber volume,anterior chamber angle, anterior chamber depth, keratometric power deviation, and Belin-Ambrosio enhanced ectasia display readings were recorded.Keratoconus was suspected based on the cut‐off values for laser vision correction[15].The patient was considered to have moderate risk of keratoconus if the mean keratometry readings were 48.1-50 D or corneal thickness at the thinnest point was 470‐500 μm, or the patient was considered to be at high risk of keratoconus if the mean keratometry readings were greater than 50 or corneal thickness at the thinnest point was <470 μm.Further, keratoconus was suspected if anterior elevation and posterior elevation at the thinnest part of the cornea were ≥8 and ≥18 respectively.The tomographic indices we chose to incorporate into our classification system were Kmax, Pmin and Ⅰ‐S value.Kmax is the maximum curvature from the anterior corneal maps,and Pmin is the minimum pachymetric measurement.The I-S value is the difference between the inferior and superior average dioptric values 3 mm peripheral to the corneal vertex.Eyes classified as Keratoconus suspect had mild tomographic irregularities, such as asymmetric bowtie, skewed radial axis, or superior/inferior steepening >1.4[16-18].Moderate risk for keratoconus is considered when Kmax >47.2 D[16-18],minimum pachymetry <470 μm[16,19-20]and I-S >1.7 signifies a high probability of Keratoconus[18].These are considered to be risk factors for Keratoconus given that progressive steepening and thinning of the cornea are well-known features of the pathophysiology of keratoconus.All the patients were diagnosed by an ophthalmologist who was an expert in corneal and external eye diseases (Shouai M).Patients were considered to have an ophthalmological abnormality if one or more of the following signs were present: glaucoma, keratoconus suspicion based on the aforementioned criteria in addition to lid, conjunctival, corneal, lenticular, and retinal abnormalities.
Statistical AnalysisStatistical analysis was conducted with IBM SPSS version 23 (IBM Corp., Armonk, NY, USA), and the results were visualized with GraphPad Prism version 8(GraphPad Software Ⅰnc., San Diego, CA, USA).Ⅴariables were presented using simple descriptive statistics as counts and percentages for categorical variables and mean and standard deviations for continuous variables.The Chi-square test was used for analyzing the association of the parameters (including the clinical severity of AD based on the SCORAD score) with ocular abnormalities.Comparison of two groups and more than two groups was conducted by an independentt-test and oneway ANOⅤA, respectively.Pearson correlation analysis was used to determine the correlation between variables presented by means.All comparative analyses were done under the assumption of normality and were adjusted for using Levenes test.The significance level was set atP<0.05.
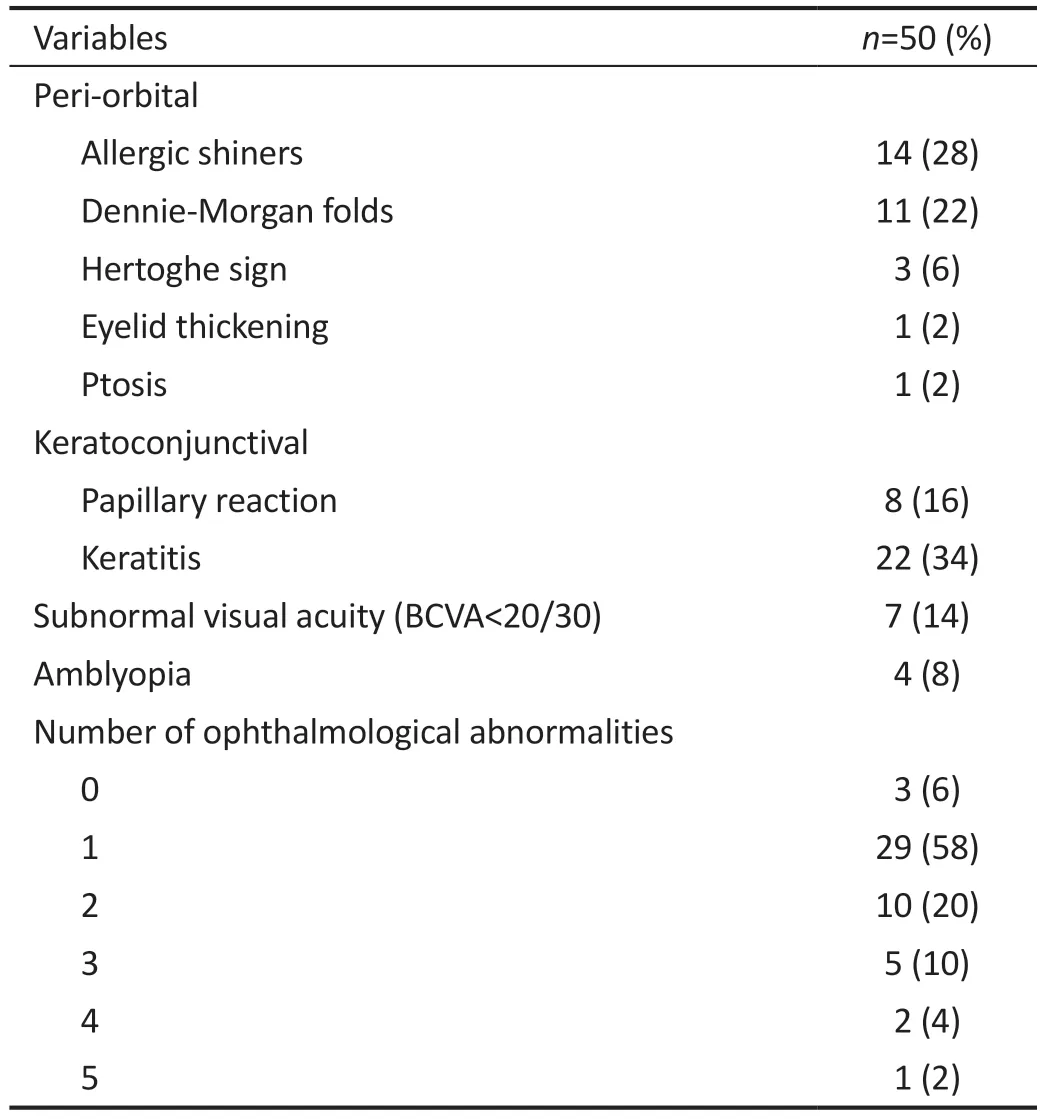
Table 1 Ocular abnormalities among AD patients
RESULTS
Ophthalmological ResultsThe mean age was 10.48±3.6y,and there was a slight male predominance (54% male children).Out of the 50 patients, 46 (92%) had ocular manifestations.Lid abnormalities such as allergic shiners,dennie morgan folds, eyelid thickening, and ptosis 54% (27/50)accounted for the majority of the ocular abnormalities followed by superficial punctate keratitis 44% (22/50).Half the patients had keratoconjunctivitis.None of them had lenticular or retinal abnormalities, glaucoma or uveitis.Further, 24 children had a family history of atopic diseases (48%), and 11 had a personal history of atopy (22%).The findings of the ophthalmic examination are shown in Table 1.The median spherical equivalence of the right and left eye was 0.63 D (range, -5.13 to +4.50 D) and 0.63 D (-5.13 to +4.25 D) respectively.The association between ophthalmic traits and variable ophthalmic variables are shown in Table 2.Children with 2 or more ophthalmic traits were found to of significantly older age, had more periorbital signs and lower SCORAD.Higher SCORAD scores were not associated with greater ocular involvement.
Dermatological ResultsAD severity was scored as mild in 7 children (14%), moderate in 19 children (38%), and severe in nearly half of the patients (48%).Further, 28 patients had facial involvement (56%), and 25 had peri-orbital signs (50%).The children had been treated topically with emollients in 12 cases and emollients and steroids in 35 cases.With regard to systemic treatment, half of the patients were being treated with only antihistamines (25/50, 50%), while two (4%) were being with antihistamines and oral steroids.The mean SCORAD score was 35.75.Children with a history of systemic treatment(27/50, 54%) had significantly higher SCORAD scores(41.11±17.1), as expected, than those who did not have a history of systemic treatment for AD (29.46±12.8,P=0.01).However, the SCORAD score did not differ according to age,sex, or any of the ophthalmological parameters.No correlation was found between the SCORAD score and the number of ophthalmological abnormalities.

Table 2 Association between the number of ophthalmic abnormalities and various variables
Corneal ParametersBased on the keratometry results, the patients were divided into three groups: normal, keratoconus suspicion, and moderate risk of keratoconus.Four patients were found to have moderate risk for keratoconus in one eye(8%), and keratoconus was suspected in eight patients (16%)(both eyes in six patients and one eye in two patients).Only four out of these patients had positive periorbital signs (8%),and only one had allergic conjunctivitis (2%).
DISCUSSION
In this study, which is the first one on ocular abnormalities in children with AD in Saudi Arabia, we found that 92%of the children had ocular manifestations on examination.There is not enough updated information in the literature about the occurrence of ocular complications in children with AD, but the available studies estimate that the incidence is 25% to 50%[12,14].This implies that the incidence of ocular complications in this cohort is considerably higher than reported estimates and might indicate the need for regular ophthalmologic examinations in children with AD in Saudi Arabia.
The SCORAD scores in the present cohort were not found to be associated with age, gender, or any of the measured ophthalmological parameters, and no association was found between the number of ocular complications and SCORAD score.Thus, even patients with mild AD based on the SCORAD score could present with ocular complications that might lead to sight-threatening conditions.This is supported by the case reported by Downie[21]in which bilateral corneal hydrops rapidly developed in an 8-year-old male patient with AD.Our findings further emphasize the need to conduct larger studies to ascertain whether regular ophthalmologic examinations in children with AD, even in those with mild disease.
With regard to the type of ocular abnormalities in this cohort,the majority of the children had palpebral and corneal changes,but none of them had sight-threatening complications such as retinal detachment and glaucoma.In our cohort, 12 children had allergic shiners, 11 had Dennie-Morgan folds, and 1 child exhibited Hertoghe sign in both eyes.These signs could be attributed to repeated itching and rubbing of the eyes.However,none of them had blepharitis, which is known to affect more than 6% of AD patients and less than 1% of the total population.The reported incidence of blepharitis in adult AD patients is highly varied.For example, one study conducted in Japan reported that 41.1% of AD patients had blepharitis, and these patients had higher SCORAD scores[11].On the contrary,a cross-sectional study conducted in Malaysia reported that only 2 out of 80 AD patients had blepharitis[22].With regard to the occurrence of blepharitis in children with AD, Carmiet al[12]reported that 1 out of 59 children had chronic atopic blepharitis.All the children in their study had mild AD,while only 7 children in this study had mild AD.This, again,indicates that the occurrence of this ocular complication is not associated with the severity of AD.Although these findings imply that the incidence of blepharitis in children with AD is low, more studies are required to confirm these findings.
Carmiet al[12]reported that the main ocular lesion in their cohort of children with AD was follicular conjunctivitis,which was detected in 18% of their AD patients who had ocular diseases.Furthermore, bacterial, viral, and fungal conjunctivitis is also associated with AD.In fact, a 20-fold greater risk ofStaphylococcus aureuscolonization exists in AD patients[23].Foster and Calogne[24]stated that the dominant feature in the 45 AD patients included in their study was atopic keratoconjunctivitis mainly involving the inferior forniceal and palpebral conjunctiva.Moreover, a clinical review conducted in Houston, Texas, revealed that atopic keratoconjunctivitis occurs in 25% to 42% of patients with AD[9].In accordance with all these findings, 50% of the children in this study had keratoconjunctivitis.A study conducted in India showed that 43% of AD patients had ocular lesions in their lids and conjunctiva.Further, 41.9% of the 43% had only eyelid involvement, 37.2% had only conjunctival involvement, and 20.9% had both eyelid and conjunctival involvement[14].In contrast to these findings, most of the patients in the present study had normal corneal and conjunctival features, but a higher percentage suffered from lid changes associated with AD.However, no significant associations were found between the AD severity index and conjunctival involvement,keratitis, or lid abnormality.In the Carmiet al[12]study in which follicular conjunctivitis was the main presentation, all the children had mild AD.This further implies that this ocular complication could occur even in cases of mild AD and reiterates the need for regular ocular examinations in children with AD.
The association between glaucoma or uveitis and AD remains understudied and under-reported.A study on Danish citizens with AD did not find a significant association between AD and glaucoma[25].Similarly, glaucoma was not detected in any of the patients in our cohort even though topical corticosteroids were used by 35 of the 50 patients and oral prednisone was used by two patients.Uveitis was not detected in any of our patients either.Likewise, an article about the impact of allergy and atopy on new onset of uveitis in Germany demonstrated that there is no significant correlation between atopy and new onset of uveitis[26].
Atopy seems to be an important factor in the occurrence of keratoconus[27].However, reports on the prevalence of keratoconus among atopic patients are conflicting[25,28].Shajariet al[27]reported that keratoconus was detected more frequently in adult AD patients than in normal subjects.Furthermore,Kayaet al[29]reported that the thickness of the central and thinnest parts of the cornea was lower in AD patients with keratoconus than in patients with keratoconus without AD.In accordance with these previous studies, we found that four patients in our cohort had a moderate risk of keratoconus and eight had keratoconus suspicion.However, we did not find a significant association between keratoconus and AD severity index.In contrast to all these findings, Bawazeeret al[30]concluded that there is no significant correlation between AD and keratoconus: atopy was indirectly associated with keratoconus because of frequent itching and rubbing of the eye.However, in our study, eyelid eczema that could lead to frequent eye rubbing was found in only 4 of the 12 patients at risk of keratoconus and allergic conjunctivitis was confirmed in only one of them.Thus, the association between AD and keratoconus is a subject that requires further research and evaluation in the future.Despite the lack of clarity on this, it is important to examine children with AD for keratoconus,even if they have mild AD and are in the early stages, as keratoconus tends to develop and progress rapidly.Detecting and treating it in the early stages will help prevent sightthreatening complications that could occur later on.
Cataracts affect nearly 12% of AD patients[31].Further, a study conducted at Kyoto University did not find any relationship between the clinical features of AD and cataract occurrence and progression[32].On the contrary, a study conducted in Denmark showed a significant association between the development of cataract and AD[25].The prevalence of rhegmatogenous retinal detachment in pediatric AD patients is 10.5% which was higher than the control group at 5.5% in a Korean 12-year nationwide cohort study[33].On the contrary, none of the children in our cohort had any retinal abnormalities, and retinal detachment was not reported in Carmiet al’s[12]cohort of children with AD either.
In the present study, a family history of atopy was not an important indicator of ocular manifestations.On the contrary,another study observed a statistically significant association between a family history of atopy and ocular manifestations in Indian children with AD[14].Another study found that facial involvement was associated with ocular changes[34].However,we did not find a significant association between facial involvement and the number of ocular abnormalities.Thus, it is not clear whether dermatological parameters related to the face might be good indicators of ocular complications when examining children with AD.
In the present study, a significant association was found between the number of ophthalmic abnormalities and periorbital signs, SCORAD score and age, but the number of ophthalmic abnormalities did not show a significant association with sex,personal or family history of atopy, or facial eczema.These associations, or lack thereof, have not been reported previously in the context of AD in children and ocular abnormalities in Saudi Arabia, so the findings are important in terms of determining the risk of ocular abnormalities in these patients.However, they need to be confirmed through future studies.
Several limitations of this study should be mentioned.The first one is the small sample size.As there is very little literature on ocular complications in children with AD, the findings need to be confirmed in a larger-scale prospective study.Second, as some of the children were uncooperative during the examination, their results were unreliable and had to be excluded.This further decreased the amount of data available for analysis.Third, this study might have a selection bias,since patients with severe AD were probably more interested in participating.This might also explain why nearly half of the examined patients had high SCORAD scores.As a result, the incidence of ocular morbidities might have been overestimated.One of the biggest strengths of this study is that it is the first to carry out a complete ocular examination in Saudi children with AD and examine the association of ocular complications with AD severity.Furthermore, corneal topography was evaluated to explore the topographic and pachymetric status of young children with AD, and the data have been reported for the first time.Moreover, our study included a wide age group of 4 to 16y that was fully examined for different ophthalmic conditions, so a large number of presentations were covered in a wide age range.
To sum up, this is the first study in Saudi Arabia to evaluate the prevalence of ocular manifestations in children with AD.Furthermore, it is the first study that assesses corneal topography among children with AD.The majority of children in this study had ocular abnormalities, which mainly included lid and corneal abnormalities.Moreover, 8% of the patients were found to have a moderate risk for keratoconus in one eye,and keratoconus was suspected in 16%.None of the patients had sight-threatening complications, such as glaucoma and retinal detachment, even though nearly half had severe AD based on the SCORAD severity index.Further, no association was found between ocular abnormalities and severity of eczema, facial eczema, or peri-orbital eczema.Larger-scale studies are needed to affirm whether regular screening for ophthalmic abnormalities is beneficial among children with AD in terms of early intervention and prevention of sightthreatening complications.
ACKNOWLEDGEMENTS
Conflicts of Interest: Raffa L,None;Roblah T,None;Balbaid N,None;Zimmo B,None;Showail M,None.
CORRlGENDUM
Safety profile of 0.0015% tafluprost eye drops in China: a post-marketing observational study
Xue-Li Chen,Yan-Jing Fu,Bo Qu,Ye-Wei Wang,Xin Tang,Yu-Hong Wang,Guo-Yi Zhou,Ming-Kai Lin,Jing-Yuan Shen,Jin Yao,Su-Yan Li,Miao-Qin Wu,Hua-Zong Peng,Ming-Ying Lai,Ren-Yi Wu,Yi-Nong Zhang,Yan Li,Xiao-Jun Wu,Ming-Chang Zhang,Su-Ping Guo and Xing-Huai Sun
(Int J Ophthalmol2023;16(1):108-114.DOI:10.18240/ijo.2023.01.16)
The authors would like to make the following change to the above article:
The name of the second author Yan‐Jing Fu should be modified as “Yan‐Jiang Fu”.
The authors apologize for any inconvenience caused by this error.Association ofCFHandMAP1LC3Bgene polymorphisms with age-related macular degeneration in a high-altitude population
Rui-Juan Guan,Xin Yan,Ling Li,Ze-Feng Kang,Xiao-Ying Zhang,Huan-Juan Yang
(Int J Ophthalmol2022;15(11):1752-1756.DOI:10.18240/ijo.2022.11.04)
The authors wish to add the foundations as follow:
Foundations:Supported by the Qinghai Province Department of Science and Technology under grant (No.2020-zj-780); Qinghai Kunlun Talents, High-end Innovative Top-Notch Talents.
The authors apologize for any inconvenience caused by this error.
 International Journal of Ophthalmology2023年5期
International Journal of Ophthalmology2023年5期
- International Journal of Ophthalmology的其它文章
- Comment on “Factors affecting single-step transepithelial photorefractive keratectomy outcome in the treatment of mild, moderate, and high myopia: a cohort study”
- Visual function and biofeedback training of patients with central vision loss: a review
- A case of Posner-Schlossman syndrome treated by gonioscopy-assisted transluminal trabeculotomy
- Mitochondrial dysfunction in glaucomatous degeneration
- Publication trends of primary angle-closure disease during 1991-2022: a bibliometric analysis
- Improving myopia awareness via school-based myopia prevention health education among Chinese students
