Twenty-four-hour movement guidelines during middle adolescence and their association with glucose outcomes and type 2 diabetes mellitus in adulthood
Antonio Grí-Hermoso,José Frniso López-Gil,Ysmin Ezztvr,Roinson Rmírez-Vélez,Mikel Izquierdo
a Navarrabiomed,Hospital Universitario de Navarra(HUN),Universidad P′ublica de Navarra(UPNA),IdiSNA,Pamplona 31008,Spain
b Health and Social Research Center,Universidad de Castilla-La Mancha,Cuenca 16007,Spain
c Department of Nursing,Universitat de Val‵encia,Valencia 46010,Spain
Abstract Purpose:The aim of the present study was to determine the association between adherence to the 24-h movement guidelines during middle adolescence and glucose outcomes (glycated hemoglobin and fasting glucose)and type 2 diabetes mellitus (T2DM)in adulthood,14 and 22 years later.Methods:We analyzed data from apparently healthy adolescents aged 12-18 years who participated in Waves I and II(1994-1996,n=14,738),Wave IV(2008-2009,n=8913),and Wave V(2016-2018,n=3457)of the National Longitudinal Study of Adolescent to Adult Health(Add Health)in the United States.Physical activity,screen time,and sleep duration were measured using questionnaires,and the 24-h guidelines were defined as:5 or more times moderate-to-vigorous physical activity per week,≤2 h per day of screen time,and 9-11 h of sleep for 12-13 years and 8-10 h for 14-17 years.Capillary and venous whole blood was collected and analyzed to determine glycated hemoglobin and fasting glucose for Waves IV and V,respectively.Results:Only 2.1%of the adolescents met all the 3 guidelines,and 37.8%met none of them.In both waves IV and V,adolescents who met physical activity and screen time guidelines had lower odds of T2DM in adulthood than those who did not meet any of these guidelines(Wave IV;prevalence ratio(PR)=0.57,95%confidence interval(95%CI):0.21-0.89;Wave V:PR=0.43,95%CI:0.32-0.74).Only for Wave V did adolescents who met all 3 guidelines have lower odds of T2DM at follow-up compared with those who did not meet any of these guidelines(PR=0.47, 95%CI: 0.24-0.91). Also, for each increase in meeting one of the 24-h recommendations, the odds of T2DM decreased by 18%(PR=0.82,95%CI:0.61-0.99)and 15%(PR=0.85,95%CI:0.65-0.98)in adulthood for Waves IV and V,respectively.Conclusion:Promoting all 24-h movement guidelines in adolescence,especially physical activity and screen time,is important for lowering the potential risk of T2DM in adulthood.
Keywords: Glucose metabolism;Glycated hemoglobin;Physical activity;Screen time;Sleep duration
1. Introduction
The annual incidence of type 2 diabetes mellitus (T2DM)has increased 30.5% over the last decade globally, reaching more than 20 million new cases in 2017.1T2DM is now considered one of the 4 major noncommunicable diseases.1People with T2DM often have other cardiovascular risk factors,including hypertension and dyslipidemia,2and are at increased risk for cardiovascular disease.3Therefore, efforts to identify effective strategies to prevent this disease remain urgent.
Adolescence is the period between childhood and adulthood, defined by the World Health Organization as ages 10-19 years.It is a period of rapid organ system development,and it is critical to adult health.4T2DM is an extreme consequence of obesity and insulin resistance in youth, but other less obvious metabolic conditions (e.g., hypertension, hyperlipidemia, or insulin resistance) are far more common and equally concerning.5Hence the importance of identifying adolescents at risk for metabolic disturbances and implementing long-lasting,successful treatment regimens.This phase is also important for understanding health and disease in adulthood,as behaviors established during adolescence might track into adulthood.6Some studies have focused on the association of some of these behaviors in isolation (e.g., sleep duration,7screen time,8,9and physical activity8,10) with T2DM during adolescence or with impaired glucose later in life. However,these behaviors are time-dependent, eliciting distinct biological processes that interact throughout a 24-h period.To address this issue, the Canadian 24-Hour Movement Guidelines for Children and Youth were developed, representing a paradigm shift in thinking about daily movement behaviors.11These guidelines propose 9-11 h of uninterrupted sleep per night for children aged 5-13 years and 8-10 h per night for those aged 14-17 years,as well as no more than 2 h of recreational screen time per day and at least 60 min of daily moderate-to-vigorous physical activity.11
A recent meta-analysis demonstrated that only 2.68%of adolescents from 23 countries were meeting the 24-hour guidelines.12There are few studies on the combined association of movement behaviors with glucose metabolism outcomes among children and adolescents;13-17most of them have been crosssectional or did not analyze the relationship between those outcomes and the risk of T2DM later in life.Few prospective studies have been published on this topic.For instance,one of these studies showed that meeting all the guidelines during childhood was not associated with lower levels of fasting glucose but with fasting insulin at 2 years follow-up.13Another study reported that multiple movement behaviors should be targeted to reduce cardio-metabolic risk in childhood.16Previously, the Coronary Artery Risk Development in(Young)Adults(CARDIA)study18demonstrated that youth aged 18 years with healthier behaviors(e.g., normal weight, regular physical activity, healthy diet, no smoking,and no alcohol consumption)are more likely to reach middle age with optimal glucose levels than those who do exhibit such behaviors. Another study showed that for adolescents with low levels of physical activity engagement,reducing sedentary behaviors was protective from T2DM during young adulthood.19Previous systematic reviews suggest that meeting more components of the guidelines was associated with better health indicators in youth20,21and adults.22Furthermore, these modifiable behaviors may be pathways for public health interventions intended to curb obesity23and,therefore,decrease the risk of noncommunicable diseases such as cardiovascular disease and T2DM.24
As far as we know, no existing studies have analyzed the relationship between 24-h movement behaviors in adolescence and the risk of T2DM in adulthood. Therefore, the aim of the present study was to determine the association between adherence to the 24-h movement guidelines during middle adolescence and glucose outcomes (glycated hemoglobin (HbA1c)and fasting glucose)and T2DM in adulthood among a diverse sample of American youth, with data taken from the National Longitudinal Study of Adolescent to Adult Health (Add Health).
2. Methods
2.1. Participants
This is a longitudinal study with data taken from the Add Health study,a nationally representative sample of youth from Grades 7-12 in the United States who were followed from adolescence through adulthood. During 1994 and 1995, over 90,000 students from a sample of 80 high schools and 52 middle schools selected with unequal probability of selection completed in-school questionnaires.Of these students,20,745 were selected to participate in the Wave I in-home interviews in 1994.25The Wave II in-home sample followed in 1996(n=14,738;age range:12-18 years),Wave IV in 2008-2009(n=15,701; age range: 24-32 years), and Wave V in 2016-2018 (n=5381 with cardiometabolic data, age range:33-39 years). Those participants with missing data on 24-h movement behaviors(n=3524)and/or those adolescents diagnosed with T2DM(n=62)at Wave I or II were excluded from the analysis. At Waves IV and V, we also excluded participants with missing data for dependent variables (i.e., HbA1c and fasting glucose)and covariates(Wave IV:n=3442;Wave V: n=1924). Our final sample included 8913 and 3457 individuals who provided responses regarding 24-h movement behaviors from the in-home interviews at Waves I-II and participated in Waves IV and V providing measures of glucose homeostasis.
The Add Health study was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill.Permission to conduct secondary analyses was obtained by the Ethics Committee of the University Hospital of Navarra(PI_2020/143).Regarding participation in this study,the parents or legal guardians of the adolescents received a signed written informed consent form before the participants’enrollment.
2.2. Anthropometry
Height and weight were self-reported in adolescence(Waves I and II) and measured in adulthood (Waves IV and V), and body mass index was calculated by dividing body weight (in kg) by height (in m2). During the in-home interviews for Waves IV and V,waist circumference was measured to the nearest 0.5 cm at the superior border of the iliac crest,as recommended by the National Cholesterol Education Program Third Adult Treatment Panel.26
2.3. T2DM
The capillary or venous blood draw was performed as the final stage of the home exam following the collection of anthropometric,cardiovascular,and medication information.
At Wave IV, capillary whole blood was collected from a finger prick and analyzed to determine HbA1c and fasting glucose.At Wave V,a venous blood draw was collected after confirming respondents were comfortable giving blood and asked to either sit or recline at their discretion.Venous blood samples were collected at home,and immediately following collection,tubes were stored at 39.2˚F for up to 2 h,then centrifuged and aliquoted.The glucose measure was classified as fasting if the measurement was taken at least 8 h after the participant’s last meal and as non-fasting otherwise. Respondents who were fasting(≥8 h)and non-fasting(<8 h)at the time of blood collection were identified. Use of a prescription medication in one or more of the therapeutic classes in the previous 4 weeks was assigned a value of 1. Non-use of a prescription medication in one of the therapeutic classes in the previous 4 weeks was assigned a value of 0.
Adults were categorized as having T2DM if they had a fasting glucose ≥126 mg/dL,a non-fasting glucose ≥200 mg/dL,an HbA1c ≥6.5%, a self-reported history of diabetes except during pregnancy,or anti-diabetic medication use in the previous 4 weeks.27
2.4. Measuring 24-h movement behaviors
2.4.1. Physical activity
In the Wave I and Wave II in-home interviews,adolescents reported their engagement in moderate-to-vigorous physical activity (MVPA) during the past 7 days according to a previously described scale and in response to 3 different questions:28“During the past week, how many times did you go rollerblading, roller-skating, skateboarding, or bicycling?”;“During the past week,how many times did you play an active sport,such as baseball,softball,basketball,soccer,swimming,or football?”;“During the past week,how many times did you do exercise, such as jogging, walking, karate, jumping rope,gymnastics, or dancing?” Responses ranged from not at all to 5 or more times,and they were scored as:not at all=0;1 or 2 times=1.5;3 or 4 times=3.5;5 or more times=6.Responses to the 3 questions were summed to create a measure of total instances of MVPA each week. They were then classified as no (0 times), some (1-4 times), and high (5 or more times)MVPA per week.Physical activity guidelines were considered met when adolescents reported 5 or more instances of MVPA per week in both of the first 2 waves. This recommendation was used previously by Gordon-Larsen et al.28with the same cohort.
2.4.2. Screen time
This behavior was determined according to a previously described scale28using the following questions: “How many hours a week do you watch television?”; “How many hours a week do you watch videos?”; and “How many hours a week do you play video or computer games?” Hours given in the 3 responses were summed to create a measure of recreational screen time per week.Screen time guidelines were considered met when adolescents reported<2 h per day in both of the first 2 waves.
2.4.3. Sleep time
Adolescents reported their sleep duration (in hours) in response to a single question in the Waves I and II inhome interviews: “How many hours of sleep do you usually get per day and/or night?” Adequate sleep duration was estimated according to guidance from the National Sleep Foundation.29Sleep duration guidelines were considered to be met when adolescents reported getting from 9 h to 11 h and 8 h to 10 h per day of sleep in those aged 12-13 and 14-17 years old, respectively, and in both of the first 2 waves.
2.5. Definitions of covariates
In-home questionnaires were used to collect information on sociodemographic factors, including age, sex, race/ethnicity(operationalized as a 4-level: White, Black or African American, American Indian or Native American, and Asian or Pacific Islander), region (coded as West, Midwest, South, and Northeast), and educational attainment (based on the highest education level attained at Waves IV and V, categorized as:less than a high school education, high school graduate or vocational school,some college,and college graduate or graduate education).
Alcohol consumption was assessed by way of responses to the following question:“Within the last 30 days,on how many days did you have alcohol (beer, wine, liquor)?” Participants who reported “never used”were classified as “never drinker”,those who reported “have used, but not in last 30 days” were classified as “former drinker”, and those who chose other options were classified as“current drinker”.Alcohol consumption is an important lifestyle factor that seems to be associated with the risk of developing T2DM.30
For smoking habits and cigarette use, adults who reported“never used”or“have used,but not in last 30 days”were classified as“not current users”,and participants who reported cigarette use at least one day in the last 30 days were classified as“current users”. Smokers are insulin resistant, exhibit several aspects of the insulin resistance syndrome, and are at an increased risk for T2DM.31
High sensitivity C-reactive protein was determined using a high sensitivity particle-enhanced immunonephelometric assay (Siemens Healthcare Diagnostic Products GmbH, Marburg,Germany).
Last,professional field staff measured blood pressure using a calibrated blood pressure monitor.Using the 2017 guidelines of the American College of Cardiology and the American Heart Association Hypertension,32hypertension was defined as having systolic blood pressure ≥130 mmHg and/or diastolic blood pressure ≥80 mmHg.
2.6. Statistical analysis
Descriptive information is shown as numbers and percentages for categorical variables and as mean and standard deviation for continuous variables. All model assumptions were checked (i.e., normality and homoscedasticity), and HbA1c and fasting glucose results were log-transformed (base 10) to normalize the distribution.
We conducted a series of linear regression models to examine the associations between meeting specific (i.e., physical activity only,screen time only,sleep duration only)and general combinations (i.e., physical activity and screen time, physical activity and sleep duration,screen duration and sleep time,and all three)of 24-h movement guidelines with HbA1c and fasting glucose. For these analyses, not meeting the guideline(s) was used as the reference group.
Poisson regression with robust error variance analyses33were used to estimate the prevalence ratio (PR) of T2DM(dependent variable)according to meeting specific(i.e.,physical activity only, screen time only, sleep only) and combinations (i.e., physical activity and screen time, physical activity and sleep duration, screen duration and sleep time, and all three) of 24-h movement guidelines at Waves I and II (independent variables). In all cases non-meeting the guideline(s)was the reference group.We also tested the odds of T2DM for each increase in one 24-h movement guideline. All analyses were adjusted by biological sex, race/ethnicity, age at followup, highest education achieved, alcohol consumption at follow-up,smoking habit at follow-up,high sensitivity C-reactive protein, waist circumference, and hypertension. Further, we used mutual adjustments between physical activity, screen time,and sleep duration.
To correct for design effects and unequal probability of selection, we used STATA Version 17.0 (StataCorp., College Station,TX,USA)with survey prefix command(SVY)to conduct design-based analyses that accounted for stratification,clustering, and unequal probability of selection34and set significance at p<0.05.STATA weights the data so that it is representative of the actual composition of each school based on grade level and gender and corrects for the unequal probability of selection of schools across regions.Finally,STATA adjusts standard errors proportional to the degree of nesting.
3. Results
Descriptive statistics for the full sample at Waves I and II and at Waves IV and V are presented in Supplementary Tables 1 and 2, respectively. Regarding 24-h movement behaviors at Waves I and II,only 2.1%of the adolescents met all 3 behaviors and 37.8% met none of them. Specifically, 20.3% of the adolescents were physically active,26.0%reported the recommended screen time use,and 36.3%of the sample reported the recommended sleep duration. At Waves IV and V, 6.7% and 7.9%of the sample were diagnosed with T2DM,respectively.
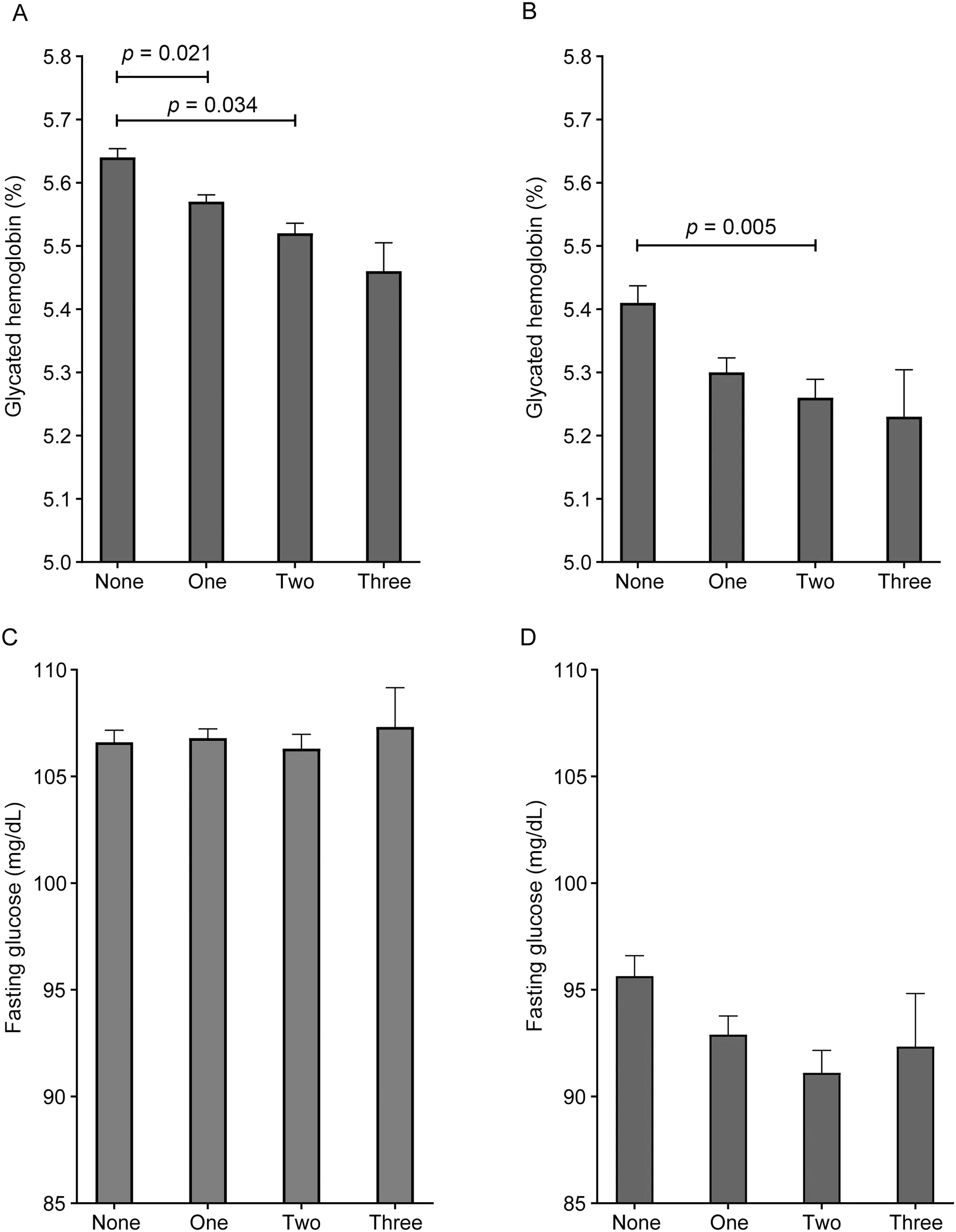
Fig.1. Differences between adolescents who met none,1,2,or 3 guidelines and log10 glycated hemoglobin(%)((A)Wave IV and(B)Wave V)and fasting glucose (mg/dL) ((C) Wave IV and (D) Wave V) in adulthood. Covariates included sex, age at follow-up, highest education achieved, race/ethnicity, alcohol consumption at follow-up, smoking habit at follow-up, hsCRP, WC at follow-up, and hypertension. To aid interpretation, data were back-transformed from the log scale for presentation in the results.hsCRP=high sensitivity C-reactive protein;WC=waist circumference.
Fig.1 reveals the differences in HbA1c and fasting glucose at Waves IV and V according to the number of 24-h movement behaviors met during adolescence. At Wave IV, adolescents who meet 1 (p=0.021) and 2 guidelines (p=0.034) showed lower HbA1c concentrations than those who did not meet any of these guidelines. At Wave V, those who met 2 guidelines showed lower HbA1c concentrations than adolescents who did not meet any of these guidelines(p=0.005).
Table 1 shows the differences in log10HbA1c and fasting glucose in adulthood between adolescents that met physical activity, screen time, and sleep duration guidelines (and combinations among them)versus those who did not.At Wave IV,adolescents who met physical activity and screen time guidelines jointly showed lower log10HbA1c than those who did not meet any of these guidelines.In addition,adolescents who met all 3 guidelines had lower log10HbA1c concentrations than those who did not meet any of these guidelines.At Wave V, adolescents who met physical activity guidelines showed lower log10HbA1c and fasting glucose than those who did not meet any of these guidelines. Also, those who met physical activity and screen time, or who met all 3 guidelines, showed lower log10HbA1c than those who did not meet any of these guidelines.
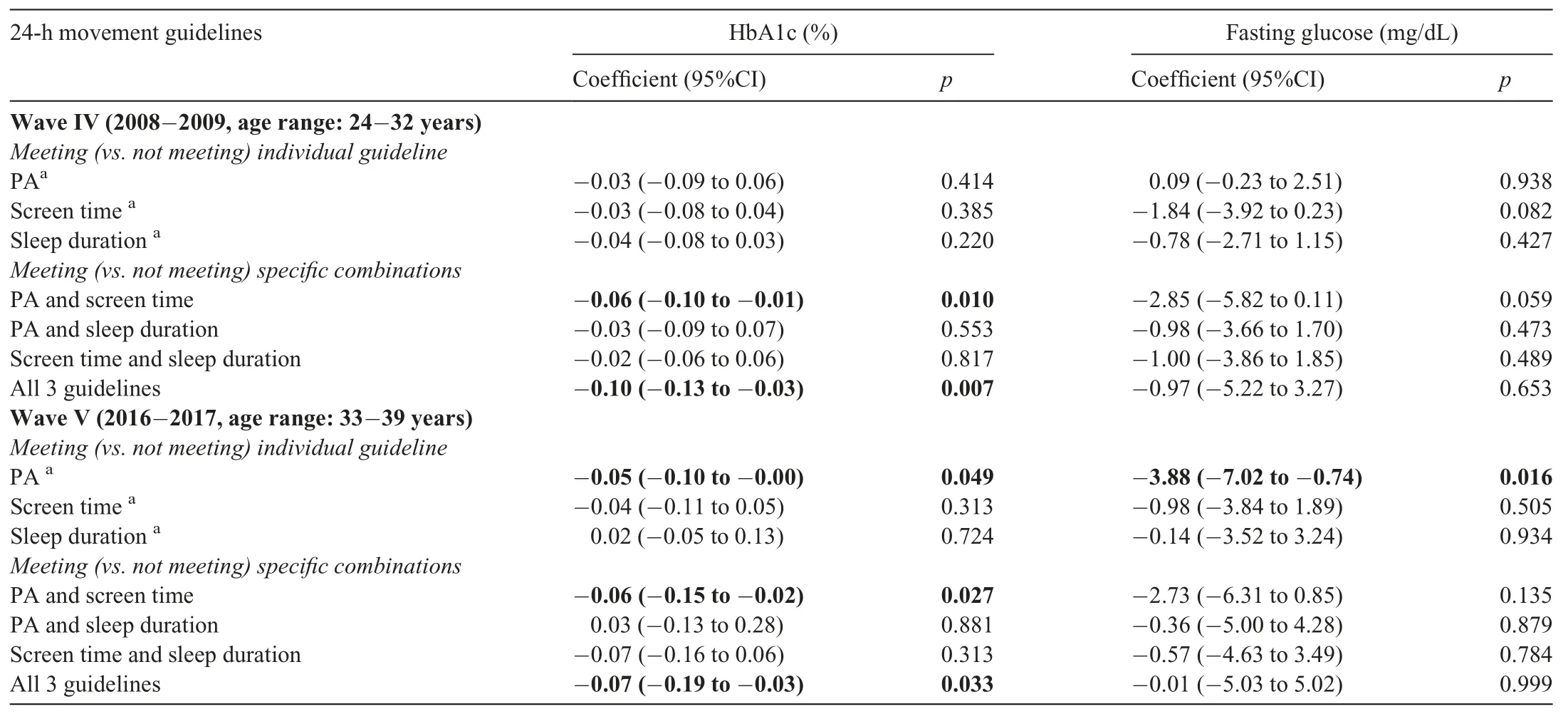
Table 1 Differences in log10 HbA1c and fasting glucose at Waves IV and V between adolescents who met vs.those who did not meet PA,screen time,and sleep duration guidelines and combinations among them.
Last,the PR for T2DM in adulthood associated with meeting vs. not meeting 24-h movement guidelines are shown in Fig. 2. In both waves, adolescents who met physical activity and screen time guidelines had lower odds of T2DM in adulthood compared to those who did not meet any of these guidelines (Wave IV: PR=0.57, 95%CI: 0.21-0.89,p=0.013;Wave V:PR=0.43,95%CI:0.32-0.74,p=0.021).At Wave V, adolescents who met all 3 guidelines had lower odds of T2DM at follow-up compared to those who did not meet any of these guidelines (PR=0.47, 95%CI: 0.24-0.91,p=0.032). Also, for each increase in meeting one of the 24-h recommendations, the odds of T2DM in adulthood decreased by 18% (PR=0.82, 95%CI: 0.61-0.99, p=0.048) and 15%(PR=0.85,95%CI:0.65-0.98,p=0.041)in Waves IV and V,respectively.
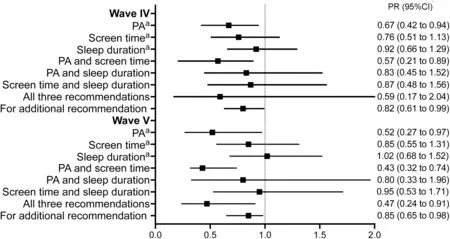
Fig.2. PRs for diagnosis of type 2 diabetes mellitus at Waves IV and V associated with meeting vs.not meeting physical activity,screen time,and sleep duration guidelines and combinations among them during adolescence.Analysis was adjusted by biological sex,race/ethnicity,age at follow-up,higher education achieved,alcohol consumption at follow-up,smoking habit at follow-up,hsCRP,WC at follow-up,and hypertension. a Mutual adjustments between physical activity,screen time,and sleep duration.95%CI=95%confidence interval;hsCRP=high sensitivity C-reactive protein;PA=physical activity;PR=prevalence ratio;WC=waist circumference.
4. Discussion
To our knowledge, this is the first prospective study that determined the relationship between meeting the 24-h movement guidelines in adolescence and glucose outcomes and risk of T2DM in adulthood, 14 and 22 years later. Overall, our results showed that meeting physical activity guidelines in isolation, jointly with screen time guidelines, and meeting all 3 guidelines during adolescence was linked to lower HbA1c concentrations and lower odds of T2DM in adulthood.In addition,for each increase in one 24-h guideline met,the odds of T2DM decreased by 15%-18%in adulthood.
According to the American Diabetes Association’s“Standards of Medical Care in Diabetes”,the 2 major goals of a diabetes prevention lifestyle intervention are to achieve andmaintain a minimum of weight loss and to increase the amount of moderate-intensity physical activity performed per week.35Specifically, the 20.3% of individuals from our sample who self-reported meeting the physical activity guideline recommendations in adolescence were less likely to have self-reported or measured T2DM in mid-adulthood, 22 years later. In accordance with the present results, a previous study has demonstrated that the MVPA levels of young adults (aged 18 years)provided protection from subsequent metabolic disease,specifically T2DM,independent of physical activity levels up through midlife.10Ekelund et al.36highlighted the importance of promoting moderate-intensity activity to improve insulin sensitivity and other metabolic risk factors and to prevent T2DM in 192 adults with a family history of diabetes. There are several biological mechanisms by which physical activity may affect glucose metabolism, including increased glucose transport into skeletal muscle through increases in Glucose transporter 4(GLUT4) protein content37and increased capacity for skeletal muscle to oxidize fat,which favors the available amount of nonesterified fatty acids to the liver and,consequently,the possible increase in hepatic insulin sensitivity.38
The American Diabetes Association statement also encourages breaking up prolonged sedentary time35as sedentary behavior is associated with abnormal glucose metabolism39and predicts T2DM.40,41In this sense, our findings suggested that,combined with physical activity,meeting the screen time guideline is related to lower HbA1c concentrations and lower odds of T2DM in adulthood.This was consistent with a previous finding from the same dataset,which showed that for adolescents with low levels of physical activity engagement,reducing sedentary behaviors is protective for T2DM during young adulthood.19Our finding also supports the results of another prospective study in this area linking youth televisionviewing behavior and raised fasting glucose in mid-adulthood.8Time spent watching television, which is the most commonly engaged in sedentary behavior in our sample (data not shown), seems to be associated with unhealthy diet;40for example,it is associated with a higher frequency of consuming discretionary foods,sugar-sweetened beverages,and takeaway foods.42This can partially explain the association between sedentary behaviors and T2DM.Another study from a population-based cohort in Northern Sweden showed that television viewing at age 16 years was associated with higher fasting glucose at age 43 years.8These results,jointly with our own,suggest that the relationship between physical activity, screen time, and cardiometabolic risk may have lasting effects from adolescence and into midlife.
A narrative review supported the contributions of sleep disorders(e.g.,alteration of sleep duration)to the development of obesity,insulin resistance, and T2DM.7In our study,sleep duration during adolescence, alone or combined with physical activity or screen time,was not associated with glucose outcomes or risk of T2DM in adulthood.This finding is consistent with that of Leppänen et al.,13who indicated that sleep duration was not prospectively related to insulin and fasting glucose concentrations in Finnish children 2 years later.In contrast, another study showed that sleep duration was associated with Homeostatic Model Assessment of Insulin Resistance after adjusting for physical activity and sedentary time over a 200-day follow-up period in a sample of Danish children.16The role of sleep quality and problems,whether combined or not with other movement behaviors,and their relationship to adult health warrants further research.
In the present study,adolescents who met 2 guidelines had lower HbA1c concentrations in adulthood than those who met 1 or no recommendations. Overall, cross-sectional studies among children and adolescents14,15confirm our finding,showing no association with glucose outcomes. Furthermore,the few existing prospective studies show contradictory findings. In accordance with the present results, 1 previous study of 485 Finnish children demonstrated that meeting all the guidelines was not associated with lower levels of fasting glucose but with lower levels of fasting insulin 2 years later.13Conversely, Hjorth et al.16reported that youth in the tertiles with the most favorable changes in relation to MVPA, sleep duration, and sedentary time during a 200-day follow-up period had remarkably lower insulin resistance compared to children in the least favorable tertiles of changes.
Finally, our study also suggested that meeting all components of the 24-h movement guidelines was associated with lower odds of T2DM at Wave V. Also, our results revealed that for each additional 24-h movement recommendation meeting,the odds of T2DM decreased by 15%-18%in adulthood. The present results are supported by a previous finding by Katzmarzyk and Staiano,14who reported that meeting several combinations of the 24-h movement behaviors was associated with lower fasting glucose levels in their cross-sectional study.Carson et al.17also showed similar results to ours,since meeting more 24-h movement behaviors was associated with lower levels of insulin(as opposed to glucose).Therefore,our overall results and previous studies support the integrated paradigm that underpins the 24-hour movement guidelines, where the focus is on the combined or synergistic effects of movement behaviors on health.20,43
There are several limitations that should be declared. First,the longitudinal study design does not allow us to establish causal-effect relationships. Second, information about movement behaviors were self-reported by adolescents,which makes them subject to bias. A stronger methodology would be more appropriate for obtaining objective measures of physical activity,sedentary behavior,and sleep duration(e.g.,accelerometers).Also,the physical activity instrument used is limited in scope since it does not include a school component and gives no indication of time, making it difficult to pinpoint whether youth met the 60 min of MVPA per day recommendation. Third, a dataset from 1994 to 1996 was used to gauge whether or not a guideline that was made later was met. Sedentary behaviors use has changed over the last 2 decades (e.g., moving from traditional television programming to streaming), which has caused an overall increase in screen time. Fourth, no data about glucose outcomes are available at adolescence and,therefore, we could not adjust the analysis for baseline levels. However, we did exclude adolescents who were diagnosed with T2DM before 18 years old.Fifth,our findings may also have been influenced by residual confounding due to the fact that confounders are not included in the regression models (e.g., diet or pubertal status)because they are not available in the Add Health. Another potential limitation could be that movement behaviors at follow-up were not included in the analysis. Sixth, at Wave IV capillary blood glucose was determined instead of other more sophisticated measures of glucose. Finally, Wave V has only 5381 participants with glucose outcomes data and,therefore,we lost a large part of the sample at follow-up. To test whether there were differences in movement behaviors between those lost vs. those retained, we conducted a x2analysis to compare adolescents who had completed all waves of data collection to those who had not completed all waves of data collection.Those who completed all waves of data collection did not report higher diagnosis of T2DM (p=0.075), physical activity (p=0.156),screen time(p=0.116),or sleep duration(p=0.540).Therefore,it does not appear that missing data meaningfully influenced results within the analytic sample.
5. Conclusion
Adolescents who jointly met physical activity and screen time recommendations were less likely to have T2DM over a 14-and 22-year follow-up period among a representative sample of US adolescents. This suggests that it may not only be important to increase participation in physical activity but also to reduce recreational screen time and other sedentary behaviors by,for example,encouraging individuals to break up prolonged periods of sedentary time.35Furthermore, meeting more components of the guidelines was associated with lower concentrations of HbA1c and lower odds of T2DM. Studies using novel statistical methodologies such as compositional analysis are needed to better clarify these relationships and to determine the potential metabolic health benefits of various combinations of movement behaviors. Also, future randomized controlled trials are warranted to explore the effects of novel strategies to simultaneously improve physical activity,sedentary time,and sleep on the risk of T2DM.
Acknowledgments
AGH is a Miguel Servet Fellow(Instituto de Salud Carlos IIIFSE-CP18/0150).JFLG is a Postdoctoral Fellow(Universidad de Castilla-La Mancha - ID 2021-UNIVERS-10414). This research received no external funding and uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J.Richard Udry,Peter S.Bearman,and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill.
Authors’contributions
AGH conceived the study,drafted the analysis plan and manuscript, and conducted statistical analyses; JFLG reviewed the analysis plan and helped to draft the manuscript; YE assisted with data cleaning and preparation and helped to draft the manuscript; MI helped to draft the manuscript; RRV helped to draft the manuscript and provided input on the analysis plan. All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interest.
Supplementary materials
Supplementary materials associated with this article can be found in the online version at doi:10.1016/j.jshs.2022.08.001.
 Journal of Sport and Health Science2023年2期
Journal of Sport and Health Science2023年2期
- Journal of Sport and Health Science的其它文章
- Exercise training-induced changes in exerkine concentrations may be relevant to the metabolic control of type 2 diabetes mellitus patients:A systematic review and meta-analysis of randomized controlled trials
- Stair climbing,genetic predisposition,and the risk of incident type 2 diabetes:A large population-based prospective cohort study
- The effects of a 20-week exercise program on blood-circulating biomarkers related to brain health in overweight or obese children:The ActiveBrains project
- Dose-dependent associations of joint aerobic and muscle-strengthening exercise with obesity:A cross-sectional study of 280,605 adults
- Chronotropic incompetence is more frequent in obese adolescents and relates to systemic inflammation and exercise intolerance
- Overweight and obesity in young adults with patellofemoral pain:Impact on functional capacity and strength
