Exercise training-induced changes in exerkine concentrations may be relevant to the metabolic control of type 2 diabetes mellitus patients:A systematic review and meta-analysis of randomized controlled trials
Antonio García-Hermoso,Robinson Ramírez-Vélez,Javier Díez,Arantxa González,Mikel Izquierdo
a Navarrabiomed,Public University of Navarra(UPNA),Health Research Institute of Navarra(IdiSNA),University Hospital of Navarra,Pamplona 310008,Spain
b CIBER of Frailty and Healthy Aging(CIBERFES),Carlos III Institute of Health,Madrid 28029,Spain
c Institute for Health Research of Navarra(IDISNA),Pamplona 31008,Spain
d Program of Cardiovascular Diseases,Center for Applied Medical Research,University of Navarra,Pamplona 31008,Spain
e Centre for Biomedical Research in Cardiovascular Disease Network,Carlos III Institute of Health,Madrid 28029,Spain
f Departments of Nephrology and Cardiology,University of Navarra Clinic,Pamplona 31008,Spain
Abstract Background:This study investigates the effects of exercise training on exerkines in patients with type 2 diabetes mellitus to determine the optimal exercise prescription.Methods:A systematic search for relevant studies was performed in 3 databases.Randomized controlled trials investigating the effects of exercise training on at least one of the following exerkines were included:adiponectin,apelin,brain-derived neurotrophic factor,fetuin-A,fibroblast growth factor-21,follistatin,ghrelin,interleukin(IL)-6,IL-8,IL-10,IL-15,IL-18,leptin,myostatin,omentin,resistin,retinol-binding protein 4,tumor necrosis factor-α,and visfatin.Results:Forty randomized controlled trials were selected for data extraction(n=2160).Exercise training induces changes in adiponectin,fetuin-A,fibroblast growth factor-21,IL-6,IL-10,leptin,resistin,and tumor necrosis factor-α levels but has no significant effects on apelin,IL-18,and ghrelin compared to controls.Physical exercise training favored large and positive changes in pooled exerkines(i.e.,an overall effect size calculated from several exerkines)(Hedge’s g=1.02,95%confidence interval(95%CI):0.76-1.28),which in turn were related to changes in glycated hemoglobin(mean difference(MD)=-0.81%,95%CI:-0.95%to-0.67%),fasting glucose(MD=-23.43 mg/dL,95%CI:-30.07 mg/dL to-16.80 mg/dL),waist circumference(MD=-3.04 cm,95%CI:-4.02 cm to-2.07 cm),and body mass(MD=-1.93 kg,95%CI:-2.00 kg to-1.86 kg).Slightly stronger effects were observed with aerobic, resistance, or high-intensity interval protocols at moderate- to vigorous-intensity and with programs longer than 24 weeks that comprise at least 3 sessions per week and more than 60 min per session.Conclusion:Exercise training represents an anti-inflammatory therapy and metabolism-improving strategy with minimal side effects for patients with type 2 diabetes mellitus.
Keywords: Adipokines;Exercise training;Hepatokines;Myokines
1. Introduction
Type 2 diabetes mellitus (T2DM) is a chronic metabolic disorder characterized by persistent hyperglycemia, and it is a leading cause of morbidity and mortality worldwide.1T2DM is estimated to affect 463 million adults between the ages of 20 and 79 (data from 2019), and this is expected to rise to>578 million by 2030.2A better understanding of the pathophysiology of T2DM and more effective methods of treating the disease are, therefore, urgently needed. According to the American Diabetes Association Professional Practice Committee, lifestyle management (e.g., weight management, physical activity) and psychosocial care are the cornerstones of T2DM management.3
Most adults with T2DM should engage in 150 min or more of moderate- to vigorous-intensity aerobic activity per week and 2-3 sessions/week of resistance exercise on nonconsecutive days.3Physical exercise activates several signaling pathways, leading to the production of the bioactive molecules responsible for the beneficial effects of physical exercise.These molecules, which are potential pharmacological targets/agents for the development of “exercise pills”, include circulating cytokines and humoral factors related to T2DM as well as “organokines”. They originate from skeletal muscle(myokines)as well as adipose tissue(adipokines)and the liver(hepatokines).Collectively,these are known as“exerkines”—a term coined by Safdar et al.4to describe the circulating factors produced and secreted by any tissue or organ that are released in response to repeated bouts of exercise. Exerkines are increasingly recognized as critical intermediaries of exercise-related changes and health benefits, mainly due to their role in inter-organ and systemic communication and coordination.5
Most of the literature associates the benefits of exerkines with aerobic exercise;6however, the effects of resistance or combined exercise (i.e., aerobic plus resistance training),intensity (i.e., light, moderate), length of program, frequency and/or duration of the session are less studied.7Furthermore,the relationship between exerkines and response in individuals with T2DM remains unexplored.The aim of the present metaanalysis was 2-fold: (a) to examine major exerkines that may serve as biomarkers for monitoring the effects of exercise on T2DM and establishing the optimal exercise prescription; and(b) to determine the association of changes in exerkines with clinical parameters such as glycated hemoglobin (HbA1c),fasting glucose, waist circumference (WC), and body mass in an effort to explore the relationship between exercise and metabolism in T2DM patients.
2. Methods
The study was conducted and reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and recommendations.8The protocol was registered in the international prospective register of systematic reviews (PROSPERO) (identification number: CRD42022283272). Two authors (AGH and RRV)independently performed the entire process, from literature selection to data extraction. Disagreements were resolved through consultation with a third researcher(MI).
2.1. Identification and selection criteria
To be eligible for inclusion in the present study,trials had to meet the following criteria (derived from the PICOS framework):(a)Participants: adults aged ≥18 years diagnosed with T2DM,excluding studies of patients with glucose intolerance,insulin resistance, or prediabetes; (b) Intervention: supervised exercise training program with a minimum duration of 2 weeks, excluding randomized controlled trials (RCTs) that used any additional diet or supplementation,such as green tea,Vitamin D, or drugs. Exercise training was defined as any body movement causing an increase in energy expenditure that involves planned or structured motion performed in a systematic manner in terms of frequency, intensity, duration,and progression and that was designed to maintain or enhance health-related outcomes according to the recommendations of the American Diabetes Association;9(c) Comparison: control group receiving ordinary care, health education, and/or placebo, excluding healthy individuals (i.e., matched controls without T2DM); (d) Outcome: included studies measured at least one of the following exerkines, all of which have previously been linked to metabolic outcomes (Supplementary Table 1): adiponectin, apelin, brain-derived neurotrophic factor (BDNF), fetuin-A, fibroblast growth factor-21 (FGF-21),follistatin,ghrelin,interleukin-6(IL-6),IL-8,IL-10,IL-15,IL-18,leptin,myostatin,omentin,resistin,retinol-binding protein 4 (RBP4), tumor necrosis factor-α (TNF-α), and visfatin; and(e)Study design:RCTs.
2.2. Search strategy
We performed an electronic search of PubMed, Embase,and Web of Science from inception to December 2,2021.The search strategy was supplemented with manual searches of the existing literature and combined the following MeSH terms:“exercise” and “myokines” and “cytokines” and “adipokines”and “hepatokines” and “type 2 diabetes” (Supplementary Method 1). We also used the aforementioned “exerkines” as search terms. Two authors (AGH and RRV) independently assessed titles,abstracts,and full texts for eligibility for potential inclusion.
2.3. Data collection process
Two authors(AGH and RRV)independently extracted data from each RCT and collected the following information: (a)study design:authors’names,year of publication,and country of the study;(b)participants:sample size,sex,age,and characteristics for all groups; (c) intervention: exercise modality,length(weeks),frequency(sessions/week),duration of training(minutes/session), and intensity of training; and (d) outcome data for each group regarding exerkines of interest and secondary outcomes (i.e., HbA1c, fasting glucose, WC, and body mass).When there was insufficient information,the authors of the included study were contacted. After extraction, a third reviewer (MI) examined the data for completeness and accuracy.Disagreements were resolved by review of the trial report and discussion.
2.4. Assessment of methodological quality and completeness of reporting
Methodological quality was appraised using Physiotherapy Evidence Database criteria,10an 11-item scale designed for rating the methodological quality of RCTs. Two authors(AGH and RRV) independently scored each study, with disagreements resolved by consensus with a third investigator(MI).Physiotherapy Evidence Database scores of 0-3 are considered poor,4-5 fair,6-8 good,and 9-10 excellent.11
The Grading of Recommendations, Assessment, Development,and Evaluation(GRADE)approach was used to evaluate the quality of the evidence of the overall effect.
2.5. Data synthesis and analysis
All analyses were carried out with STATA software using admetan and lfk modules(Version 17;StataCorp.,College Station,TX,USA).We implemented the random-effects inversevariance model with the Hartung-Knapp-Sidik-Jonkman adjustment.Changes in exerkines were calculated by subtracting change differences between the exercise and control groups,using the pooled standard deviation(SD)of change in both groups. If change score SDs were not available, they were calculated from pre-SD and post-SD values along with 95%confidence intervals(95%CIs)for either change outcome or exercise training effect differences.12When the data were shown only by figures,Webplotdigitizer 4.3 software(Version 4.3; https://automeris.io/WebPlotDigitizer/) was used to extract them.Effect size was expressed as Hedge’s g to correct for possible small sample bias.13When a study included more than 2 arms in comparison with a control group,we halved the number of participants in the control group for each of the comparisons.
Meta-analyses were performed for each exerkine that was included in 3 or more RCTs. For this reason, we were unable to pool data for BDNF, follistatin, ghrelin, IL-15, myostatin,omentin,and RBP4.
We also determined the overall effect size(hereafter called pooled exerkines) by considering the following aspects: (a)when exercise typically favors a reduction in the exerkine(e.g.,exercise has been shown to reduce IL-6 and TNF-α levels in patients with T2DM14), we changed the direction of effect size to ensure the same direction for all exerkines. This resulted in a change of direction for fetuin-A,IL-6,IL-18,leptin,myostatin,resistin,visfatin,and TNF-α in each study(i.e.,negative effect sizes were changed to positive and vice versa);and (b) when a study included several exerkines (e.g., leptin,adiponectin),we used only the larger effect size to avoid duplication(i.e.,the same group appearing on 2 or more occasions).
Using the pooled exerkines, subgroup analyses were performed according to type of exercise training (aerobic, highintensity interval training, resistance, and both (concurrent)),intensity (using the categories of the American College of Sports Medicine: light, moderate, moderate to vigorous, and vigorous),7,15length of program (<24 or ≥24 weeks), frequency (≤3 or >3 sessions per week) and duration of session(<60 and ≥60 min per session).
Meta-regression analyses were performed to evaluate the association between changes in exerkines and changes in HbA1c (%), fasting glucose (mg/dL), WC (cm), and body mass (kg). When possible, associations between changes in exerkines were analyzed.The following associations were possible: adiponectin/leptin, adiponectin/resistin, IL-6/TNF-α,and FGF-21/fetuin-A.
Heterogeneity across studies was calculated using the inconsistency index (I2), which is derived from the Cochran Q statistic:160%-40%, negligible heterogeneity; 30%-60%,moderate heterogeneity;50%-90%,substantial heterogeneity;and 75%-100% considerable heterogeneity. Lastly, smallstudy effects and publication bias were examined using the Doi plot and the Luis Furuya-Kanamori index.17Luis Furuya-Kanamori values beyond±1 are considered to be indicative of minor asymmetry; values ± 2 indicate major asymmetry and suggest the presence of publication bias.17
3. Results
3.1. Study selection
From the retrieved articles, a total of 40 RCTs18-58were included in the present study (Fig. 1). Four RCTs used the same control group50,51or sample.21,23Two others were included only in the systematic review due to lack of data needed to calculate an effect size.44,48Reasons for exclusion are shown in Supplementary Method 2 in the Supplementary Materials.
3.2. Characteristics of included trials
The study characteristics are summarized in Supplementary Table 2.
The study included a total of 2160 individuals with T2DM(1281 in the exercise groups and 879 in the control groups).Seven studies included only men19,24,27,38,40,42,45and 9 included only women.21,23,29,39,49-51,54,56Interventions included aerobic exercise (n=639), high-intensity interval training (n=95), resistance exercise (n=255), concurrent training (n=343), or several arms with the aforementioned protocols. Exercise training duration ranged from 8 weeks to 96 weeks,40and training frequency ranged from 132to 526,28,39,51,51times weekly, with sessions from 15 min20,41to 75 min43in duration.
Of the 40 studies, 15 RCTs analyzed adiponectin,19,22,24,25,28,31-34,39,43,47,49,53,54 3 apelin,21,36,372 BDNF,44,484 fetuin-A,38,50,51,536 FGF-21,29,38,42,45,50,511 follistatin,4212 IL-6,18,19,22,23,26,27,31,32,34,41,46,583 ghrelin,36,37,571 IL-8,183 IL-10,22,33,351 IL-15,233 IL-18,33,35,5210 leptin,19,22,24,28,39,40,43,47,49,53 2 myostatin,42,451 omentin,542 RBP4,19,394 resistin,22,31,34,5312 TNF-α,18-20,22,27,30,31,33,34,41,57,58and 3 visfatin31,37,56(Supplementary Table 2).
Most of the RCTs did not relate information about side effects. Those studies that did report no major adverse effects or health problems attributable to the assessments or training sessions.19,22,53,23,32-37,49However, 3 studies reported postexercise hypoglycemic events28,31or minor injuries.41
3.3. Methodological quality within studies
The methodological quality assessment using the Physiotherapy Evidence Database scale showed a mean score of 4.8 out of a possible 10 points, with a range of 3 points46to 7 points25,27(Supplementary Table 3).
Overall, the quality of evidence (GRADE) for each pooled estimate comparing exercise protocols with the control group was low quality(Supplementary Table 4).

Fig.1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses(PRISMA)flow diagram.
3.4. Effect estimates of exercise training on exerkines
Meta-analysis indicated that physical exercise training induces an increase in adiponectin (p=0.008), FGF-21(p=0.022), and IL-10 (p=0.041) levels and a decrease in fetuin-A(p=0.001),IL-6(p<0.001),leptin(p=0.001),resistin (p=0.012), TNF-α (p < 0.001), and visfatin (p=0.045).No significant changes were found in apelin(p=0.170),IL-18(p=0.127), and ghrelin (p=0.725) levels in comparison with the control groups(Table 1).
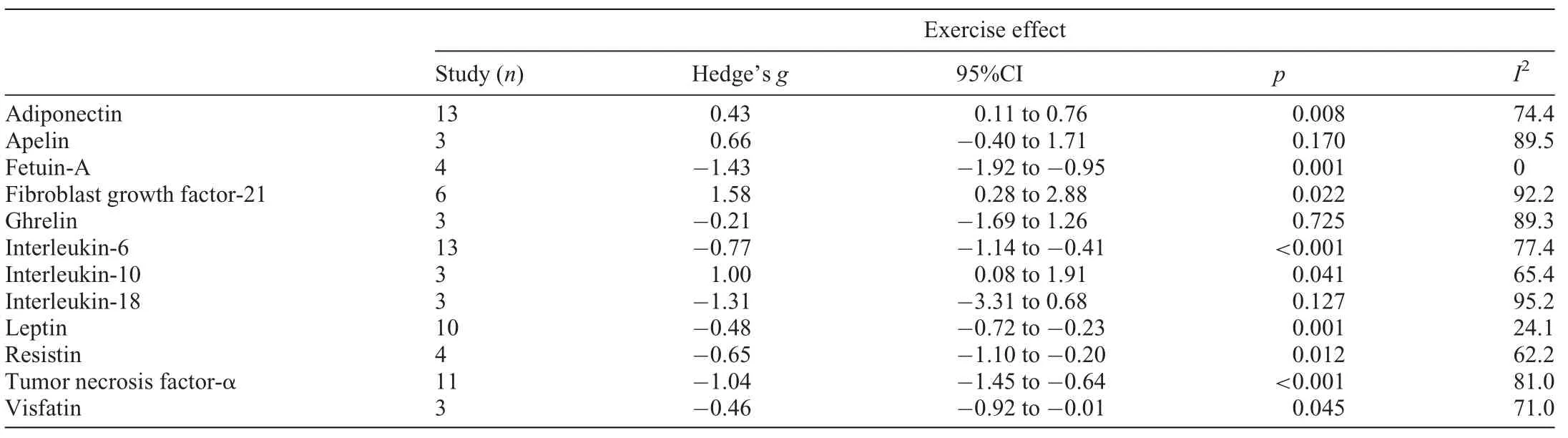
Table 1 Effect of exercise programs on different exerkines in patients with type 2 diabetes mellitus.
Of note, meta-analysis also demonstrated that physical exercise training favored a reduction in HbA1c (mean difference (MD)=-0.81%, 95%CI: -0.95% to -0.67%, p <0.001, I2=93.3%) (Supplementary Fig. 1), fasting glucose(MD=-23.43 mg/dL, 95%CI: -30.07 mg/dL to-16.80 mg/dL, p < 0.001, I2=92.5%) (Supplementary Fig.2),WC(MD=-3.04 cm,95%CI:-4.02 cm to-2.07 cm,p<0.001, I2=0%) (Supplementary Fig. 3), and body mass(MD=-1.93 kg, 95%CI: -2.00 kg to -1.86 kg, p < 0.001,I2=0%) (Supplementary Fig. 4), as well as large and positive changes in pooled exerkines (Hedge’s g=1.02, 95%CI:0.76-1.28,p<0.001,I2=84.14%)(Fig.2).
No asymmetry suggestive of small-study effects was observed(Luis Furuya-Kanamori index=1.90)(Supplementary Fig.5).
Fig. 3 depicts the effect of exercise on pooled exerkines in patients with T2DM according to different characteristics of the programs. Subgroup analysis showed similar effects according to type of exercise(aerobic training:Hedge’s g=1.06,95%CI:0.70-1.42,p<0.001,I2=83.5%;high-intensity interval training: Hedge’s g=1.09, 95%CI: 0.34-1.83, p=0.011,I2=66.1%; resistance training: Hedge’s g=0.91, 95%CI:0.01-1.87, p=0.039, I2=88.6%; concurrent training: Hedge’s g=1.03, 95%CI: 0.54-1.52, p < 0.001, I2=83.8%) (p difference between type of exercise 0.975), intensity (moderate:Hedge’s g=1.01, 95%CI: 0.55-1.48, p=0.001, I2=85.0%;moderate to vigorous: Hedge’s g=1.05, 95%CI: 0.59-1.52, p< 0.001, I2=84.7%; vigorous: Hedge’s g=0.83, 95%CI:0.37-1.30, p=0.001, I2=80.2%) (p difference between intensity of the program 0.054), length of intervention (<24 weeks:Hedge’s g=1.00, 95%CI: 0.69 -1.33, p < 0.001, I2=83.6%;≥24 weeks: Hedge’s g=1.06, 95%CI: 0.59-1.53, p < 0.001,I2=86.7%) (p difference between length of the programs 0.844),and frequency per week(≤3 sessions per week:Hedge’s g=1.07, 95%CI: 0.74-1.40, p < 0.001, I2=85.2%; >3 sessions per week: Hedge’s g=0.88, 95%CI: 0.47-1.29, p <0.001,I2=81.0%) (p difference between frequency of exercise per week 0.398). Sessions equal to or longer than 60 min(Hedge’s g=1.30, 95%CI: 0.82-1.78, p < 0.001, I2=88.2%)showed a greater effect size than sessions less than 60 min(Hedge’s g=0.81, 95%CI: 0.52-1.10, p < 0.001, I2=76.7%)(p difference between duration of the session p=0.033).
3.5. Changes in clinical parameters according to changes in exerkines
3.5.1. HbA1c
The meta-regression model showed positive(IL-6:β=0.44,p=0.012; leptin: β=0.97, p=0.009; resistin: β=1.24,p=0.001; TNF-α: β=1.52, p < 0.001) and negative (adiponectin: β=-0.49, p=0.014; apelin: β=-2.25, p < 0.001)associations between the decrease in each exercise factor and the decrease in percentage of HbA1c(Table 2).
3.5.2. Fasting glucose
The meta-regression model showed positive (resistin:β=0.04, p=0.003; TNF-α: β=0.02, p=0.049; visfatin:β=0.02, p=0.001) and negative (apelin: β=-0.03, p <0.001;FGF-21:β=-0.02,p=0.042)associations between the decrease in exerkines and changes in fasting glucose(Table 2).
3.5.3. WC
The meta-regression model showed positive (leptin:β=0.31, p=0.010; resistin: β=0.30, p=0.040; TNF-α:β=0.30,p=0.006)and negative(adiponectin:β=-0.58,p<0.001) associations between changes in the aforementioned exerkines and changes in WC(Table 2).
3.5.4. Body mass
The meta-regression model showed positive associations between changes in IL-6 (β=0.47, p < 0.001) and TNF-α(β=0.36, p=0.029) and changes in body mass (Table 2).Regarding pooled exerkines, the meta-regression models showed a negative association between the changes in exerkines and changes in HbA1c (β=-0.31, 95%CI: -0.51 to-0.11, p =0.003) (Supplementary Fig. 6), WC (β=-0.38,95%CI: -0.58 to -0.18, p=0.001) (Supplementary Fig. 7),and body mass (β=-0.11, 95%CI: -0.20 to -0.03,p=0.006) (Supplementary Fig. 8), but not in fasting glucose(β=-0.01,95%CI:-0.02 to 0.03,p=0.723)(Supplementary Fig.9).
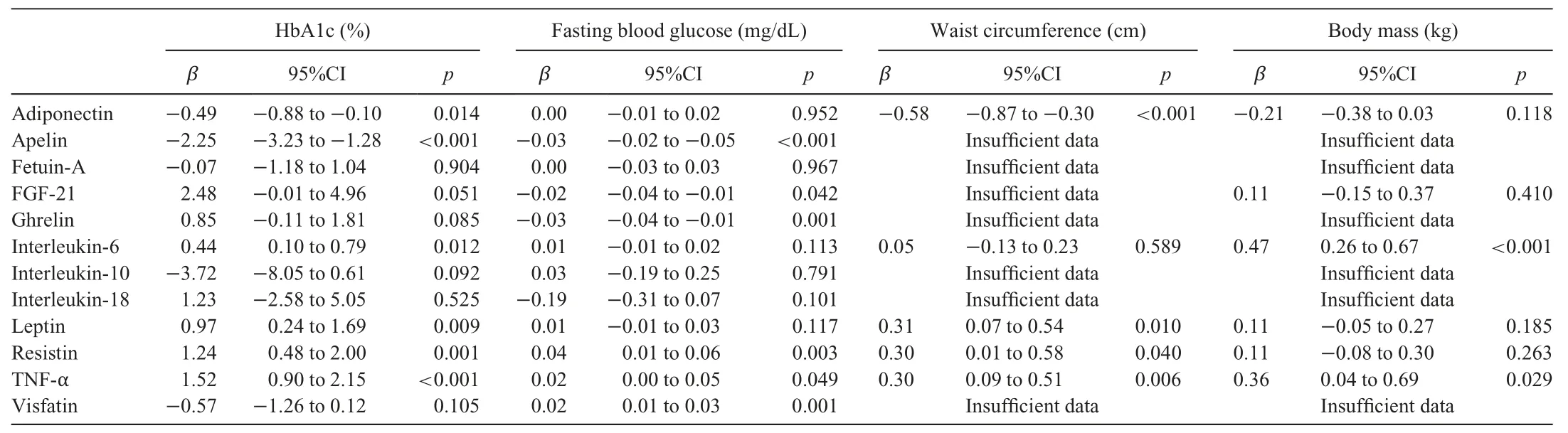
Table 2 Associations between changes in exerkines and changes in clinical outcomes(HbA1c,fasting glucose,waist circumference,and body mass).
3.6. Associations between changes in exerkines
The meta-regression model showed a positive association between the changes in adiponectin/leptin (β=-1.35, p <0.001) (Supplementary Fig. 10) and IL-6/TNF-α (β=0.34,p=0.010) (Supplementary Fig. 11), respectively. The metaregression model also showed that there is no association between the changes neither in adiponectin/resistin(β=-0.40, p=0.085) (Supplementary Fig. 12), nor in FGF-21/fetuin-A(β=-1.04,p=0.208)(Supplementary Fig.13).
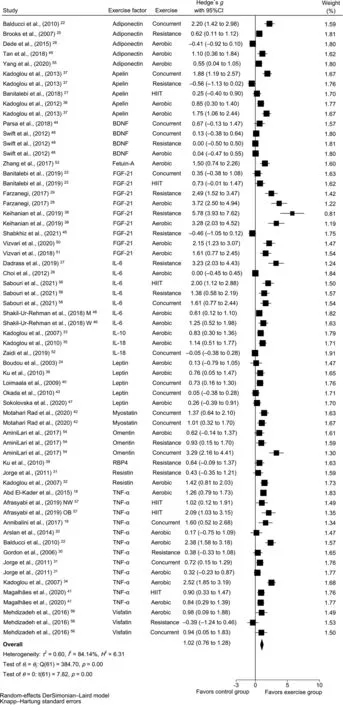
Fig. 2. Effects of exercise interventions on pooled exerkines in patients with type 2 diabetes mellitus. 95%CI=95% confidence interval; BDNF=brain-derived neurotrophic factor; FGF-21=fibroblast growth factor-21; HIIT=high intensity interval training; IL-6=interleukin-6; M=men; NW=normal weight;OB=obese;RBP4=retinol-binding protein 4;TNF-α=tumor necrosis factor-α;W=women.
4. Discussion
In the last decade, an increasing number of clinical studies have demonstrated that the benefits of exercise training programs are at least partly the result of inter-tissue communication via exerkines (e.g., metabolites, hormones, myokines,microRNAs, and/or extracellular vesicles). Indeed, a single session of aerobic exercise was found to change the expression of ~9800 molecular analytes in systemic circulation,including transcripts,proteins,metabolites,and lipids.59Inter-organ signaling from skeletal muscle is found throughout the body,including in fat, liver, pancreas, bone, heart, immune, and brain cells.60The notion that exerkines facilitate beneficial cross-talk among diverse organs and tissues has begun to be incorporated into treatment paradigms for T2DM.61
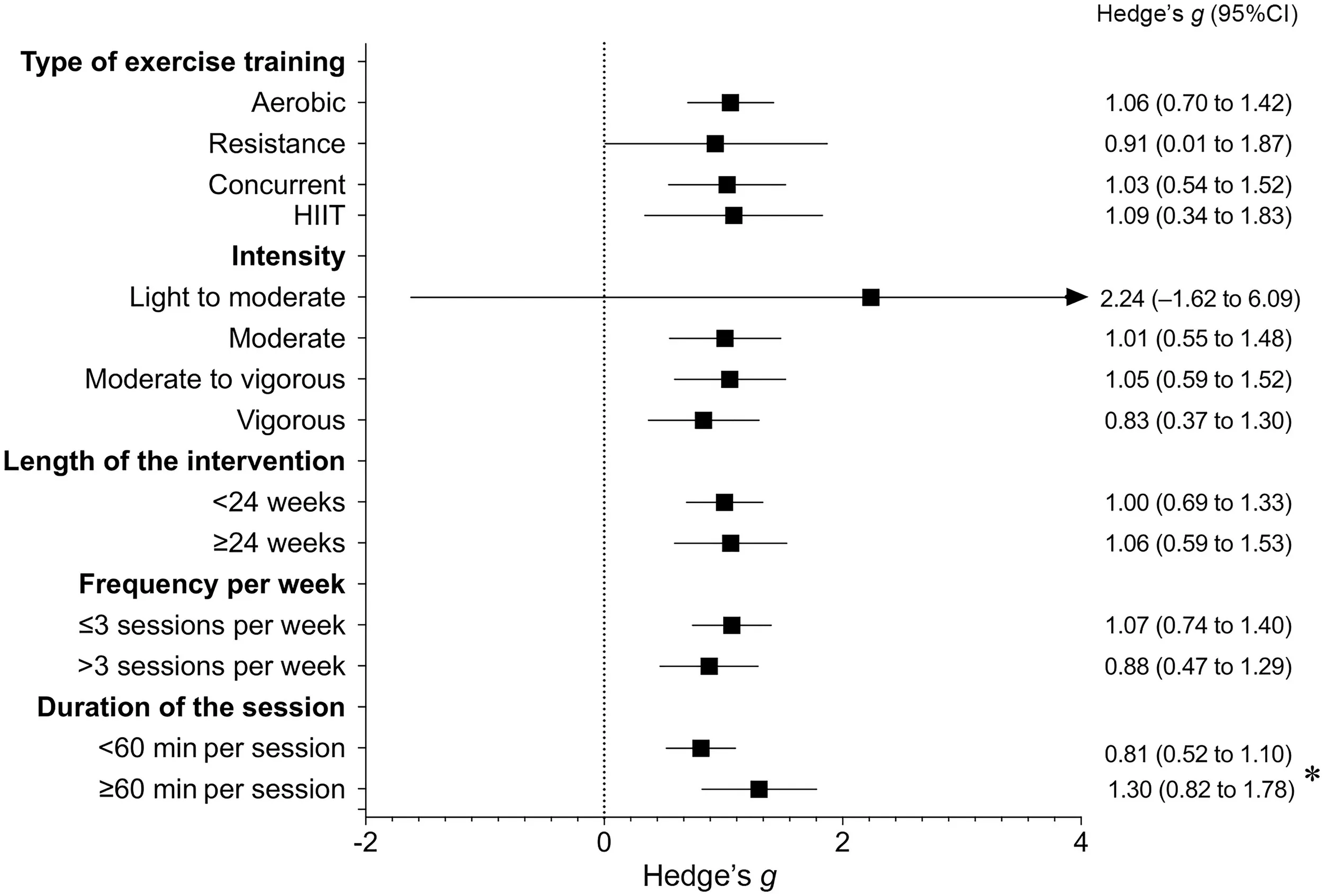
Fig.3. Overall effect of exercise on pooled exerkines in patients with type 2 diabetes mellitus according to different characteristics of the programs.*Difference between groups p=0.033.95%CI=95%confidence interval;HIIT=high intensity interval training.
Our meta-analytic approach allowed us to generate novel evidence showing that any form of regular exercise changes the circulatory blood levels of several exerkines,including adiponectin, fetuin-A, FGF-21, IL-6, IL-10, leptin, resistin, and TNF-α,in patients with T2DM as compared to control groups.In this context, our results suggest that exerkines have utility as potential biomarkers and/or therapeutic targets to treat T2DM and associated metabolic complications.This is in line with the strong body of evidence demonstrating that exercise is an effective strategy for the treatment of insulin resistance and T2DM.62
Most of the data in the present study were obtained for the effect of exercise on IL-6 levels.18,19,22,23,26,27,31,32,34,41,46As a multifunctional cytokine, IL-6 has been implicated in the development of insulin resistance in T2DM63through the generation of inflammation and control of cell differentiation,migration, proliferation, and apoptosis.64Contrastingly, as a paradigmatic myokine, IL-6 is also thought to induce an antiinflammatory cascade by triggering the release of antiinflammatory cytokines.65Similar to the results for IL-6, we found that chronic exercise reduced levels of IL-18 and TNF-α.On this basis we hypothesize that therapeutically targeting inflammatory pathways may improve glycemic control and reduce the risk of complications in people with T2DM.66
Another novel finding from our meta-analysis was the positive effect exercise training had by decreasing the levels of fetuin-A,leptin,and resistin,which are broadly involved in obesity and related disorders,including T2DM,non-alcoholic fatty liver disease, and metabolic syndrome. Recently, Ramírez-Vélez et al.67reported that exercise reduces fetuin-A levels in obesity, T2DM, and cardiovascular disease in adults and the elderly. The authors concluded, however, that these effects should be interpreted with caution because of the variety of exercise types investigated and the involvement of differentobesity-related disorders.Our meta-analysis revealed that exercise training decreased leptin levels in adults with T2DM,which is in line with a previous meta-analysis done by Becic et al.,68who reported that physical exercise reduces leptin levels in prediabetic and diabetic individuals. Resistin is an emerging cardiovascular risk factor implicated in T2DM.69Contrary to other reports,70,71we found that exercise induced a considerable decrease in resistin levels. Kadoglou et al.32showed that a 16-week aerobic exercise training program of four 45-60-min sessions per week (50%-85% maximum oxygen consumption)might exert pleiotropic cardioprotective actions by modifying the expression of certain inflammatory cytokines, including resistin, in patients with T2DM. Following training, the reduction in resistin was associated with alterations in the level of high-sensitivity C-reactive protein, IL-18, and in maximum oxygen consumption. Interestingly, in our analysis, exerciseinduced changes in resistin were positively related to changes in HbA1c and WC, suggesting an alternative explanation for the metabolic control in patients with T2DM.
It is well-recognized that hypoadiponectinemia (low levels of serum adiponectin)is associated with impaired glucose regulation, inflammation, obesity, atherosclerosis, and T2DM.72Our meta-analysis revealed that overall physical exercise increased adiponectin levels,although significant study heterogeneity was evident.Notably,high heterogeneity for adiponectin levels was also found in previous meta-analyses.68,73However, our meta-regression model also showed an association between the changes in adiponectin levels and changes in glycemic control based on HbA1c (and on WC). It is wellknown that circulating adiponectin levels decrease with increasing levels of insulin resistance.74This relationship was confirmed by Yamamoto et al.,75who also showed that nearly 90%of patients who developed diabetes after a 3-year followup had prediabetes at baseline (fasting glucose ≥110 mg/dL and/or HbA1c ≥6.0%).
Evidence indicates that TNF-α is involved in the development and/or progression of T2DM.76Overall, we found that physical exercise led to a significant decrease in serum TNF-α levels; however, significant study heterogeneity was present.This heterogeneity can likely be explained by the wide range of characteristics of both exercise programs and patients across studies.A study by Timper et al.77indicated that IL-6 inhibits TNF-α production and may contribute to the stimulation of peripheral insulin sensitivity.Clinical studies have shown that FGF-21 analogs improve dyslipidemia in obese patients with T2DM.78In addition to activating autophagy genes and improving inflammation, FGF-21 can also regulate glucose and lipid metabolism by controlling metabolism-related genes,such as adipose triglyceride lipase and acetyl-CoA carboxylase.79FGF-21 is predominantly expressed in the liver,but it is also found in adipose tissue and, to a lesser extent, skeletal muscle in physiological conditions.80Strikingly, our metaanalysis revealed that exercise decreased FGF-21 levels but,again,significant study heterogeneity was found.In a study of obese individuals and patients with T2DM,Sabaratnam et al.81reported that a single 1-h bout of acute exercise increased the muscle mRNA and circulating levels of FGF-21 immediately after exercise, and both remained elevated 3 h into recovery without differences between the 2 groups. Other studies have reported an attenuated plasma FGF-21 response to acute exercise in obese individuals82and in patients with T2DM.83Thus,FGF-21 appears to be an important exercise factor that might play a key role in tissue crosstalk and promote the beneficial effects of exercise on whole-body metabolism; however, the mechanisms have yet to be unraveled.
Overall, the results of this meta-analysis suggest that exercise training-induced changes in exerkines concentrations may be relevant in the metabolic control of T2DM due to their multisystemic benefits. Fig. 4 illustrates how exercise programs favor changes in exerkines concentration among patients with T2DM. However, much of the regulation by exercise of these exerkines remains unexplored, and there are still several challenges to their validation and translation into clinical practice.Therefore, it will be necessary for the treatment of T2DM patients to clarify these aspects and determine the molecular contribution of personalized patterns of physical exercise.
5. Strengths and limitations
To the best of our knowledge,this is the first meta-analysis to examine the efficacy of several types of exercise training protocols(and doses)on 19 exerkines in patients with T2DM.A strength of the present study is that we determined the therapeutic potential of exerkines and their association with clinical parameters, such as metabolic control measured by HbA1c,fasting glucose, WC, and body mass. These exerkines could emerge as biomarkers or as preventative or therapeutic targets for T2DM.However,we recognize that there are some limitations to our findings.First,significant heterogeneity was found in the results for apelin, FGF-21, IL-6, IL-18, TNF-α, and pooled exerkines,which may be due to differences in methodology, participation criteria (e.g., age, years diagnosed with T2DM),and exercise training protocols;however,we did perform subgroup analyses to account for heterogeneity among RCTs. Second, not all RCTs included data on clinical outcomes (i.e., HbA1c, fasting glucose, WC, and body mass),thus our meta-regression analyses should be interpreted with caution.Also,substantial heterogeneity in the main results and in subgroup analyses generated uncertainty about the real change in magnitude that exerkines can produce in patients with T2DM. Finally, the quality of evidence in the overall analysis was determined to be low according to GRADE criteria.
In conclusion,this meta-analysis identified an optimal dosage for exercise prescription(any form of exercise at moderate and/or vigorous intensity with a program lasting longer than 24 weeks,with at least 3 sessions per week,≥60 min per session)to induce significant improvements in exerkines in adults living with T2DM. In turn, these changes are associated with improvements in clinical metabolic parameters. Therefore,exerkines may emerge as biomarkers for monitoring the effects of exercise and as potential novel therapeutic targets.While the quality of evidence in the overall analysis was determined to be low,clinicians could consider these findings when prescribing exercise for patients with T2DM in order to ensure optimal effectiveness.

Fig.4. The effects of physical exercise on the regulation of exerkines.↑=increase;↓=decrease.
Acknowledgment
AGH is a Miguel Servet Fellow (Instituto de Salud Carlos III-CP18/0150).
Authors’contributions
AGH and RRV were responsible for the conceptualization and design of the systematic review and meta-analysis, the screening process, data collection and extraction, risk of bias assessment, and data analysis, as well as the drafting of the original version of the manuscript; MI conceived the study,participated in its design, conducted the search and identification of studies,checked the information in the selected articles,and helped to draft the manuscript in its initial and post-review versions;JD and AG were responsible for drafting and revising the manuscript. All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Supplementary materials
Supplementary materials associated with this article can be found in the online version at doi:10.1016/j.jshs.2022.11.003.
 Journal of Sport and Health Science2023年2期
Journal of Sport and Health Science2023年2期
- Journal of Sport and Health Science的其它文章
- Stair climbing,genetic predisposition,and the risk of incident type 2 diabetes:A large population-based prospective cohort study
- Twenty-four-hour movement guidelines during middle adolescence and their association with glucose outcomes and type 2 diabetes mellitus in adulthood
- The effects of a 20-week exercise program on blood-circulating biomarkers related to brain health in overweight or obese children:The ActiveBrains project
- Dose-dependent associations of joint aerobic and muscle-strengthening exercise with obesity:A cross-sectional study of 280,605 adults
- Chronotropic incompetence is more frequent in obese adolescents and relates to systemic inflammation and exercise intolerance
- Overweight and obesity in young adults with patellofemoral pain:Impact on functional capacity and strength
