Oncologic impact of colonic stents for obstructive left-sided colon cancer
Hideyuki Suzuki,Shingo Tsujinaka,Yoshihiro Sato,Tomoya Miura,Chikashi Shibata
Hideyuki Suzuki,Shingo Tsujinaka,Yoshihiro Sato,Tomoya Miura,Chikashi Shibata,Department of Gastroenterological Surgery,Tohoku Medical and Pharmaceutical University,Sendai 983-8536,Miyagi,Japan
Abstract Colonic stenting has had a significant positive impact on the management of obstructive left-sided colon cancer(OLCC)in terms of both palliative treatment and bridge-to-surgery(BTS).Notably,many studies have convincingly demonstrated the effectiveness of stenting as a BTS,resulting in improvements in shortterm outcomes and quality of life,safety,and efficacy in subsequent curative surgery,and increased cost-effectiveness,whereas the safety of chemotherapy after stenting and the long-term outcomes of stenting as a BTS are controversial.Several studies have suggested an increased risk of perforation in patients receiving bevacizumab chemotherapy after colonic stenting.In addition,several pathological analyses have suggested a negative oncological impact of colonic stenting.In contrast,many recent studies have demonstrated that colonic stenting for OLCC does not negatively impact the safety of chemotherapy or long-term oncological outcomes.The updated version of the European Society of Gastrointestinal Endoscopy guidelines released in 2020 included colonic stenting as a BTS for OLCC as a recommended treatment.It should be noted that the experience of endoscopists is involved in determining technical and clinical success rates and possibly oncological outcomes.This review discusses the positive and negative impacts of colonic stenting on OLCC treatment,particularly in terms of oncology.
Key Words:Colonic stents;Obstructive left-sided colon cancer;Bridge to surgery;Chemotherapy;Long-term outcomes;European Society of Gastrointestinal Endoscopy guidelines
INTRODUCTION
Colorectal cancer remains one of the most common malignant diseases worldwide.Among all patients with colorectal cancer,approximately 10% present with large bowel obstruction[1].The most common location for obstructive colon cancer(OCC)is the sigmoid colon,and more than 75% of OCC are located on the left side,i.e.,distal to the splenic flexure[2].
Emergency surgery(ES)has traditionally been the mainstay of OCC management.There are several options for ES procedures to treat obstructive left-sided colon cancer(OLCC);however,a stoma is often needed in any case.Patients with clinically severe instability or in whom resection is not possible should be treated with diverting loop colostomy[3].Hartmann’s procedure,that is,resection of the diseased colon or rectum with end colostomy,has been widely performed for resectable OLCC[4].Resection with primary anastomosis could be considered an option during ES for resectable cases;due to the risk of anastomotic leakage,a temporary diverting stoma can be created simultaneously in many cases.However,the reversal rate of stomas is relatively low when created under these conditions.Öistämöet al[5]retrospectively analyzed acute cases of OLCC and demonstrated that 35% of stomas created with the intention of being temporary were never reversed.Stomas can have a negative impact on the patient’s body image and quality of life(QOL).Additionally,diverting stoma formation in colorectal resection for OCC is related to increased postoperative complications,failure to wean off the ventilator,and longer hospital stays[6].
Colonic stenting is a powerful modality for intestinal decompression to resolve problems associated with ES.In addition,recent advances in stent technology have profoundly impacted OLCC management.Herein,we review the current state of colonic stenting and discuss its impact on colorectal cancer treatment,particularly focusing on its relationship with oncology.
HISTORY AND INDICATION
Palliative purpose and bridge to surgery
There are two main purposes of colonic stenting for OCC:palliative treatment and bridge to surgery(BTS).In this context,palliative treatment involves stenting applied to patients with an unresectable lesion,while BTS comprises preoperative stenting for intestinal decompression until the condition suitable for curative surgery is improved[7].In comparison,colonic stenting for palliative purposes has a long history of use.Colonic stents were first reported by Dohmotoet al[8]in 1991.This study reported using stents for palliative treatment of OCC.Since then,many studies have elucidated the usefulness of colonic stents for palliative treatment in patients requiring intestinal decompression.In addition,the effectiveness of short-term outcomes of stent placement for unresectable colorectal cancer has been widely recognized,at least in the late 20thcentury[9,10].
Recently,self-expandable metallic stents(SEMS)as BTS have been widely used.Relief from obstruction with BTS enables restoration of dilated intestinal conditions prior to surgery,decreases mortality and morbidity,avoids stoma,and improves the quality of life[11].Importantly,colonic stenting as a BTS should be performed under strict indications compared with stenting for palliative treatment,as BTS ultimately aims at a radical cure and requires long-term safety.
Left-sided vs right-sided colon
Stents can be placed not only in the left-sided colon but also in the right-sided colon.Although some reports have suggested that obstructive right-sided colonic cancer is also a good indication of SEMS,the effectiveness of SEMS for right-sided colonic obstruction has been less reported than that for left-sided colonic obstruction[9].Moritaet al[12]analyzed the advantages of SEMS as a BTS over primary surgery in a retrospective,multicenter cohort study.When patients with left-sided colon cancer were compared,the rates of primary resection with anastomosis and stoma-free surgery were significantly higher in the SEMS group,whereas when patients with right-sided colon cancer were compared,no significant difference in the rates was observed between the SEMS and primary surgery groups.In addition,several disadvantages of SEMS placement in the right-sided colon have been pointed out,including a lower technical success rate and longer procedure time[13-15].The authors of the European Society of Gastrointestinal Endoscopy(ESGE)guidelines also suggested the difficulty of stenting in the colon proximal to the splenic flexure and emphasized that SEMS recommendations should be applied to leftsided colon cancer[16].
TECHNICAL AND CLINICAL SUCCESS RATES
Recent studies have reported high technical and clinical success rates of SEMS placement for OCC.In a meta-analysis published in 2021,Neoet al[17]examined the technical and clinical success rates of SEMS for colorectal obstruction.In this study,technical success was defined as successful placement and deployment of the stent,and clinical success was defined as colonic decompression within 96 h after the stent was successfully placed.The technical and clinical success rates of SEMS were 92% in 1550 patients[95% confidence interval(CI):0.88-0.95]and 82% in 1105 patients(95%CI:0.77-0.87),respectively.In another meta-analysis published in 2021,the success rates were compared between SEMS and transanal decompression tubes(TDT).The overall success rates of SEMS and TDT were 92.1% and 71.9%,respectively,and both the technical and clinical success rates of SEMS were significantly better than those of TDT[18].
Some reports have suggested that technical and clinical success rates depend on the operators’ experience,with experience of at least 20-30 cases required to ensure safety and effectiveness[15,19].In addition,Boyleet al[20]identified short strictures and wide angulations distal to the stricture as factors indicating successful stenting in colonic obstruction.A post hoc analysis of a multicenter clinical trial in Japan identified several factors related to the difficulty of SEMS placement,including peritoneal carcinomatosis or expansive strictures[13].
The Japan Colonic Stent Safe Procedure Research Group proposed a scoring system for the clinical features of colorectal obstruction according to the patient’s oral intake status,termed the ColoRectal Obstruction Scoring System(CROSS).This system scores patients on a scale of 0-4 as follows:0,requiring continuous decompression;1,no oral intake;2,liquid or enteral nutrition;3,oral intake of soft solids,low-residue diet,or full diet with symptoms of stricture;and 4,oral intake of soft solids,lowresidue diet,or full diet without symptoms of stricture[21].The above-mentioned post-hoc analysis suggested that CROSS 0 before stenting was one of the factors related to the difficulty of SEMS placement[13].In contrast,another post-hoc analysis of multicenter clinical trials showed that SEMS as BTS in CROSS 0 patients showed comparable technical and clinical success rates,safety,and short-term outcomes to those in CROSS 1 and 2 patients[22].Thus,it is inconclusive whether CROSS 0 before SEMS placement affects the technical and clinical success rates of SEMS.
COMPLICATIONS
Perforation
Perforation is one of the most common and critical complications of SEMS placement.A recent metaanalysis demonstrated that the overall perforation rate of colonic stenting for OLCC is 5%[17].In addition,several studies have reported the outcomes of patients with stent-related perforations or factors related to stent-related perforations.
According to the meta-analysis mentioned above,when the studies were compared between perforation rates > 8% and ≤ 8%,the perforation rate > 8% group showed poorer technical success rates,although the 5-year overall and disease-free survival rates were not significantly different[17].In a Dutch randomized clinical trial,the SEMS in the BTS group tended to have a lower 4-year disease-free survival rate than that in the ES group.In addition,the subgroup with stent-related perforation had a significantly poorer disease-free survival than the ES group,which suggested that stent-related perforation exacerbated oncological outcomes.However,it should be noted that in this trial,the number of patients was small,and the stent-related perforation rate was high(approximately 23%)[23].Furthermore,it should also be noted that ES had better postoperative outcomes than BTS by stent because of the lower success rate of stent placement reported prior to 2014.
Datyeet al[24]aggregated articles on perforation after SEMS placement for OCC until 2008 and analyzed data such as causes and mortality.The overall perforation rate was 4.9%,and concomitant chemotherapy,steroids,and radiotherapy were identified as risk factors for perforation;however,no significant difference was observed in the perforation rate between palliative treatment and BTS.The authors also emphasized a high mortality rate of perforation cases(16%);however,the data did not necessarily show a negative impact of SEMS itself,considering the low overall perforation-related mortality rate(0.8%)and high mortality rate of ES(15%-20%).
van Halsemaet al[25]pointed to the stent type as a risk factor for perforation.The authors defined stent types with high(< 10%)(WallFlex,Comvi,and Niti-S D-type)and low(< 5%)(Hanarostent and Niti-S covered)perforation rates.In fact,the perforation rates of certain stent types,especially the WallFlex stent,vary across reports.For example,Meisneret al[26]demonstrated that the overall perforation rate of WallFlex stent placement for OCC was 5.1% in 255 cases in prospective and multicenter studies.In a prospective multicenter study using WallFlex stent in Japan,the perforation rate was reported to be 1.6%[27].van Halsemaet al[25]reported a relatively high occurrence of delayed perforation after WallFlex stent placement and considered that the short follow-up period may have reduced the overall perforation rate of the stent.
Migration and re-obstruction
According to a systematic review,the rate of stent migration is approximately 10%(interquartile range 3%-22%).In this report,laser pretreatment and chemotherapy were identified as factors that promote stent migration[28].Because the high risk of perforation and migration has been mentioned,laser or balloon dilation prior to stent placement is not recommended[28-30].The overall re-obstruction rate was reported to be 10%(interquartile range 0%-15%),and when the cases were limited to palliative treatment,the re-obstruction rate was 16%(interquartile range 0%-23%)[28].
Safety of chemotherapy
The negative impact of SEMS on colorectal cancer management has been demonstrated in several respects,including chemotherapy after SEMS placement,which raised the concern that chemotherapy after SEMS placement may increase the risk of perforation.In theory,chemotherapy destroys proliferating cancer cells in the colonic wall;therefore,it can provoke stent-related perforation[25].Although the safety of chemotherapy after SEMS placement remains to be fully elucidated[31],several recent studies have suggested an answer.
In a retrospective study that reviewed patients who underwent SEMS placement,the perforation rates were 13% in patients receiving no chemotherapy,6% in patients receiving chemotherapy without bevacizumab,and 20% in patients receiving chemotherapy with bevacizumab[32].Another retrospective study also suggested that subsequent bevacizumab therapy increased the risk of complications after SEMS insertion,and the perforation risk increased nearly threefold[33].A meta-analysis of studies between 2005 and 2011 further revealed that the perforation rate in patients receiving bevacizumab-based chemotherapy was significantly higher than that in patients receiving no chemotherapy,whereas the perforation rate in patients receiving non-bevacizumab-based chemotherapy was significantly lower than that in patients who received no chemotherapy[25].
Some reports have demonstrated that chemotherapy does not affect the SEMS complications.However,a recent retrospective analysis indicated that chemotherapy before SEMS increased the risk of stent-related complications,whereas chemotherapy after SEMS had no impact on complications[34].In a single-center retrospective study,Leeet al[35]compared the adverse events of SEMS as a palliative treatment for OCC between patients receiving bevacizumab therapy and those not receiving bevacizumab therapy.In this study,the perforation rate in the bevacizumab group was only 1%,which was equivalent to that of the non-bevacizumab group(3%).The authors considered that the low perforation rate might be related to the many years of experience of endoscopists.Additionally,one retrospective study showed the effectiveness and safety of SEMS before neoadjuvant chemotherapy and curative surgery,although the sample size was small.This study suggested the relatively low toxicity and high tolerability of neoadjuvant chemotherapy with two cycles of CAPOX or three cycles of mFOLFOX6 after SEMS.The resected specimens were also analyzed,suggesting a low risk of perineural invasion[36].
POSITIONING IN GUIDELINES
The degree of recommendation for SEMS as palliative management or BTS for OLCC has been described in many international guidelines,and the description seems to change with time.Herein,recent changes in the positioning of SEMS in the guidelines and the impact of changes in the description of SEMS are discussed below.
Websteret al[37]reviewed 19 international guidelines for the management of OLCC between 2010 and 2018.Stenting for palliative management was recommended in most guidelines,whereas opinions regarding the recommendation of emergency stenting as a BTS were divided.Eight guidelines recommended ES,two from the United States recommended emergency stenting as BTS,and nine suggested either ES or stenting as BTS could be selected.Guidelines from countries other than the United States did not actively recommend SEMS as a BTS until recently.
However,the description of the recommendations in the ESGE guidelines has recently changed.In the ESGE guidelines published in 2014,SEMS as BTS for OLCC was not recommended because of the risk of stent-related complications,particularly perforation[38].In recent years,many studies have revealed the long-term safety of SEMS as a BTS;therefore,the description of the ESGE guidelines regarding the use of SEMS for OCC was updated in 2020,and SEMS as a BTS for OLCC has become a recommended treatment[16].
The impact of these updated recommendations in the guidelines has also been reported.The national colorectal cancer guidelines were updated in the Netherlands in 2014,and SEMS as a BTS for OLCC is clearly recommended.Consequently,the application rates of ES and SEMS for OLCC were reversed,and some changes occurred after 2014 in the Netherlands:the proportion of laparoscopic surgery increased,and the permanent stoma rate and total hospital stay decreased[39].
Despite the major impact of the guidelines on treatment,it should be noted that concerns regarding the quality of the guidelines have also been reported.Gavriilidiset al[40]used the Appraisal of Guidelines for Research and Evaluation II instrument to evaluate the quality of the 14 current guidelines describing the management of OLCC.The authors pointed out a poor applicability score in many guidelines and concerns regarding variations in guideline quality.Further research may trigger more changes to the description of guidelines and improve their quality.
SHORT-TERM AND LONG-TERM OUTCOMES
Short-term outcomes
Traditionally,in many cases of OCC,emergency decompression surgery was performed without adequate evaluation of preoperative staging and comorbidity.As a result,the risk of morbidity and mortality was unavoidably involved.SEMS as a BTS is considered a valid option for these cases as it can offer plenty of time to evaluate preoperative problems and improve the medical condition of patients[9].Based on this perspective,it is not surprising that SEMS as a BTS has been reported to be advantageous in terms of short-term outcomes compared to ES.In a meta-analysis of randomized controlled trials comparing SEMS as BTS and ES for OLCC,the need for stoma creation,the incidence of postoperative complications,and the occurrence of wound infection were significantly reduced in the SEMS group[41].
TDT is another option for BTS of OCC;however,TDT has more disadvantages than SEMS:Slow decompression,bad odor,complicated management,difficult oral intake,and poor QOL[42].Furthermore,several meta-analyses have compared the short-term outcomes between SEMS and TDT,and TDT was found to have poorer short-term outcomes.TDT showed lower clinical and technical success rates,solid food intake,and temporal discharge in a subsequent operation;TDT increased blood loss,prolonged operative time,and enhanced stoma rates[18,43].In the context of these circumstances,the ESGE guidelines updated in 2020 do not recommend TDT placement over SEMS placement[16].
Negative reports on long-term outcomes
The advantages of SEMS as a BTS in short-term outcomes have been convincingly demonstrated,whereas the long-term outcomes of SEMS as a BTS have been controversial.In other words,the oncological safety of SEMS as a BTS remains unclear.However,high-quality research on the long-term outcomes of SEMS as a BTS has been increasing in recent years.Thus far,several studies have suggested the negative oncological impact of SEMS placement(Table 1).In a meta-analysis of randomized control trials,although no significant differences were observed in 3-year disease-free survival or overall survival between the SEMS as BTS group and ES group,the risk of systemic recurrence was significantly higher in the SEMS group than in the ES group[44].Katsukiet al[45]analyzed a nationwide inpatient database in Japan and conducted a retrospective cohort study using propensity score-matching.The authors compared the long-term outcomes of patients with OLCC between SEMS as BTS and ES and demonstrated that the SEMS group showed significantly worse overall survival than the ES group.Gorissenet al[46]analyzed OLCC patients aged 75 years and younger from a prospective cohort study.In this study,the local recurrence rate in the SEMS group was significantly higher than that in the ES group,and the authors concluded that SEMS was associated with an increase in local recurrence,particularly in younger patients.Ueharaet al[47]retrospectively evaluated the oncological outcomes of SEMS in patients with stage II or III OCC.The authors reported a higher distant metastatic recurrence rate in the SEMS group than in the ES group.Megeet al[48]examined the overall and disease-free survival of patients who underwent SEMS placement or creation of decompression stoma as a BTS for OLCC in a multicenter retrospective study.The authors demonstrated a significantly lower overall survival rate in the SEMS group,which may be related to an increase in worse pathological findings,such as tumor perforation.Sabbaghet al[49]reported significantly lower overall survival and significantly higher cancer-specific mortality in the SEMS group than in the ES group.
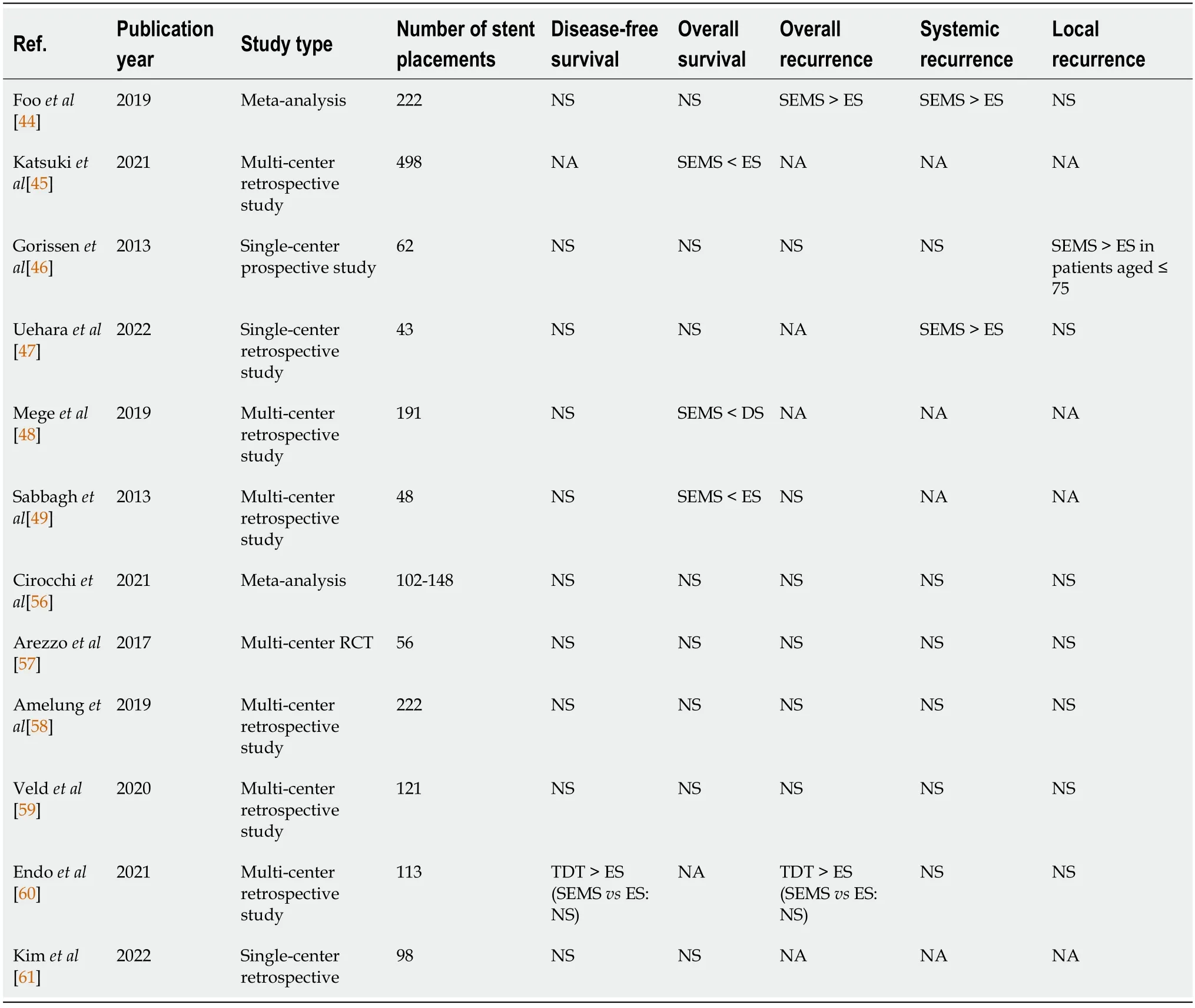
Table 1 Recent reports on long-term outcomes of colonic stenting as a bridge to surgery for obstructive left-sided colon cancer
Negative reports in pathological studies
As mentioned above,the potential negative impact of SEMS on oncological outcomes has also been suggested through histopathological examinations.Sabbaghet al[50]conducted a pathological analysis and revealed that tumor and peritumor ulceration,perineural invasion,and lymph node invasion were seen more frequently in resected specimens after SEMS placement than in cases of surgery only.These pathological features are associated with poor prognosis.Other authors have also reported negative factors for SEMS placement from a pathological viewpoint.Zhanget al[51]analyzed the histopathological findings of specimens resected after SEMS or TDT for OLCC.The authors reported that vascular invasions,wound abscesses,and ulcer formation was more frequently observed in the SEMS group than in the TDT group.
Some reports have also indirectly suggested the negative impact of SEMS on colorectal cancer treatment through analysis of the peripheral blood of patients.Maruthachalamet al[52]reported that circulating cytokeratin 20 mRNA levels after stent placement for left-sided colon cancer was significantly higher than before stenting,suggesting the possibility of tumor manipulation by inserting a guidewire or dilating and deploying the stent.Yamashitaet al[53]showed an increase in viable circulating tumor cells after SEMS placement for OCC,which suggested that SEMS placement and expansion could allow the release of colorectal cancer cells into circulation.Recent technological developments in genome sequencing and molecular diagnosis have allowed the measurement of circulating tumor DNA(ctDNA),which is released from tumor cells undergoing apoptosis or necrosis into the systemic circulation[54].The use of ctDNA has been extensively evaluated as a promising biomarker for the treatment of colorectal cancer.Takahashiet al[55]demonstrated that the plasma levels of ctDNA in patients with OCC increased after SEMS placement,although this increase was not observed after TDT insertion.These findings indicate that SEMS placement may induce tumor cell dissemination.However,it remains unclear whether these changes in peripheral blood are related to the long-term oncological prognosis of patients.
Positive reports on long-term outcomes
As mentioned below,the oncological prognosis of SEMS as BTS is equivalent to that of ES and has been increasing in recent years(Table 1).In a meta-analysis of randomized controlled trials comparing SEMS as BTS and ES for OCC,SEMS showed the same mortality and significantly lower morbidity than ES.In addition,recurrence and survival outcomes were not significantly different between SEMS and ES[56].Arezzoet al[57]demonstrated no significant differences in 3-year overall survival rates or progressionfree survival rates observed between SEMS as a BTS and ES in a large multicenter randomized controlled trial.In addition,considering the significantly lower stoma rate in the SEMS group,the authors concluded that SEMS as a BTS was a viable approach for OCC.Amelunget al[58]retrospectively compared the long-term outcomes of patients with OLCC between SEMS as BTS and ES using propensity score matching,showing no significant differences in the 3-year disease-free survival rates,overall survival rates,or locoregional recurrence rates,whereas the SEMS group showed a lower permanent stoma risk.In a cohort study in the Netherlands,decompressing stoma and SEMS were compared to determine which has advantages as a BTS for OLCC.The study showed no significant differences in the 3-year locoregional recurrence rates,disease-free survival rates,or overall survival rates[59].Endoet al[60]reported that the long-term oncologic outcome of SEMS as BTS for patients with OLCC was comparable to that of ES,whereas the long-term outcome of TDT was poorer than that of ES.A recent Korean retrospective study examining the long-term outcomes of SEMS as BTS for OCC further found no significant difference in the 5-year overall survival and 5-year disease-free survival between the SEMS and ES groups.The authors emphasized the high technical and clinical success rates(99% and 92.9%,respectively)and a low perforation rate(1%)in the study,which could be due to the highly experienced endoscopist.Similarly,SEMS placement performed by experienced endoscopists may improve oncological outcomes[61].Thus,endoscopist experience also seems to influence the longterm prognosis of patients.Amelunget al[62]performed a systematic review and meta-analysis of patients with OLCC to compare the long-term oncological outcomes after SEMS as a BTS with those after ES.The authors demonstrated that SEMS placement showed a significant survival benefit in more than 40 patients.The ESGE also recommends that an experienced endoscopist should perform or directly supervise stent placement[16].
CURATIVE SURGERY AFTER COLONIC STENTING
In cases of resectable OLCC,SEMS can facilitate the performance of minimally invasive one-stage surgery safely and effectively,which is one of the major benefits of SEMS as a BTS.Enomotoet al[63]compared laparoscopic and open surgery after SEMS insertion for OCC.Blood loss in the laparoscopic surgery group was less than that in the open surgery group,whereas the operative time was significantly shorter in the open surgery group.
The safety and efficacy of robot-assisted laparoscopic surgery after SEMS placement have also been reported recently[64].Liet al[65]analyzed 79 cases where SEMS placement was performed for OCC in the largest single center in Singapore from 2013 to 2020.The authors showed that 14% of the patients underwent robot-assisted surgery for curative surgery.The progression and spread of minimally invasive surgery for colorectal cancer can strengthen the benefits of SEMS as BTS.
No consensus has yet been reached regarding the proper waiting period between SEMS insertion and curative surgery.Satoet al[66]retrospectively analyzed the long-term oncological outcomes of patients with OCC who underwent SEMS placement and curative surgery.The authors found that relapse-free survival was significantly shortened when the interval between stenting and curative surgery was longer than 16 d.Another retrospective study examining long-term outcomes after SEMS as a BTS for OCC further demonstrated that the risk of recurrence is associated with a long interval(longer than 18 d)between stenting and curative surgery[67].In a nationwide cohort study in the Netherlands,patients with OLCC receiving SEMS as a BTS were divided into three groups according to the interval between stenting and surgery,as follows:5-10 d group,11-17 d group,and > 17 d.No significant differences were observed in 3-year disease-free survival or overall survival between the groups,although shortterm outcomes were generally better in the 11-17 d group than in the 5-10 d and > 17 d groups[68].In the ESGE guidelines published in 2014,the suggested time interval from colonic stenting as BTS to elective surgery was 5-10 d in patients with left-sided colon cancer;however,recent ESGE guidelines suggested a time interval of approximately 2 wk until resection[16,38].In addition,the authors of the recent ESGE guidelines further described that the time interval should be determined considering the balance between stent-related adverse events and surgical outcomes because a short interval can reduce stent-related adverse events,whereas a long interval can improve surgical outcomes[16].It should also be noted that ctDNA concentration was reported to increase over time following SEMS placement,which implies that a long interval may worsen the oncological outcome[55].At any rate,as there is no prospective comparative study on this matter[16],the optimal time interval between SEMS and curative surgery remains uncertain,and further research is required.
COST-EFFECTIVENESS
Many reports have shown that SEMS is cost-effective for both palliative intervention and BTS.Quinnet al[69]analyzed the costs and effectiveness in patients with unresectable or metastatic colorectal cancer who received SEMS or ES for acute colonic obstruction using decision tree analysis.The authors demonstrated that SEMS is a more cost-effective treatment for palliative intervention than ES.In a Japanese single-center retrospective study,short-term outcomes and total healthcare costs were compared between the SEMS,curative surgery,and ES groups.The study showed earlier oral intake,shorter total hospital stay,and lower total costs in the SEMS group than in the ES group,which suggested that SEMS as BTS was a more cost-effective treatment[70].A Canadian decision analysis performed in 2006 elucidated the cost-effectiveness of SEMS as a BTS compared with the conventional surgical approach for acute OLCC[71].
Despite these studies,many clinicians may still regard SEMS for BTS as a treatment with lower costeffectiveness.Suenet al[72]administered a questionnaire to Oceanian surgeons,surveying their intention to participate in randomized controlled trials on stent placement for OCC.Most surgeons gave a positive response to using stents for palliative treatment,whereas the majority of surgeons gave a negative response to using stents as BTS because they considered stenting as a BTS less cost-effective than ES.
CONCLUSION
Colonic stenting has had a positive impact on the management of OLCC,including facilitating the avoidance of stoma and reducing postoperative complications in the subsequent curative surgery,whereas a negative impact of colonic stenting on long-term oncologic outcomes seemed to have been emphasized until a decade ago.Many recent studies have demonstrated the long-term safety of colonic stenting for OLCC,which led to a change in the ESGE guidelines updated in 2020 as follows:SEMS as a BTS for OLCC is a recommended treatment.It should be noted that the experience of endoscopists is involved in determining the technical and clinical success rates and possibly the oncological outcomes.Uncertainty remains regarding SEMS placement for OLCC,including the long-term oncologic prognosis and safety of chemotherapy after SEMS;further investigation will be needed to clarify these points in the future.
FOOTNOTES
Author contributions:Suzuki H wrote the paper;Tsujinaka S supervised and critically revised the manuscript;Sato Y,Miura T,and Shibata C critically revised the manuscript;all authors have read and approved the final manuscript.
Conflict-of-interest statement:The authors declare no conflicts of interest in regards to this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non
commercial.See:https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Japan
ORCID number:Hideyuki Suzuki 0000-0003-0696-2799;Shingo Tsujinaka 0000-0002-8554-3869;Yoshihiro Sato 0000-0003-3722-6815;Tomoya Miura 0000-0001-9092-460X;Chikashi Shibata 0000-0001-8191-4784.
S-Editor:Chang KL
L-Editor:A
P-Editor:Chang KL