Bedside anterior segment optical coherence tomographyassisted reattachment of severe hemorrhagic Descemet’s membrane detachment after ab externo 360-degree suture trabeculotomy combined with trabeculectomy
Shan-Shan Liu, Li-Mei Liu, Xiao-Jun Fan, Xiao-Xiang Sun, Fu-Mei Yin, Fang-Xing Zhu,Ji-Bing Wang
Glaucoma Unit, Department of Ophthalmology, Weifang Eye Hospital, National Key Clinical Specialty, Weifang 261000,Shandong Province, China
Dear Editor,
We report a case of severe hemorrhagic Descemet’s membrane detachment (HDD) following ab external 360-degree suture trabeculotomy with trabeculectomy that was successfully managed with the guidance of bedside anterior segment optical coherence tomography (ASOCT).Descemet’s membrane detachment (DMD) is a complication that impairs vision and is commonly observed after cataract surgery. It’s reported a high incidence (25%-82%) of focal DMD that were mostly subclinical and detected only with gonioscopy[1]. The incidence of visually significant DMD after extracapsular surgery and phacoemulsification is reported to be 2.6% and 0.5% respectively[2]; however, the most recent reports demonstrate an incidence of 0.044% to 0.52% after phacoemulsification surgery[3-4]. DMD has also been reported to occur in various other surgeries like keratoplasty, iridectomy,vitrectomy, holmium laser sclerostomy, alkali burn. Several cases were reported following glaucoma surgeries, such as trabeculectomy, and Schlemm’s canal operations, such as viscocanaloplasty and trabeculotomy[5]. Several of these DMDs are usually small, localized, peripheral, with nonscrolled edges,and do not require surgical intervention. And management methods include administration of steroids and hyperosmotic agents, neodymium:YAG (Nd:YAG) laser to create a break to dissipate blood, or tissue plasminogen activator to dissolve and wash out the blood. Total DMD requiring surgical intervention for reattachment has been reported after trabeculectomy[6].But severe HDD is exceedingly rare, and its management is more challenging. At present, there are no reports on the management of severe HDD following ab external 360-degree suture trabeculotomy. Herein, we report a case of severe HDD following ab externo 360-degree suture trabeculotomy combined with trabeculectomy and its management with the guidance of bedside ASOCT.
Ethical ApprovalAll procedures adhered to the guidelines of the Declaration of Helsinki. Written informed consent, which was approved by the Office of Research Ethical Committee of the Weifang Eye Hospital (Approval Number: 2021-01-02),was obtained from the patient. This report does not contain any personal information that could lead to the identification of the patient.
A 60-year-old woman presented with a history of advanced bilateral glucocorticoid-induced glaucoma for 3y, which was not controlled with four antiglaucoma medications (carteolol hydrochloride eye drops; brimonidine tartrate;brinzolamide;travoprost). Her best-corrected visual acuity (BCVA, Snellen Chart) was 20/40 in both eyes. The intraocular pressure (IOP,Goldman applanation tonometry) was 26 and 40 mm Hg,the central corneal thickness (Specular Microscope, SP, 3000P,TOPCON, Japan) was 438 and 450 µm, and the number of central endothelial cells was 2153 and 2341 cells/mm2in the right eye and left eye, respectively. Glaucomatous optic disc cupping was significant, with a vertical cup/disc ratio of 0.8 in the right eye and 0.9 in the left eye. Gonioscopy (AVG;Surgical Gonio Lens, Volk Alcon, Mentor, OH, USA) showed a wide anterior chamber angle in both eyes. The Humphrey Field Analyzer (30-2, Humphrey Instruments, Carl Zeiss Meditec. Inc., Germany) revealed that the 30-2 automated perimetry mean deviation was -25.51 in the right eye and-30.34 in the left eye.
The patient underwent ab externo 360-degree suture trabeculotomy with trabeculectomy. The procedure in both eyes was performed competently by Wang JB; the left eye had an improved BCVA at 0.6 with an IOP of 11 mm Hg; however, a shallow anterior chamber was observed in the right eye during suture trabeculotomy. At the end of the procedure, massive DMD and blood in the inferonasal region were observed.The blood was evacuated to the fullest extent through careful aspiration with a cannula, and an air tamponade was performed to reattach Descemet’s membrane.
On postoperative day 1, the right eye had a BCVA of 20/200 and an IOP of 11 mm Hg. Slit-lamp examination revealed a diffused bleb, corneal edema, a small air bubble in the anterior chamber, and hyphema. ASOCT (Visante, Model 1000,Carl Zeiss Meditec, Dublin CA, USA) showed the attached Descemet’s membrane within the area of the air bubble in the superior anterior chamber and the DMD involving the whole pupil area with inferior intrastromal hemorrhage and hyphema.The patient was managed conservatively with intensive steroids and hyperosmotic medication for 3d.
On postoperative day 3, further examination showed that the BCVA of the right eye decreased to counting fingers at 0.5 m,the air bubble disappeared, and corneal edema worsened(Figure 1A). Furthermore, ASOCT showed that DMD involved almost the whole cornea (Figure 1B-1F). Surgical intervention was required, and the ASOCT equipment was moved to the operating room, at the patient’s bedside. A partial-thickness corneal incision was made at the temporal cornea under the guidance of the bedside ASOCT (Figure 1E). The procedures performed by the same surgeon included the following: watertight suture of the scleral flap to prevent air escape; gentle sliding on the cornea with a cannula to evacuate liquefied blood under the condition of the flat anterior chamber, similar to that in the Dirisamer technique applied in Descemet’s membrane endothelial keratoplasty[7]; injection of sterile air into the anterior chamber; and use of beside ASOCT for the re-examination of the right eye to ensure that Descemet’s membrane was reattached completely (Figure 2).On day 1 after the intervention, the BCVA of the right eye was improved to 20/100 with an IOP of 10 mm Hg. The cornea dramatically became clear and the hyphema and air bubble disappeared in the anterior chamber. ASOCT showed the complete reattachment of Descemet’s membrane(Figure 3A). The patient was managed with intensive steroids and non-steroidal drugs for about 2mo. The cornea remained transparent thereafter, and the IOP was maintained without medication during follow-up. Corneal stains were visible in the peripheral inferior area. Three months later, the BCVA was 20/80 and IOP was 11 mm Hg, with clear cornea and residual peripheral corneal stains. The endothelial cell count was 2013 cells/mm2and the central corneal thickness was 416 μm.Lens opacity gradually increased. The BCVA decreased to 20/200 and cataract surgery was performed uneventfully 6mo later. The patient achieved an uncorrected visual acuity of 20/25, and the IOP was 10 mm Hg without medication at 6mo after cataract surgery. The cornea was clear with reduction in blood stains. ASOCT showed that Descemet’s membrane was attached well (Figure 3B). The corneal endothelial cell count was 1880.8 cells/mm2and the central corneal thickness was 429 μm.

Figure 1 The third postoperative day A: Slit-lamp photography shows severe HDD accompanied by massive corneal edema and hyphema,and the air bubble is no longer present; B-F: ASOCT images show the peripheral and central area, non-scrolled DMD with intrastromal hemorrhage, and hyphema; E: OCT confirmed attached region in the peripheral temporal cornea where the incision was made at the arrowheads area. ASOCT: Anterior segment optical coherence tomography; DMD:Descemet membrane detachment; HDD: Hemorrhagic Descemet membrane detachment; OCT: Optical coherence tomography.

Figure 2 The second surgery on the right eye (the surgeon’s view)A: Inferior pre-Descemet hemorrhage, hyphema, and corneal edema before operation; B: Suture watertight of the sclera flap; C: Gentle slide on the cornea with a cannula to evacuate liquified blood out from the cornea incision in temporal cornea under the flat AC; D:Flatted Descemet’s membrane with little blood remained; E: Injected sterile air to the AC; F: Beside ASOCT confirmed that Descemet’s membrane reattached completely. AC: Anterior chamber; ASOCT:Anterior segment optical coherence tomography.
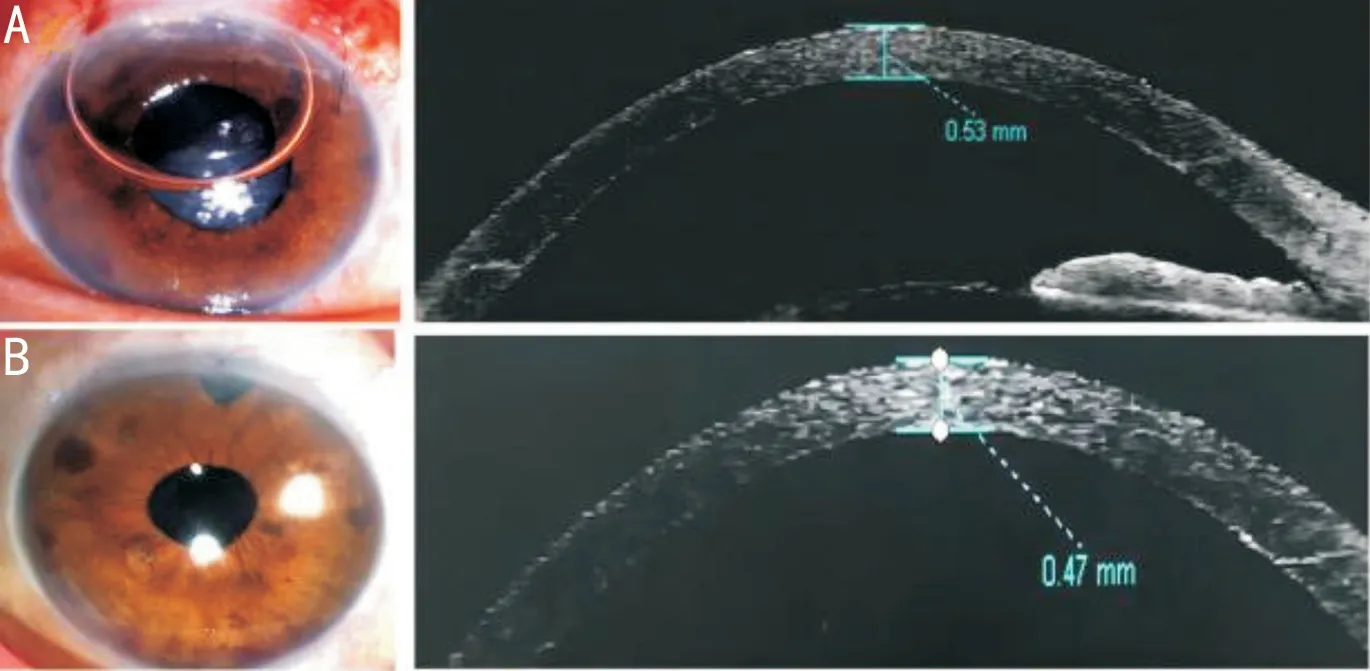
Figure 3 Slit-lamp microscopy and ASOCT examination A: Clear cornea with air bubble in the AC, hyphema disappeared 1d after intervention, ASOCT showed Descemet’s membrane reattached completely; B: The blood staining reduced and the intraocular lens in position 6mo after cataract surgery. ASOCT showed Descemet’s membrane reattached well. AC: Anterior chamber; ASOCT: Anterior segment optical coherence tomography.
DISCUSSION
Schlemm’s canal surgeries are widely used as compared to traditional filtering surgeries in recent years because of their safety, efficacy, quickness, and bleb independence after the procedure[8]. These surgeries include trabeculotomy,viscocanalostomy, and canaloplasty, of which ab interno gonioscopy assisted transluminal trabeculotomy or suture trabeculotomy and ab externo transluminal trabeculotomy or 360-degree suture trabeculotomy are often used in open angle glaucoma. Yalinbaset al[9]compared ab externo and ab interno 360-degree suture trabeculotomy in mild and moderate open angle glaucoma; the results showed similar efficacy in reducing the IOP and similar IOP spike occurring post operation. Complications related to Schlemm’s canal surgery,such as hyphema and small DMD. Jaramilloet al[10]reported a 7.4% incidence of DMD in 162 eyes after canaloplasty, half of which were associated with intracorneal haemorrhage, and do not typically affect visual acuity and intervention is not needed.And localized HDD has also been reported in up to 6.7% of cases, mostly located in the inferior or inferonasal cornea and surgical intervention is usually not needed[11]. Although the best timing and management approach to HDD and intracorneal hematoma remain controversial, most authors agree that the blood should be drained to avoid deterioration of vision. To our knowledge, there have been no reports regarding severe HDD after Schlemm’s canal surgeries.
Most of the DMDs or small HDDs occur during viscoelastic injections or when the microcatheter does not move to the exit continuously; thus, viscoelastics may enter the cornea at Schwalbe’s line because of the weak walls of Schlemm’s canal.In the present case, hemorrhage occurred because episcleral blood refluxed through the collector channels to Schlemm’s canal and then to the space created by the DMD or anterior chamber, similar to that in some reports[9]. The possible reasons for severe DMD may be as follows: long-term high IOP may decrease the adhesion between Descemet’s membrane and stroma[12], a shallow anterior chamber was present, the suture slid to the apex of Schlemm’s canal, and the tract force was more oriented between the stroma and Descemet’s membrane circumferentially during trabeculotomy.
Usually, for severe DMD or HDD cases, surgical management is needed when conservative treatment is unsuccessful.Early drainage is an imperative and mandatory in patients with visual axis involvement. In most cases of HDD, early management resulted in recovery of the BCVA and regaining of central corneal transparency with rapid visual rehabilitation.Management methods include administration of steroids and hyperosmotic agents, Nd:YAG laser to create a break to dissipate blood, or tissue plasminogen activator to dissolve and wash out the blood[13-14]. Most of these evacuative interventions use adjunctive gas descemetopexy, with air or sulfur hexafluoride[15]. Management of HDD with trabeculectomy is more challenging as the tamponading agents would escape through the filter channel[16]. In our case that involved almost the whole cornea, Descemet’s membrane failed to reattach after air tamponade as the bubble escaped from the ostium. So firstly we closed the scleral flap with sutures to form a closed system of the eyeball, which was comparable to the DMD case reported by Sharifipouret al[17].
ASOCT play an important role in the course of DMD therapy.The image quality of ASOCT is superior and also the absence of corneal contact reduces the risk of infection. Some reports showed good results after measured the DMD of cataract surgery by ASOCT and guided conservative or surgical intervention. The scale of HDD involved with whole corneal edema was evaluated using ASOCT. Additionally, with the aid of beside ASOCT, the evacuation incision was made precisely,and DMD was completely reattached. With the development of technology, intra-operative OCT is increasingly applied in various surgeries in the field of glaucoma and endothelial keratoplasty to determine graft apposition and bubble presence at the end of surgery, especially in cases of high-intensity corneal opacity. However, the high cost of microscopeintegrated intra-operative OCT systems and restriction of the scanning area and imaging quality limit its use[18-19]. Moving the ASOCT equipment to the patient’s bedside in the operating room may be a more accessible and practical substitute.
Severe HDD is a rare but potential complication of ab externo 360-degree suture trabeculotomy, leading to vision impairment.Bedside ASOCT and a flat anterior chamber are helpful for placing corneal incision and confirming reattachment of Descemet membrane. A watertight flap closure is important for HDD air tamponade in the eyes with ostium.
ACKNOWLEDGEMENTS
The authors would like to thank the patient and her family for agreeing to collect and report the clinical data.
Authors’ contributions:Wang JB, Liu SS, Liu LM, and Fan XJ performed the operations. Sun XX, Yin FM, and Zhu FX were responsible for data acquisition. Liu SS drafted the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest: Liu SS,None;Liu LM,None;Fan XJ,None;Sun XX,None;Yin FM,None;Zhu FX,None;Wang JB,None.
 International Journal of Ophthalmology2023年2期
International Journal of Ophthalmology2023年2期
- International Journal of Ophthalmology的其它文章
- Perspectives and clinical practices of optometrists in Saudi Arabia concerning myopia in children
- Progression of myopia among undergraduate students in central China
- Flipped classroom approach to global outreach: crosscultural teaching of horizontal strabismus to Chinese ophthalmology residents
- Topical ketotifen treatment for allergic conjunctivitis: a systematic review and Meta-analysis
- Pseudomembranous conjunctivitis in a patient with DRESS syndrome
- Two cases of persistent shallow anterior chamber after cataract surgery combined with goniosynechialysis
