Perspectives and clinical practices of optometrists in Saudi Arabia concerning myopia in children
Muteb K. Alanazi, Essam S. Almutleb, Yousef S. Badawood, Mohammed A. Kudam, Maria Liu
1Optometry Department, College of Applied Medical Sciences,King Saud University, Riyadh 11362, Saudi Arabia
2UC Berkeley School of Optometry, Berkeley 94720,California, United States
Abstract
● KEYWORDS: myopia; myopia management; optometry;clinical practice; Saudi Arabia
INTRODUCTION
Myopia prevalence has dramatically increased worldwide, reaching epidemic levels. In the United States, one-third of individuals aged 12 years and older are reported as myopic[1]. European countries such as Hungary revealed that myopic refractive error was three times higher in young adult individuals compared to older age groups(>55y)[2]. Some Asian countries have documented an even higher prevalence of myopia. In China, the prevalence is more than 80% among schoolchildren older than 12y[3], where the myopia prevalence in Chinese university students exceeded 90%[4]. It is estimated that by 2050, approximately half of the world’s population will be myopic[5]. Despite the significant increase in myopia prevalence worldwide, the prevalence varies across populations of different regions and ethnicities.In Saudi Arabia, studies reported a myopia prevalence of 49%among adults in the Riyadh region[6], and a similar prevalence was reported in adults in the eastern region of the country[7].Few cross-sectional studies examined the prevalence of myopia among children in Saudi Arabia and found that the prevalence of uncorrected myopia varied between 4% and 6%[8-9].
The issue of myopia is not only the reduced visual acuity but also the potential for substantial vision loss. It has been reported that patients with moderate (spherical equivalent ≤-3.0 to >-6.0 D) to high myopia (spherical equivalent ≤-6.0 D) are significantly more susceptible to ocular abnormalities and at a higher risk of developing vision-threatening ocular diseases, such as cataracts, retinal detachment, chorioretinal atrophy, and glaucoma[10-11].Additionally, the earlier the onset of myopia, the greater the risk of its progression and severity. This increases the risk of serious ocular diseases associated with myopia and the lifetime economic burden[12-13]. Therefore, early management of myopia progression with effective strategies should be a priority.
Slowing myopia progression can be accomplished by either of two mechanisms of action, optical or pharmaceutical, both of which have clinically relevant therapeutic effects. There are three main evidence-based myopia control strategies:two based on optical defocus (overnight orthokeratology and multifocal soft contact lenses) and one pharmaceutical agent(topical atropine)[14-19]. Based on available evidence from clinical trials, atropine appears to be the most promising single therapy for myopia retardation, with up to a 70% myopia control rate depending on the atropine dose. However, significant side effects are associated with higher concentrations[14-15]. In contrast, optical modalities showed significant anti-myopia efficacy in children, varying between 43% and 46% for orthokeratology and multifocal contact lenses[16].
Therefore, understanding the current clinical habits of myopia management is essential. Practitioners in countries such as the US and China are early adopters of myopia control treatment modalities in optometric practices to address the dramatic increase in myopia prevalence and severity; however, there are significant intra-regional differences. The vast majority of practitioners still prescribe single-vision spectacles as the primary management of pediatric myopia[20-21].
In Saudi Arabia, most healthcare services are provided free of charge to all citizens. Ministry of Health is the government and primary service provider through its public hospitals and health centers across the country, making up 60% of the health care services[22]. In 2002, Health Insurance Council was formed in Saudi Arabia that introduced the first guideline for mandatory health insurance that was implemented gradually.Free-of-charge healthcare services are a unique advantage of the Saudi Arabian healthcare system. However, significant population growth and increased life expectancy have led to long waiting times for many healthcare services that can easily exceed several weeks to months, including vision care services. A referral from a primary care physician to an eye clinic is required for a child with myopia to obtain vision care services. This process will most likely take weeks for a myopic child to receive necessary vision care services. Parents may seek private eye clinics and pay for vision care services to avoid long waits and processes. Since the healthcare system in Saudi Arabia is quite different from that in western countries such as the United States, it may impact the early detection of childhood myopia as well as the adoption and implementation of myopia control management approaches in the region,which may differ from what has been observed in other countries with different healthcare systems.
To the best of our knowledge, several gaps remain with respect to understanding the current clinical practice in Saudi Arabia.There are no published data discussing the current clinical approach of practitioners in Saudi Arabia and their knowledge of the condition. There is a critical need to obtain information that sheds light on the clinical examination and treatment of children with myopia.
The aim of the present study was to assess optometrists’knowledge and understanding of myopia in Saudi Arabia, their self-reported practices in the diagnosis of childhood myopia,and their level of engagement in myopia management. In addition, we investigated the potential limitations that restrict the adoption of myopia treatment modalities in the region.
SUBJECTS AND METHODS
Ethical ApprovalThis study followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of King Saud University College of Medicine(approval number: E-21-6366). Informed consent was obtained from all participants.
ParticipantsAs of 2021, there are a total of 1886 practicing optometrists in Saudi Arabia (64% male), with 45% practicing in the capital of the country (i.e., Riyadh), according to the Saudi Commission for Health Specialties. An online questionnaire was created in English with an available Arabic translated version using Google Forms. The questionnaire was directly distributed to optometristsviaemail and social media platforms, beginning in November 2021. The questionnaire was available and received responses over 12wk. Reminders were sent every three weeks.
Survey DesignThe questionnaire was designed to measure:1)optometrists’ knowledge and awareness of myopia, including its associated risk of ocular diseases, 2) self-reported clinical practice performed by optometrists for myopia diagnosis and management for children, 3) myopia control treatment, and 4)self-reported barriers by optometrists that limit the adoption of myopia control treatments. Multiple answers were permitted for some questions about the myopia-associated risk of ocular diseases and the routinely performed clinical procedures.
Statistical AnalysisStatistical analyses were conducted using SPSS (v28 IBM, New York, USA). Descriptive analyses were performed to determine the percentage of respondents for each question. Graphs were plotted using SPSS v28 and Microsoft Excel 2019. A Chi-square analysis was performed to examine the differences between the sample of respondents and the population of optometrists in Saudi Arabia.
RESULTS
Practitioner DemographicsOf the 1886 practitioners, 171 complete responses were collected from 171 optometrists(9.06% response rate) over a period of 12wk, beginning in November 2021. Over 50% of the practitioners were practicing in the Riyadh region as the primary practice location.Approximately 60% of respondents were male optometrists.Almost two-thirds (65%) of the respondents reported having a clinical and research interest in myopia management. Seventy percent of the respondents reported working in public health clinics or hospitals, while the rest worked in independent clinics or academic institutes. Over half of the respondents reported that they routinely provided clinical care to 6 to 15 children with myopia every week. The proportion of respondents who completed the survey did not significantly differ from the population of practicing optometrists in Saudi Arabia based on sex (χ2=0.44,P=0.5) and region (χ2=2.05,P=0.36). The percentage of respondents in this study was greater than that reported in previous studies that targeted optometrists and other healthcare practitioners in Saudi Arabia[23-24].
Clinical Examination and Diagnosis of Myopia in ChildrenFigure 1 provides an overview of responses regarding the clinical tests that are routinely used to examine schoolchildren with myopia, defined between the ages of 6 and 16y, on initial presentation.
Three lists of clinical examinations (i.e., refraction, binocular vision, and ocular biometrics) were included in the questionnaire. All respondents indicated that they would perform refraction, with 59% reporting cycloplegic retinoscopy and 53% indicating non-cycloplegic (manifest)subjective refraction. Cycloplegic measures of refraction have been reported to manifest slightly more frequently. Over 80%of respondents indicated that they would perform the cover test, whereas about 12% reported that they did not perform binocular vision assessments in children with myopia. Most respondents (62%) reported that they performed at least one of the listed ocular biometric tests (i.e., axial length, corneal topography, pupil size measurement, and peripheral refraction),whereas approximately 38% reported that they did not perform any of the biometric tests. Axial length measurements and corneal topography were most frequently reported in children with myopia (37% and 36%, respectively; Figure 1).
Practitioners’ Awareness of Ocular Complications of High MyopiaPractitioners were asked about their knowledge of the association between high myopia (≤-6.0 D) and ocular pathology with a total of seven ocular conditions being listed in this survey. Interestingly, three ocular conditions (i.e., diabetic retinopathy, age-related macular degeneration, and angleclosure glaucoma) were also listed with the perception of being associated with high myopia, which has not been demonstrated in clinical studies. Association of retinal detachment/breaks with high myopia were reported by 75% of participants whilst approximately one-third of respondents selected cataract to be associated with myopia. The other listed ocular conditions (i.e.,choroidal neovascularization, primary open angle glaucoma,angle-closure glaucoma, diabetic retinopathy, and age-related macular degeneration) were reported in the range of 13% to 20%.
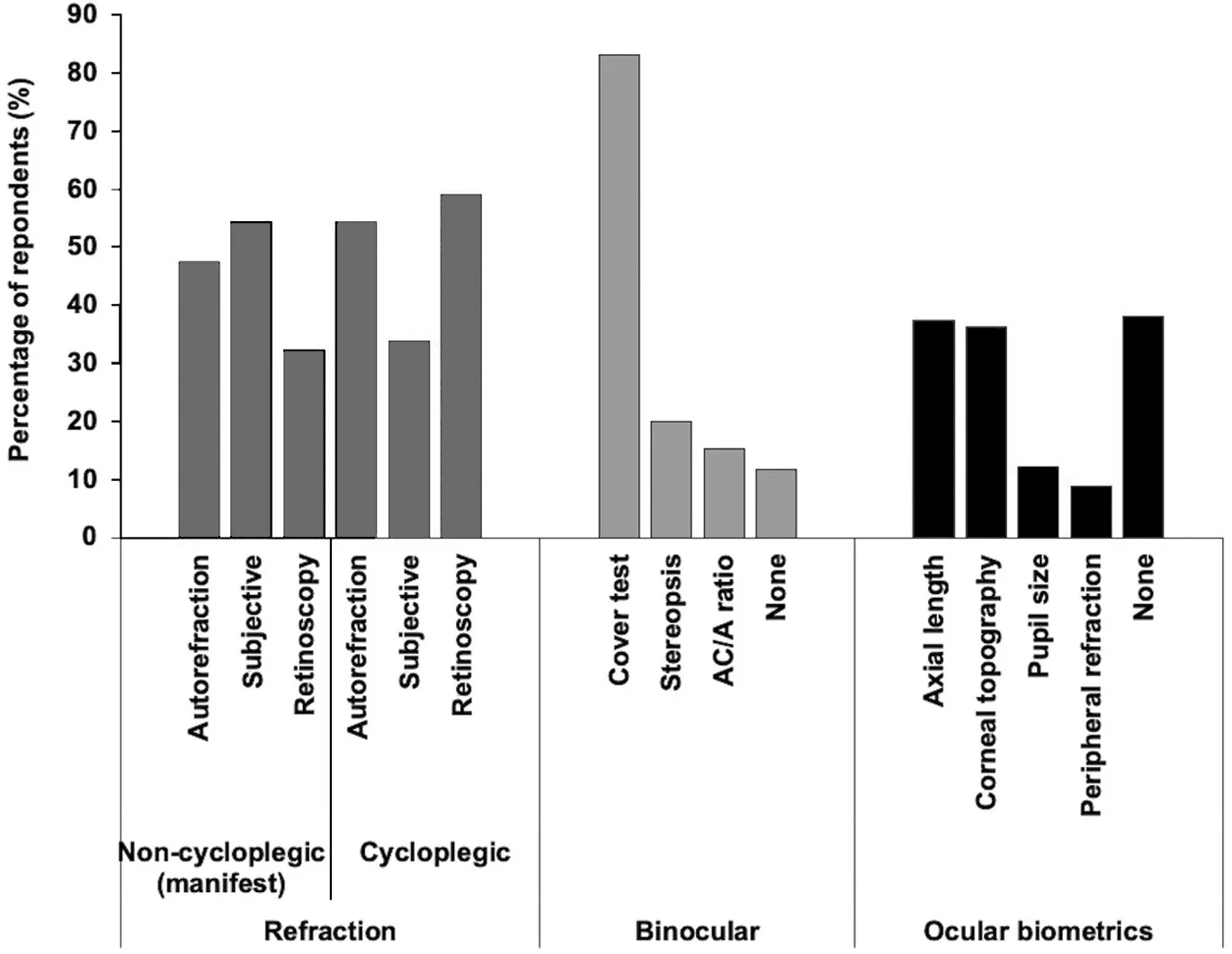
Figure 1 Percentage of reported routinely performed clinical procedures on all school-aged children (5-16y) with myopia on initial presentation.
Management Approaches to Childhood Myopia in Saudi ArabiaSixty-five percent of the respondents reported that they did not use any type of myopia treatment modality and prescribed only single-vision distance full correction lenses for children with myopia. Thirty-five percent of respondents reported that they would prescribe myopia control treatment.In the survey, three questions were asked about practitioners’type of myopia management choice as the first, second, and third most commonly prescribed treatment modalities. The questions consisted of a list of myopia control treatment strategies, including atropine, orthokeratology, multifocal contact lenses, multifocal spectacles, and advising patients to increase the time spent outdoors. Interestingly, 80% of the respondents who prescribed myopia control treatments reported that advising patients to increase the time spent outdoors was their first choice. However, high-dose atropine(1%) was not administered by any of the practitioners (Table 1).Furthermore, practitioners were asked about the frequency of myopia treatment prescriptions. Sixty percent of the optometrists who reported that they would prescribe myopia treatment indicated that they only prescribed it to approximately 30% or less of their patients with childhood myopia (Figure 2). Practitioners who reported that they would prescribe myopia control treatments were asked to rate the relative importance of several potential factors that are considered important when deciding on a myopia control strategy for a child. The child’s rate of myopia progression and the child’s current refraction were rated to be “very important”and “important” by over 75% of the respondents. Factors suchas the child’s pupil size and ethnicity were the least important factors reported when deciding upon myopia treatment(Figure 3).

Table 1 Percentage of optometrists’ selections of childhood myopia management approaches

Figure 2 Percentage of respondents reporting the frequency of prescribing myopia control treatment strategies to their school children with myopia.
Role of Optometrists in Parent EducationRespondents were asked when and how frequently they discussed the long-term ocular risk associated with myopia and options for management. Approximately 30% of the practitioners reported that they would discuss these topics with parents or adult caregivers of myopic children. Over the third of respondents only discussed the condition and the treatments with an adult caregiver if the child had high myopia (≤-6 D; Figure 4).
Potential Barriers in Providing Childhood Myopia TreatmentSeveral potential factors are listed in the survey.Practitioners were asked to rate the relative importance of each factor as a barrier limiting the adoption of myopia control treatment in their practice. The factors that were considered most important were insufficient support from the workplace and the lack of experience needed to provide clinical care to children with myopia (Figure 5).
DISCUSSION
The major aim of this study was to investigate the knowledge and understanding of optometrists in Saudi Arabia in relation to childhood myopia, current clinical practice in diagnosing childhood myopia, and level of practitioners’ engagement in myopia management. The survey also assessed the potential limitations that restrict the adoption of myopia treatment in the country. To the best of our knowledge, this is the first study to report on the current practice of childhood myopia management in Saudi Arabia.
Responses were received from all regions of Saudi Arabia.The majority were male optometrists in the Riyadh region.According to recent data obtained from the Saudi Commission for Health Specialties, there are 1886 practicing optometrists in Saudi Arabia, of which 64% are male, and 45% are in Riyadh. Based on the results, the distribution of respondents by region and gender was similar to that obtained from the Saudi Commission for Health Specialties in 2021. The obtained response rate of the current study was 9.06%, which is higher than the rates reported in previous studies that targeted optometrists and other healthcare professionals in Saudi Arabia at 2.6% and 1.6%, respectively[23-24].

Figure 3 Percentage of optometrists rating the relative importance of factors when deciding on a myopia management approach for children.

Figure 4 Percentage of respondents who indicated discussing the risk of ocular diseases associated with myopia and myopia treatment options with adult caregivers.
With respect to the clinical tests used to examine schoolaged children with myopia, there was a slightly higher preference for cycloplegic refraction measures (59% and 54%,respectively). Cycloplegic refraction is considered the “gold standard” for measuring refractive error in children. Failure to use cycloplegic measures likely overestimates the degree of myopia in children[25]. Given there is a strong association between higher myopia and longer ocular axial length[26],ocular biometric measures such as axial length have become essential in monitoring the ocular changes with myopia interventions. Other biometric measures are essential when implementing certain myopia control treatments (i.e., corneal topography for orthokeratology, multifocal contact lens fitting,and pupil size to monitor the induced dilation from atropine treatment). Considering that this study reports current clinical practice rather than research, 37% of practitioners reported taking axial length at the initial examination of a myopic child with myopia, whereas 38% indicated that they would not take any ocular biometric measures. This finding likely reflects the limited accessibility of expensive optical-based biometry medical instruments within optometric practices.
Myopia is a risk factor for several serious ocular diseases that lead to irreversible vision impairment. The risk is significantly higher in highly myopic eyes (≤-6 D). Most respondents were aware of the associated incident risk of retinal breaks/detachments with myopia. However, most respondents were unaware of the risks of cataract, choroidal neovascularization,and primary open angle glaucoma. On the other hand, a proportion of respondents (13% to 16%) reported that there was an association between increased incidence of angleclosure glaucoma, diabetic retinopathy, and age-related macular degeneration with high myopia, which have not been linked with myopia[27]. Although it is well known that several complications are related to high myopia. In this study,there were misconceptions from respondents that some other ocular conditions such as diabetic retinopathy and age-related macular degeneration are also associated with high myopia.Therefore, further education is necessary to provide accurate and recent knowledge about myopia-related complications and to elucidate the mechanisms by which high myopia leads to increased risks of these ocular conditions.

Figure 5 Percentage of optometrists rating the relative importance of barriers that limit the adoption of myopia management approaches in clinical practices.
The results of several clinical trials have established that overnight orthokeratology is one of the most effective myopia treatments[28]. The survey asked about the types of myopia management options prescribed by practitioners and how frequently they were prescribed to children with myopia.Approximately two-thirds (65%) reported that they would prescribe only a single vision correction for children with myopia. A similar percentage was found in a study that investigated myopia control global trends in Asia, Australia,Europe, North America, and South America in year 2015[20].The same study was repeated after between the years 2018 and 2019 and reveal that the primary approach was still prescribing single vision correction for myopic children(64%)[29]. Another study that surveyed Australian optometrists found that about half of practitioners prescribed single vision distance correction to manage myopia in children[21]. Only 35%of the respondents indicated that they would prescribe myopia management approaches to their patients. Notably, advising optometrists to increase the time spent outdoors was the most reported myopia management approach (80%) as a first choice. The beneficial protective effect of increasing time spent outdoors against myopia development and progression has been reported while ensuring adequate outdoor time[30-31]. On other hand, other studies have shown no clear benefit against myopia[32]. Interestingly, myopia management approaches such as overnight orthokeratology and high-dose atropine were the least reported by practitioners, which could be linked primarily to lack of experience and knowledge, lack of clinical equipment, and insufficient clinical guidance. Since advising adult caregivers to increase time spent outdoors for their children does not require clinical experience or possession of clinical devices, it is plausible that this management approach was reported to be the most used among practitioners. One of the factors reported as the most important barrier to myopia management adoption was the lack of experience needed to provide clinical care to children with myopia, which supports the high percentage with this particular approach.
This study sheds light on the clinical behaviour of optometrists in relation to childhood myopia in Saudi Arabia. The findings demonstrated that most clinical diagnostic tools were performed on myopic children on the first presentation. Distance singlevision spectacle lenses are considered the main approach by most practitioners. Among the prescribed myopia management approaches, increasing the time spent outdoors is the most commonly used approach.
Moving forward, some public health efforts should focus on promoting the importance of early establishment of ocular growth profiles and possible government subsidies for optical biometers to allow the earliest possible detection of abnormal axial elongation preceding the refractive onset of myopia.Moreover, note that currently, none of the novel spectacles designed for myopia control are available in Saudi Arabia;however, once available, they will likely play an important role in the public health effort for myopia management, considering their safety, convenience, and feasibility in the primary care setting.
ACKNOWLEDGEMENTS
The authors extend their appreciation to the Deanship of Scientific Research, College of Applied Medical Sciences Research Center at King Saud University, for funding this work.
Conflicts of Interest:Alanazi MK,None;Almutleb ES,None;Badawood YS,None;Kudam MA,None;Liu M,None.
 International Journal of Ophthalmology2023年2期
International Journal of Ophthalmology2023年2期
- International Journal of Ophthalmology的其它文章
- Progression of myopia among undergraduate students in central China
- Flipped classroom approach to global outreach: crosscultural teaching of horizontal strabismus to Chinese ophthalmology residents
- Topical ketotifen treatment for allergic conjunctivitis: a systematic review and Meta-analysis
- Pseudomembranous conjunctivitis in a patient with DRESS syndrome
- Two cases of persistent shallow anterior chamber after cataract surgery combined with goniosynechialysis
- Bedside anterior segment optical coherence tomographyassisted reattachment of severe hemorrhagic Descemet’s membrane detachment after ab externo 360-degree suture trabeculotomy combined with trabeculectomy
