Effects of slanted bilateral lateral recession vs conventional bilateral lateral recession on convergence insufficiency intermittent exotropia: a prospective study
Yuan-Jin Li, Xiao-Qi Huang, Bei-Qian Yi, Yi-Jia Zhao, Die-Wen-Jie Hu, Run-Ting Ma,Wen-Ping Li, Mei-Hong Ye, Lian-Hong Zhou
Department of Ophthalmology, Renmin Hospital of Wuhan University, Wuhan 430060, Hubei Province, China
Abstract
● KEYWORDS: ocular surgery; exotropia; convergence insufficiency; prognosis; pediatric disease
INTRODUCTION
Intermittent exotropia (IXT) is a transitional strabismus that exists between exotropia and constant exotropia[1]. It is the most common type of strabismus in children of Asian descent[2]. Patients with IXT may have their eyes normally positioned when fixing their attention, with exotropia occurring when they are tired or distracted. Convergence insufficiency intermittent exotropia (CI-IXT) is a subtype of IXT, characterized by at least 10 prism diopters (PD) greater exodeviation for near vision than distant vision.
Eye position control in CI-IXT patients is worse than in patients with other types of IXT, and surgical treatment should be done as soon as possible[3-5]. Conventional bilateral lateral recession (C-BLR) and slanted bilateral lateral recession(S-BLR) are currently the two commonly used operations to treat CI-IXT. Although C-BLR has been widely used, it remains unable to fix excessive near-distance difference (NDD)in CI-IXT patients. Comparatively, S-BLR is a modified operation, with the main purpose of reducing NDD[5-9]. Due to the limited number of previous studies on S-BLR, the different success criteria used, and lack of randomization in prospective studies, there remains insufficient evidence to support S-BLR as the recommended treatment for CI-IXT.
Given this, we sought to adopt a prospective, randomized,controlled, double-blind method for a clinical study regarding S-BLR and C-BLR surgical approaches. We observed the differences in several post-operative clinical measurements,including near deviation, distance deviation, and NDD between 22 patients receiving either S-BLR or C-BLR. Patients were then followed up for 12mo after surgical intervention to objectively evaluate the effects of S-BLR and C-BLR as treatment approaches for children with CI-IXT.
SUBJECTS AND METHODS
Ethical ApprovalThis study followed a protocol approved by the Medical Ethics Committee of Renmin Hospital of Wuhan University (No.201973). CI-IXT patients who were treated at Renmin Hospital of Wuhan University from July 2019 to December 2020 met the following inclusion criteria, and informed consent was obtained from legal guardians.
Research SubjectsTwenty-two patients who underwent strabismus surgery performed by the same surgeon were included in this study. According to the study’s randomization design, 22 patients were randomly divided into the experimental and control groups (11 cases per group) using the random number table method. The experimental group received S-BLR,while the control group received C-BLR.
Inclusion and Exclusion CriteriaInclusion criteria included 1) age 5-12y; 2) according to their response to 1h preoperative monocular occlusion, near deviation was at least 10 PD greater than distant deviation, distant deviation being ≥15 PD, and near deviation being ≤50 PD; 3) ability to control eye position was ≥3; 4) ciliary muscle palsy refraction myopia ≤5.0 D,hyperopia ≤3.0 D, and anisometropia ≤2.5 D; 5) best-corrected visual acuity of eyes with poor eyesight ≥0.5 and binocular vision difference <2 lines; 6) if any eye had myopia <-0.5 D,astigmatism >|1.5 D|, or anisometropia >1.0 D, the patient was required to wear glasses for at least 2wk before re-checking the degree of strabismus; 7) the subjects and their parents or legal guardians provided written informed consent and were willing to accept randomization into a study group followed by regular follow-up.
Exclusion criteria included the following: 1) history of either previous strabismus surgery or botulinum toxin injection; 2)combined with vertical strabismus >5 PD, abnormal oblique muscle function, rotational strabismus, dissociated vertical deviation or A and V patterns, and/or combined with other horizontal, vertical muscle transposition surgery, oblique muscle surgery, and/or vertical muscle surgery; 3) paralytic or restrictive strabismus; 4) when looking to the right or left, strabismus is 5 PD more than the original strabismus;5) presence of any other eye diseases, except for strabismus and/or refractive error; 6) history of intraocular surgery and/or refractive surgery; 7) abnormal craniofacial development affecting the orbit; 8) obvious neurological abnormality; 9)born with pregnancy less than <34wk or birth weight <1500 g.
Research Methods
Organizational division of labor and requirementsThe research team consisted of three people, including one standing research manager, one operator, and one examiner. The research manager was responsible for the design, grouping,work scheduling, data collection, and arrangement of the prospective study. The operator operated on subjects based on sealed randomization numbers; the examiner was responsible for measuring all observational indicators of the subjects.During the study, the subjects and the examiners were blinded,and the operation records were uniformly collected regarding the number of millimeters of the lateral rectus in each eye; the median value of the slanted lateral recession was also recorded.Unblinding was implemented either at study termination or subject withdrawal/discontinuation.
Observational indicatorsEye position examination included the following: 1) near deviation, distant deviation, NDD; 2)binocular vision function (near stereopsis); 3) visual acuity and refractive status. Surgical success criteria included:postoperatively, regardless of the near or distant residual exotropia <10 PD, residual esotropia <5 PD, and NDD <10 PD,the prism and alternative cover test (PACT) were tested at least twice.
Preoperative evaluationSubjects’ basic information and medical history was collected and included: 1) external eye and anterior segment under slit lamp and fundus examination under fundus pre-set lens; 2) binocular vision function (including wearing the appropriate glasses, near stereopsis, repeating the examination three times, and recording the best results.Stereopsis was evaluated by the Titmus test at near); 3) Scores regarding the ability to control (according to the grading method of eye position control ability proposed by Mohney and Holmes[10]) and the examination was repeated three times,with the worst result being recorded; 4) vision and refractive examination, patients who developed myopia <-0.5 D,astigmatism >|1.5 D|, hyperopia >+3.0 D, and/or anisometropia>1.0 D were required correction with glasses, while myopia and astigmatism were required complete correction; hyperopia was properly under-corrected; 5) patients underwent monocular occlusion for 1h prior to eye position examination to rule out a pseudo IC-IXT. Eye position examination was conducted after proper optical correction, with the deviations at distance(6 m) and near (33 cm) of each patient measured by prism and alternate cover tests with fixation on accommodative targets indoors; 6) AC/A ratio (placing -2.00 D spherical lenses in front of each eye, and the far-gradient was used to measure the AC/A ratio[11]; 7) eye movement examination, which included checking eye movement in 9 diagnostic eye positions; 8)torsional strabismus examination was assessed with the foveato-dise angle (FDA) in fundus photography.
If the surgery was delayed for more than one month for any reason, the preoperative evaluation was repeated.
Surgical methodGeneral or local anesthesia was performed according to the age and/or cooperation level of the patient.All surgeries were performed by the same surgeon. Following a conjunctival cul-de-sac incision, the muscle was disinserted,recessed, and sutured directly to the globe. The upper pole of the muscle was recessed according to the distant exodeviation and the lower pole according to near exodeviation. Surgical doses for the lateral recession were calculated primarily based on Park’s method.
Follow-upAll post-operative, follow-up visits were scheduled 1wk, 1, 3, 6, and 12mo after surgery and included:external eye and fundus examination, binocular vision function examination, control ability score, visual acuity and refractive examination, eye position examination, AC/A value measurement, eye movement examination, and rotational strabismus examination. To improve the follow-up rate, all follow-up visits were scheduled in advance. Researchers also reminded subjects and their parents or legal guardians 1wk in advance of the visit.
Statistical AnalysisSPSS 23.0 software was used for all statistical analysis. The data for postoperative near and distant deviations as well as those for NDD and NDD improvement did not conform to a Gaussian distribution and are expressed as median and quartile [M (Q25, Q75)]. Enumeration data were expressed as a percentage. All hypothesis tests were two-sided tests. Statistical significance was determined at aP-value less than 0.05. The Wilcoxon rank-sum test was used to compare the measurement data between groups, and the Fisher’s exact test was used to compare the enumeration data between groups. One-way repeated measurement ANOVA was used to compare the preoperative and postoperative strabismus and NDD between the two groups.
RESULTS
Patients’ CharacteristicsIn this study, there were 5 males and 6 females in the S-BLR group, with 4 males and 7 females in the C-BLR group (P=1.000). The patients’ characteristics data are shown in Tables 1 and 2.
Postoperative CorrectionThe characteristics of the subjects obtained from the last follow-up are shown in Table 3. The success rate of S-BLR group was 90.91% (10/11), and the over-correction rate was 9.09% (1/11); the success rate of C-BLR group was 72.73% (8/11), and the over-correction rate was 9.09% (1/11). Overall, two cases of NDD remained 10 PD, and 1 case of NDD was 14 PD in C-BLR group. For each group, there was one case of over-correction without diplopia that was clinically observed.
Post-operative Improvement of Near and Distant DeviationThe comparisons in the improvement of near and distant deviation between the two groups after surgery were shown in Table 4. One week after surgery, there was no significant difference in near deviation between the two groups (Z=-1.280,P=0.201). There were statistically significant differences in 1, 3, 6, and 12mo after operation. The distant deviation in the two groups was not statistically significant in 1wk, 1, 3, 6, and 12mo after the operation.Table 2 Preoperative clinical data in two groups of CI-IXT patients M (Q25, Q75)
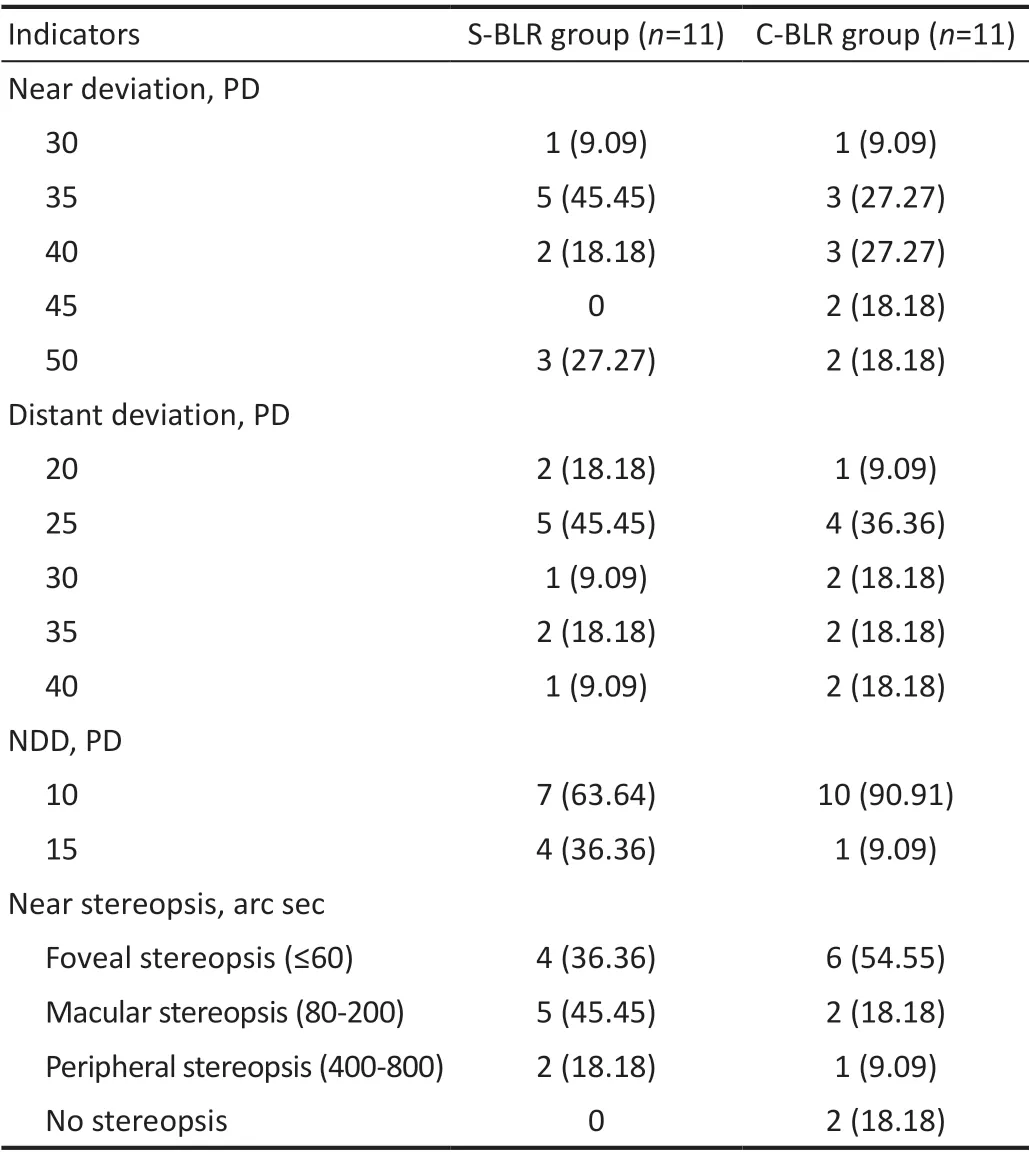
Table 1 Preoperative ocular position and near-stereoscopic examination in two groups of CI-IXT patients n (%)

CI-IXT: Convergence insufficiency intermittent exotropia; M: Median;Q: Interquartile range; S-BLR: Slanted bilateral lateral recession;C-BLR: Conventional bilateral lateral recession; NDD: Near-distance difference; PD: Prism diopters.
Postoperative Near-Distance DifferenceNDD in the C-BLR group had a general, increasing trend (F=92.78,P<0.001),while the NDD in the S-BLR group showed an overall decreasing trend (F=19.101,P=0.001).
Postoperative 1wk, there was no significant difference in NDD between the two groups (Z=-1.846,P=0.065). There were statistically significant differences in NDD between the two groups at 1, 3, 6, and 12mo after surgery (Table 5). NDD improvement of postoperative 1wk, there was no significant difference between the two groups (Z=-1.944,P=0.052),while 1, 3, 6, and 12mo after surgery, the difference in NDD improvement between the two groups was statistically significant (Table 5).

Table 3 Surgical outcomes of two groups at different, post-operative time points n (%)
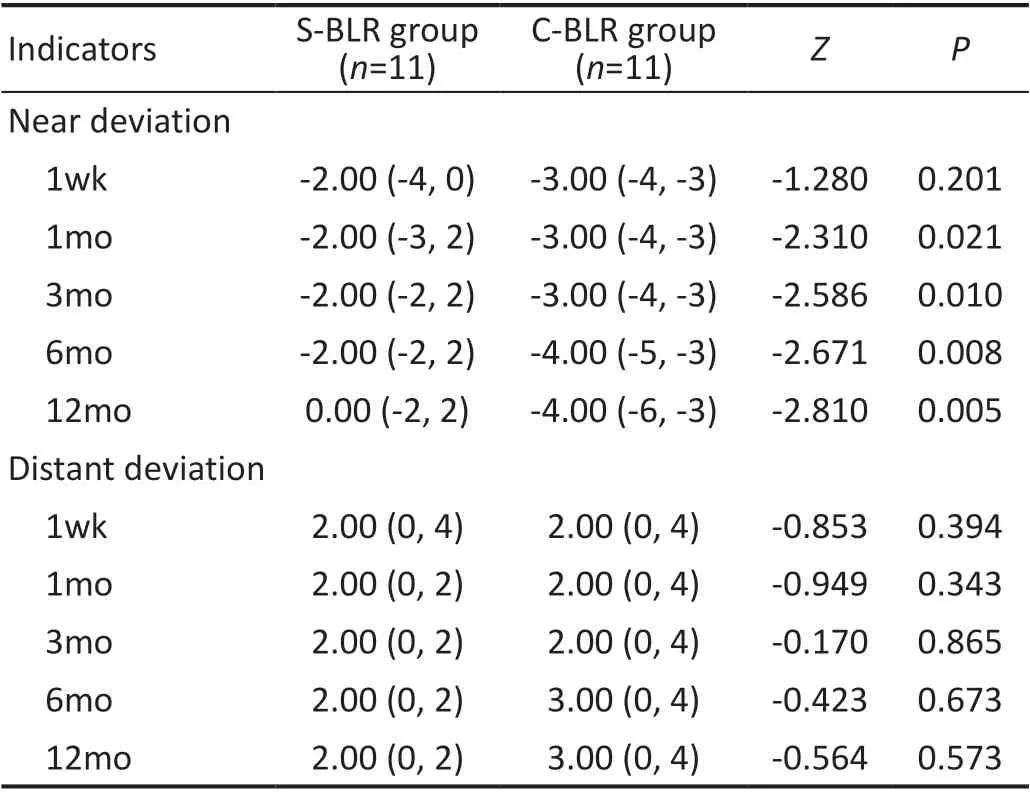
Table 4 Deviations comparison between two groups after surgery M (Q25, Q75), PD

Table 5 NDD comparison between two groups after surgery M (Q25, Q75), PD
Postoperative Near Stereoacuity ImprovementOf the 11 patients in the S-BLR group, 4 had normal stereoacuity before surgery. At 12mo postoperatively, 6 patients in the S-BLR group had improved near-stereoacuity compared with thatbefore surgery. Of the 11 patients in the C-BLR group, 6 had normal stereoacuity before surgery, 5 patients had improved near-stereoacuity 12mo after surgery compared with that before surgery, and 2 patients had no stereoacuity before and after surgery. There was no significant difference in near stereopsis between the two groups 12mo after surgery (Z=-8.77,P=0.380; Table 6).

Table 6 Near stereoacuity in two groups after surgery n (%)
DISCUSSION
The results obtained in this randomized prospective study showed that in patients with CI-IXT, S-BLR was clinically more successful than C-BLR. The postoperative NDD of S-BLR group was significantly different from that of C-BLR group. From 1 to 12mo after surgery, there was a statistically significant difference in near deviation between two groups.There was no significant difference in near stereopsis 12mo after surgery.
C-BLR is a common procedure for the treatment of CI-IXT[12].This surgical approach often results in suboptimal outcomes in patients with CI-IXT[13]. To improve the outcome of CIIXT surgery, clinicians have been seeking new or improved procedures to reduce NDD. For instance, the Sniret al[14]introduced S-BLR. Studies have shown that the upper and lower parts of the external rectus muscle are innervated and partitioned by different nerve abducent branches, providing a theoretical basis for S-BLR[15-16]. According to Scott’s theory[17], this surgical method can reduce NDD by balancing the tension of the upper and lower muscle fibers and achieve the synchronous correction of both near and distant deviations.Among these surgical designs, S-BLR has the highest success rate, reaching 92%[14], which is much higher than C-BLR[18],C-BLR combined with adjusting sutures, and enhanced C-BLR surgery[19-21]. Based on these studies, S-BLR can effectively reduce near and distant deviation as well as NDD.
In this study, the difference in postoperative NDD between the two groups was statistically significant, which provided evidence for the effectiveness of this approach. From 1 to 12mo after surgery, there were statistically significant differences between the S-BLR and C-BLR groups in their respective near deviations. Whereas there was no statistically significant difference between the two groups in the distant deviation at each time point after surgery. This difference may be related to the fact that the near deviation was greater before surgery than the distant deviation. Since CI-IXT is characterized by a near deviation greater than distant deviation by at least 10 PD,S-BLR effectively reduced NDD by balancing the tension of upper and lower muscle fibers. Comparatively, C-BLR has no such advantage. Therefore, there will be significant differences in near deviation between the two groups after surgery, while the difference in distant deviation remained statistically unaffected.
Fuet al[22]performed S-BLR on 29 patients with CI-IXT. Their results showed that S-BLR reduced the difference between near and distant deviations, with no obvious complications.Renet al[23]included 34 patients with CI-IXT and followed up for an average of 15on after S-BLR. Their results showed that the surgical success rate was 70.6%, and the of average near deviation was significantly reduced from preoperative(11.12±2.06) PD to postoperative (2.47±3.04) PD. These results indicated that this approach is an effective and safe method for the treatment of CI-IXT, which can decrease NDD and near deviation.
In a related report, Wanget al[4]followed up 44 patients in the S-BLR group and 57 patients in the C-BLR group for 3mo using a prospective study. They concluded that the NDD improvement in the S-BLR group was more obvious than that in the C-BLR group, and that the near deviation of the S-BLR group was significantly larger than that of the C-BLR group. There was also no statistically significant difference in distant deviation between the S-BLR and C-BLR groups either before or after surgery. Three months after surgery, the orthotopic rate of the S-BLR group was higher than that of the C-BLR group. These results showed that S-BLR was a safe and effective operation. Our present study was consistent with the conclusions of these other studies, in that the NDD improvement in the S-BLR group was more obvious than that in the C-BLR group. Moreover, the near deviation of the S-BLR group was significantly smaller than that of the C-BLR group after surgery, while the distant deviation was not statistically significant between the S-BLR and C-BLR groups either before or after surgery.
Chunet al[24]conducted a prospective non-randomized study and performed S-BLR in 55 patients with CI-IXT, with a success rate of 76%. Studies have found that the abducent nerve can be divided into distinct upper and lower branches in the human external orbital rectus muscle, innervating the upper and lower parts of the lateral rectus respectively[15]. In the primary position, the lateral rectus upper and lower muscle fiber length is equal, being approximately 40 mm. When concentrating at near reading eye position, the upper muscle fibers extend to 41.5 mm, while the lower muscle fiber length is reduced to 37.1 mm. This suggests that when in the near reading position, the lower part of the rectus muscle fibers shorten, resulting that the tension of lower muscle fibers is stronger than that of the upper muscle fibers. By slanting the lateral rectus, the tension of the upper and lower muscles is artificially balanced, so as to simulate a more balanced muscle relationship as in the primary position. Ultimately, this reduces the difference in the near, distant deviation and NDD[16,22].
This study was a double-blind randomized controlled trial that used a one-year follow-up to evaluate the final data set,was done in an independent laboratory. In the study design,C-BLR was used as the control group for treatment of CI-IXT.A randomized controlled study was conducted for the new surgical method for CI-IXT patients. This study had a good follow-up rate and good clinical trial treatment compliance.Due to the influence of the COVID-19 pandemic, the followup time of 5 patients at the 6-month post-operative time point was delayed by 2-3mo. Given this, there was a small degree of follow-up loss, resulting bias in this study. Despite this,we used telephone contacts to allow patients to have followup examinations as soon as possible after the outbreak had subsided.
In conclusion, S-BLR had better effects than C-BLR for the treatment of CI-IXT in near deviation and NDD, presenting as a safe and effective surgical procedure for the treatment of
CI-IXT.
ACKNOWLEDGEMENTS
Foundation:Supported by “323” Action Plan for Prominent Issues Affecting People’s Health of Hubei Province, Health Commission of Hubei Province, China.
Conflicts of Interest: Li YJ,None;Huang XQ,None;Yi BQ,None;Zhao YJ,None;Hu DWJ,None;Ma RT,None;Li WP,None;Ye MH,None;Zhou LH, None.
 International Journal of Ophthalmology2023年2期
International Journal of Ophthalmology2023年2期
- International Journal of Ophthalmology的其它文章
- Comment on: Amniotic membrane for covering high myopic macular hole associated with retinal detachment following failed primary surgery
- Trend of glaucoma internal filtration surgeries in a tertiary hospital in China
- Optical coherence tomography enhanced depth imaging of chorioretinal folds in patients with orbital tumors
- Trends in operating room-based glaucoma procedures at a single eye center from 2016-2020
- Comparison of biological behavior of lacrimal gland adenoid cystic carcinoma with high-grade transformation cells
- Small incision lenticule extraction and femtosecondassisted laser in situ keratomileusis in patients with deep corneal opacity: case series
