Optical coherence tomography enhanced depth imaging of chorioretinal folds in patients with orbital tumors
Zhi-Yu Peng, Lu Gan, Kang Xue, Akrit Sodhi, Xiao-Feng Ye, Hui Ren, Jiang Qian
1Department of Ophthalmology, Eye and ENT Hospital of Fudan University, Shanghai 200031, China
2Shanghai Key Laboratory of Visual Impairment and Restoration, Shanghai 200031, China
3Wilmer Eye Institute, Johns Hopkins University School of Medicine, Baltimore, MD 21287, USA
Abstract
● KEYWORDS: chorioretinal folds; orbital mass; enhanced depth imaging optical coherence tomography; choroidal thickness; inner/outer segment defects
INTRODUCTION
Orbital mass of all kinds would cause symptoms by mass effect mostly presenting as asymptomatic axial proptosis. And it would also influence visual acuity by optic nerve compression, retinal striae, hyperopia, increased intraocular pressureetc[1]. The timing of surgery for most benign tumors remains unclear. Take cavernomas, the most common benign orbital tumor as an example, surgery is performed to prevent putative visual damage by increasing the pressure of the cavernoma on visually vital structures, to debulk a cosmetically unsightly orbit and to obtain a histologic diagnosis, especially in cases where imaging cannot predict the kind of tumour[2-4].
Choroidal folds are produced by deformation of the globe where the expanding retrobulbar mass indents the sclera[5].Their relationship to visual acuity, visual prognosis and timing of surgery is not clear.
Enhanced depth imaging (EDI) optical coherence tomography(OCT) has been widely used for imaging the full-thickness of the choroid[6-8]. Herein, we conduct a prospective observational case series study to find the features of chorioretinal folds in orbital mass imaged using EDI OCT, in order to explore the role of chorioretinal folds in the mass effect and determine whether EDI spectral-domain optical coherence tomography(SD-OCT) could be a more sensitive measure of damage to the outer retina and could be a useful prognostic and/or diagnostic tool for patients with orbital masses.
SUBJECTS AND METHODS
Ethical ApprovalOur study protocol was approved by the Institutional Review Board of the Eye & ENT Hospital ofFudan University. Informed consent was obtained from all individual participants included in the study.

Table 1 Profile of patients included in the study
PatientPatients with intraorbital tumors indenting the sclera were included in the study (Figure 1). Those who had a history of previous vision-affecting eye disease or who required orbital exenteration or extensive tumor excision were excluded from the study.
Enhanced Depth Imaging SD-OCTImages were obtained in both eyes pre- and post-surgery. Considering axial length,myopia and to some extent age have a significant influence on choroidal thickness[9-10], the contralateral eye served as a control. The images were obtained by positioning an OCT device close enough to the eye to acquire an inverted image.Twenty sections were obtained within a 5×30° rectangle encompassing the macula and optic nerve, with 100 scans averaged for each section, and the horizontal section passing directly through the center of the fovea selected[11-12]. Postoperation EDI SD-OCT scans were performed using the follow-up mode. Inner segment/outer segment (IS/OS) defects were measured as the missing length of IS/OS layer. IS/OS defects and subfoveal choroidal thickness was measured manually on EDI SD-OCT images using the Image J tool(National Institute of Health, Bethesda, MD, USA). Choroidal thickness is the distance from the outer edge of the hyperreflective retinal pigment epithelium (RPE) to the inner sclera.
Statistical AnalysisStatistical software was IBM SPSS Statistics (version 26, USA). Descriptive statistics was performed to evaluate variations of choroidal thickness and Pearson correlation coefficient was applied to correlate choroidal thickness between both eyes. APvalue less than 0.05 was considered significant.
RESULTS
Totally 20 patients were included in this study. Patients’ profile was shown in Table 1. The mean age of the patients was 39.95 (range, 25 to 60)y, 11 (55%) were female and the rest 9(45%) were male. Totally 10 of the 20 patients were cavernous hemangioma, 3 cases were polymorphous adenomas of lacrimal gland, 4 cases were solitary fibrous tumor (SFT), 1 nerve sheath tumor, dermoidcyst, and squamous cell carcinoma of lacrimal cyst respectively. Two patients with cavernous hemangioma underwent intratumoral injection of bleomycin A5[13-14]and the rest patients received tumor excision. Patients were followed 1 to 14mo after surgery, 5.8mo on average.Visual acuity prior surgery ranged from 20/200 to 20/20 and 5 patients’ visual acuity remained the same after the surgery and the other 15 patients’ visual acuity was improved during follow-up. Among the 5 patients whose visual acuity was the same, 4 patients’ visual acuity was 20/20 at the first time. While the rest one whose visual acuity was 20/125 at presentation followed 1mo only. Photoreceptor IS/OS defect was found in 10 of all the patients and 8 of them fully recovered after excision of orbital mass, 2 were better (Figure 2). Visual acuity was improved in 9 of 10 patients with IS/OS defect after surgeries.And the rest one followed 1mo only and with papilloedema.Papilloedema was found in 6 patients whose visual acuity was lower than 20/32 at presentation and 3 of them did not present with IS/OS defect in EDI OCT. The subfoveal choroidal thickness prior surgeries was 225±15 μm, and the thickness increased 50±14 μm after surgeries. IS/OS defect was 51±20 μm on average at beginning. Both choroidal thickness and IS/OS defect are closely related to visual acuity (P<0.05).

Figure 1 Contrast-enhanced magnetic resonance image demonstrating an orbital cavernous hemangioma indenting the posterior sclera.
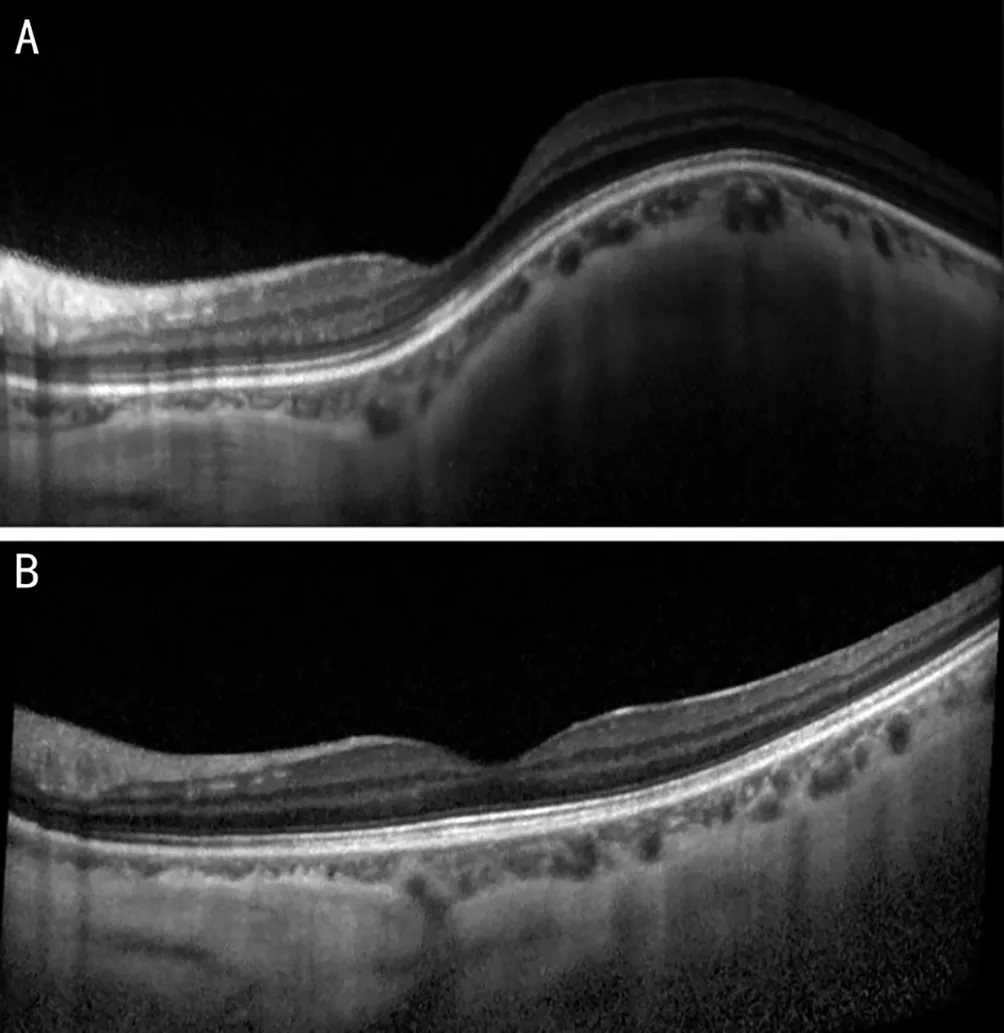
Figure 2 EDI OCT of the left eye of a 53-year-old female with cavernous hemagioma A: Before the surgery; B: Both chorioretinal folds and IS/OS defect improved a lot after 1mo post-surgery. EDI OCT: Enhanced depth imaging optical coherence tomography; IS/OS: Inner segment/outer segment.
DISCUSSION
Theoretically, orbital neoplasms of most kinds besides some kind of lymphomas like mucus associated lymphoid tissue lymphoma would ident the sclera resulting to the formation of chorioretinal folds if the tumor volume was big enough or it was growing right beside the eyeball. During the study, we encountered different kinds of orbital neoplasms including cavernous hemangioma, polymorphous adenoma,SFT, dermoidcyst, adenoid cystic carcinoma, embryonal rhabdomyoma, mesenchymal chondrosarcoma, nerve sheath tumor, squamous cell carcinoma. But some of them received orbital exenteration or extensive excision of the tumor which would influence the visual acuity and were excluded from the study. Cavernous hemangioma is the most commonly seen benign tumor in the orbit[15]and it is soft. So, the chorioretinal folds causing by cavernous hemangioma do not accompany IS/OS defect that often. Four out of 10 patients diagnosed with cavernous hemangioma in this study were with IS/OS defect. To the contrary, all of the 3 patients with polymorphous adenoma of lacrimal gland in the study were found with IS/OS defect in EDI OCT. And 3 of 4 patients with SFT in this study had IS/OS defect. It implies that those firm tumors might be more easily to cause IS/OS defect and the superior temporal location of the tumors is more easily to affect the fovea and result visual loss.
The choroid is a highly vascular structure with blood flow and thickness varying in relation to the intraocular pressure,perfusion pressure[16], endogenous nitric oxide production[17],vasoactive secretory production of choroidal ganglion cells[18-19], endogenous circulating catecholamines[20-23], and its intrinsic vasomotricity[24]. The choroidal layer is crucial for the metabolic function of the outer layers of the retina,including the RPE and photoreceptors[25-26]. The microvascular loss may decrease the ability of the choroid to supply proper levels of oxygen and other metabolites to the RPE and outer retina[11,27-30]. Zabenet al[31]reported a study to estimate the association between choroidal thickness in the macular area and retinal sensitivity in eyes with high myopia. And they found that retinal sensitivity in highly myopic eyes is directly correlated with choroidal thickness and does not seem to be associated with retinal thickness[10,31-32]. All these findings are consistent with current study. In this study, tumor indentations decreased the choroidal thickness and the choroidal thickness was slightly related to the visual acuity and IS/OS defect(Pearson correlation coefficient =-0.33).
On the other hand, patients included in this study do not have other eye diseases besides orbital tumor. After surgeries,when the compression was resolved most of IS/OS defect would recover except one patient with IS/OS defect as long as 375 μm at presentation and did not fully recovered after a 14-month follow up (Figure 3). It implies that some extent of IS/OS defect can be recovered if there was no further damage to the retina.
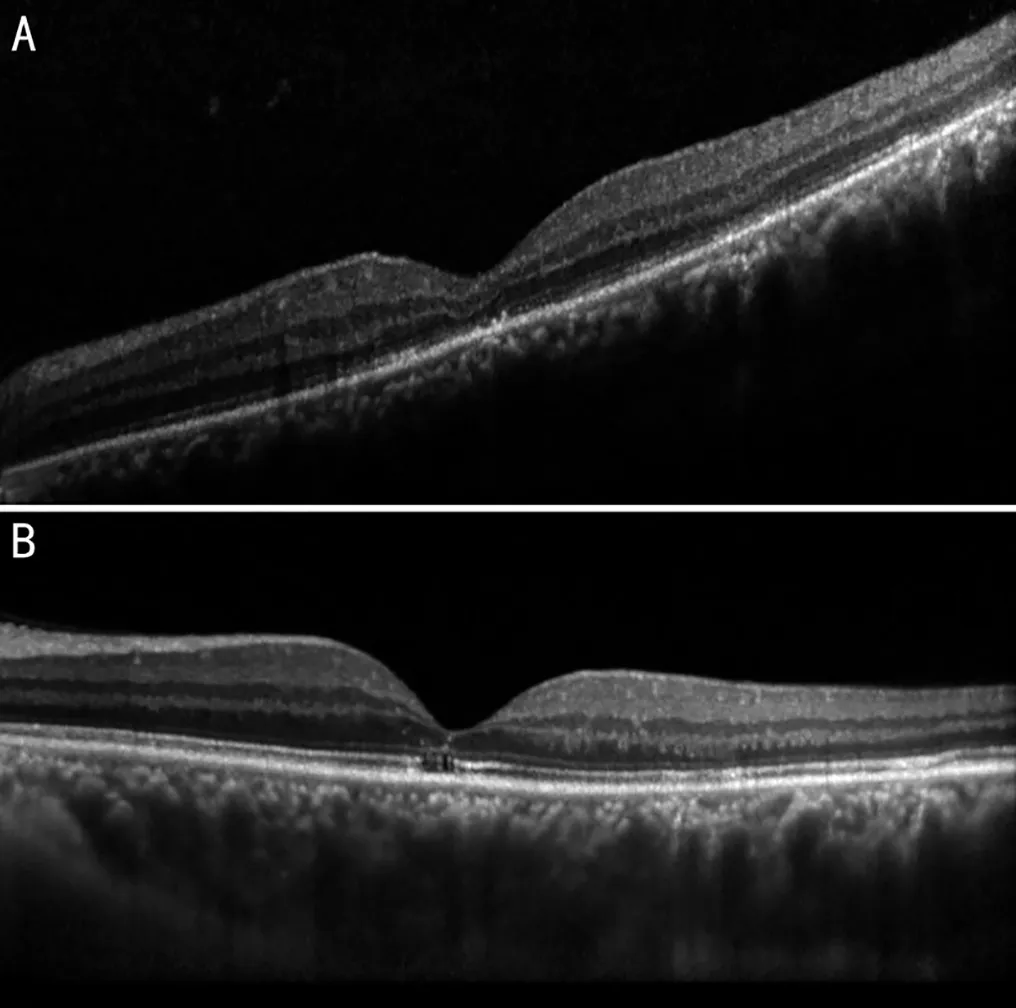
Figure 3 EDI OCT of the left eye of a 48-year-old male with polymorphous adenoma of lacrimal gland A: IS/OS defect measured as 375 µm was found in this patients before the surgical removal of the tumor.B: IS/OS defect did not fully recovered after 14mo post-surgery. EDI OCT: Enhanced depth imaging optical coherence tomography; IS/OS:Inner segment/outer segment.
Papilloedema was found in 6 patients whose visual acuity was lower than 20/32 at presentation and 3 of them did not present with IS/OS defect in EDI OCT suggesting that papilloedema was one of the causes beside IS/OS defect for visual loss in these patients.
Totally 4 patients’ visual acuity were 20/20 before surgery in this study even with the presentation of chorioretinal folds. And there were no obvious complains about their visual acuities at beginning. It might imply that even there are wrinkles of the retina the visual acuity might not be influenced dramatically without IS/OS defect.
In conclusion, decreased choroidal thickness as well as chorioretinal folds alone is not a necessity affecting visual acuity. Photoreceptor IS/OS defect caused by chronic compression of orbital mass is closely related to visual acuity,and it could recover in most of the patients but might not recover after surgery in a few patients. Besides, the presence of papilloedema, with or without IS/OS defect, suggests visual acuity damage. Identification of IS/OS defect in patients with chorioretinal folds using EDI-OCT might help to improve visual acuity to operate patients with orbital mass and choroidal compression as soon as possible.
ACKNOWLEDGEMENTS
Foundation:Supported byNational Natural Science Foundation of China (No.81300805).
Conflicts of Interest:Peng ZY,None;Gan L,None;Xue K,None;Sodhi A,None;Ye XF,None;Ren H,None;Qian J,None.
 International Journal of Ophthalmology2023年2期
International Journal of Ophthalmology2023年2期
- International Journal of Ophthalmology的其它文章
- Comment on: Amniotic membrane for covering high myopic macular hole associated with retinal detachment following failed primary surgery
- Trend of glaucoma internal filtration surgeries in a tertiary hospital in China
- Effects of slanted bilateral lateral recession vs conventional bilateral lateral recession on convergence insufficiency intermittent exotropia: a prospective study
- Trends in operating room-based glaucoma procedures at a single eye center from 2016-2020
- Comparison of biological behavior of lacrimal gland adenoid cystic carcinoma with high-grade transformation cells
- Small incision lenticule extraction and femtosecondassisted laser in situ keratomileusis in patients with deep corneal opacity: case series
