Comparative study of functional optical zone: small incision lenticule extraction versus femtosecond laser assisted excimer laser keratomileusis
Yao-Wen Song, Meng-Fan Cui, Yi Feng, Min Qu, Yan Gao, Rui He
1Department of Excimer Laser, Shanxi Eye Hospital, Taiyuan 030002, Shanxi Province, China
2The First Clinical Medical College, Shanxi Medical University,Taiyuan 030001, Shanxi Province, China
Abstract
● KEYWORDS: functional optical zone; small incision lenticule extraction; femtosecondlaser assisted excimer laser keratomileusis; spherical equivalent; spherical aberration
INTRODUCTION
In refractive surgery, the laser treated area is termed the optical zone, which considerably impacts postoperative visual quality. Effectiveness and safety of corneal refractive surgery have been greatly improved in recent years[1], leading to a higher standard for visual outcomes after surgery[2].Previous studies have investigated laser performance,centration, corneal thickness, repetition rate, biomechanics,and wound healing, and modifications were made for better surgical outcomes[3-4]. Moreover, the clinical application of small incision lenticule extraction (SMILE) surgery significantly improved postoperative visual outcomes[5-6].However, reduced functional vision under mesopic conditions in some patients is still a noteworthy problem. In cases where pupil size exceeds the laser ablation area, optical complications such as reduced night vision, halos, and glare can occur.Studies have shown that this is directly associated with the size of optical zone[7-8].
The size of the optical zone of human eyes is equal to the overlapping area between the pupil and cornea, which corresponds to the cornea area that light goes through to form images on the retina[9]. To ensure a smooth optical surface and optimal visual quality after refractive surgery, the laser treated area consists both an optical zone and a transition zone. The optical zone provides refractive correction, while the transition zone compensates for the abrupt change of corneal curvature and smooth the transition from optical surface to the untreated cornea[10]. The size of optical zone is the only modifiable parameter that determines postoperative visual outcome. The diameter of the intended optical zone is normally set at 6 to 7 mm, and it may vary according to the ablation modes. In practice, operation design usually takes various factors into consideration, such as pupil diameter, refractive error, and corneal thickness.
Visual quality is the highest at the central cornea and decreases towards periphery as a result of increased spherical aberration(SA). This “periphery effect” becomes even greater after myopic refractive surgery, because the margin of the laser treated area can increase SA, leading to lower visual quality than expected. Therefore, it is critical to improve postoperative visual quality by achieving adequate functional optical zone(FOZ). Recent clinical studies defined FOZ as the area of cornea surface that provides functional vision before or after laser treatment. FOZ features the lowest aberration and provides the best quality of vision at central cornea[11-12].Theoretically, postoperative FOZ is approximately identical to the correction area after the transition zone is set; however,previous studies have demonstrated that the actual optical zone after surgery was always smaller than expected, regardless of whether a transition zone exists or not[13-14]. It is important to accurately estimate the size of FOZ. This can not only provide valuable information for operation design, but also reduce or even avoid postoperative complications, which is critical in ensuring excellent postoperative visual quality. To date,there are limited studies investigating the size of FOZ and its associated factors in SMILE surgery. Meanwhile, femtosecond laser assisted excimer laser keratomileusis (FS-LASIK)is expected to remain as one of the mainstream refractive surgeries for a considerable period of time due to its accuracy,safety and low costs. Thus, the aim of this study is to analyze and compare the changes of FOZ after SMILE and FS-LASIK surgeries and explore the potentially associated factors, in an effort to provide some useful information for operation design in clinical practice.
SUBJECTS AND METHODS
Ethical ApprovalThis study was approved by the Ethics Committee of Shanxi Eye Hospital (approval No.SXYYLL-20211201), and all subjects signed the informed consent.
Study DesignThis case-series study retrospectively enrolled 133 patients (262 eyes) with myopia or myopic astigmatism aged 18 to 43y (25.81±5.38y) who received corneal refractive surgery between November 2018 and July 2021 at Shanxi Eye Hospital.
Inclusion criteria were: 1) regular corneal shape before and after surgery; 2) no severe dry eye by tear function tests; 3)transparent cornea with no nebula or macula; 4) discontinuing soft contact lens wear for over 2wk, hard contact lens wear for over 1mo or orthokeratology lens wear for over 3mo prior to the procedure; and 5) being able to attend postoperative follow-up visits for at least 3mo.
Ophthalmic ExaminationsAll patients underwent routine preoperative ophthalmic examinations including preoperative uncorrected visual acuity (pre-UCVA), preoperative best corrected visual acuity (pre-BCVA), postoperative uncorrected visual acuity (post-UCVA), postoperative best corrected visual acuity (post-BCVA), slit lamp examinations, intraocular pressure measurements, and fundus examinations. Central corneal thickness (CCT) was measured using RTVue anterior segment OCT (Optovue, Inc., California, US). Pentacam 3-demensional anterior segment analyzer (Pentacam 70900,Oculus Inc., Germany) was used to acquire and measure mean keratometric value (Km), SA within the central 8 mm area, and aspherical parameterQ-value.
Functional Optical Zone MeasurementAll measurements were done by an experienced technician before and 3mo after surgery. Planned functional optical zone (PFOZ) for all eyes was 6.5 mm. The average of 3 acceptable measurements (i.e.,image quality parameter >95%, diameter of analyzed area>8 mm, and misalignment<0.3 mm from pupil center) was recorded for each eye. The achieved functional optical zone(AFOZ) was measured on the Power Distribution screen of Pentacam 3-D analyzer, with pupil center as the center,selecting “ring” to obtain total corneal refractive power(TCRP). The diameter of the ring was adjusted using the mouse. According to Fuet al[15], the AFOZ was defined as the largest ring diameter when the TCRP did not exceed 0.5 D more than that at the central 4 mm of the cornea (Figure 1).
Surgical Procedure and Postoperative ManagementAll procedures were performed by 3 highly experienced refractive surgeons (Feng Y, Qu M, and He R). After prepping and draping, proparacaine hydrochloride eye drops was instilled for topical anesthesia. The conjunctival sac was irrigated with balanced salt solution following insertion of a speculum.Ophthalmic sponge was used to dry the cornea.
All SMILE procedures were performed with VisuMax Femtosecond laser system (Carl Zeiss Meditec, Jena, Germany).A repetition rate of 500 kHz and pulse energy of 135 nJ were applied. The diameter of PFOZ was set at 6.5 mm. The intended thickness of cornea cap was 120 μm with an intended diameter of 7.5 mm. A 2.5 mm incision was made superiorly on the cornea. Intraoperative laser treatment sequence was as follows: lenticule interface, lenticule side-cut, cap interface,and small incision. After completion of the femtosecond cutting, the cap and lenticule were manually separated and the lenticule was extracted. Postoperatively, patients received gatifloxacin eye drops (Laoboyuntang Pharmaceutical Co.,Ltd., Chuxiong, China) 4 times daily for 14d and loteprednol eye drops (FREDA Pharmaceutical Co., Ltd., Jinan, China)4 times daily for 1wk followed by steady tapering over the subsequent 3wk.
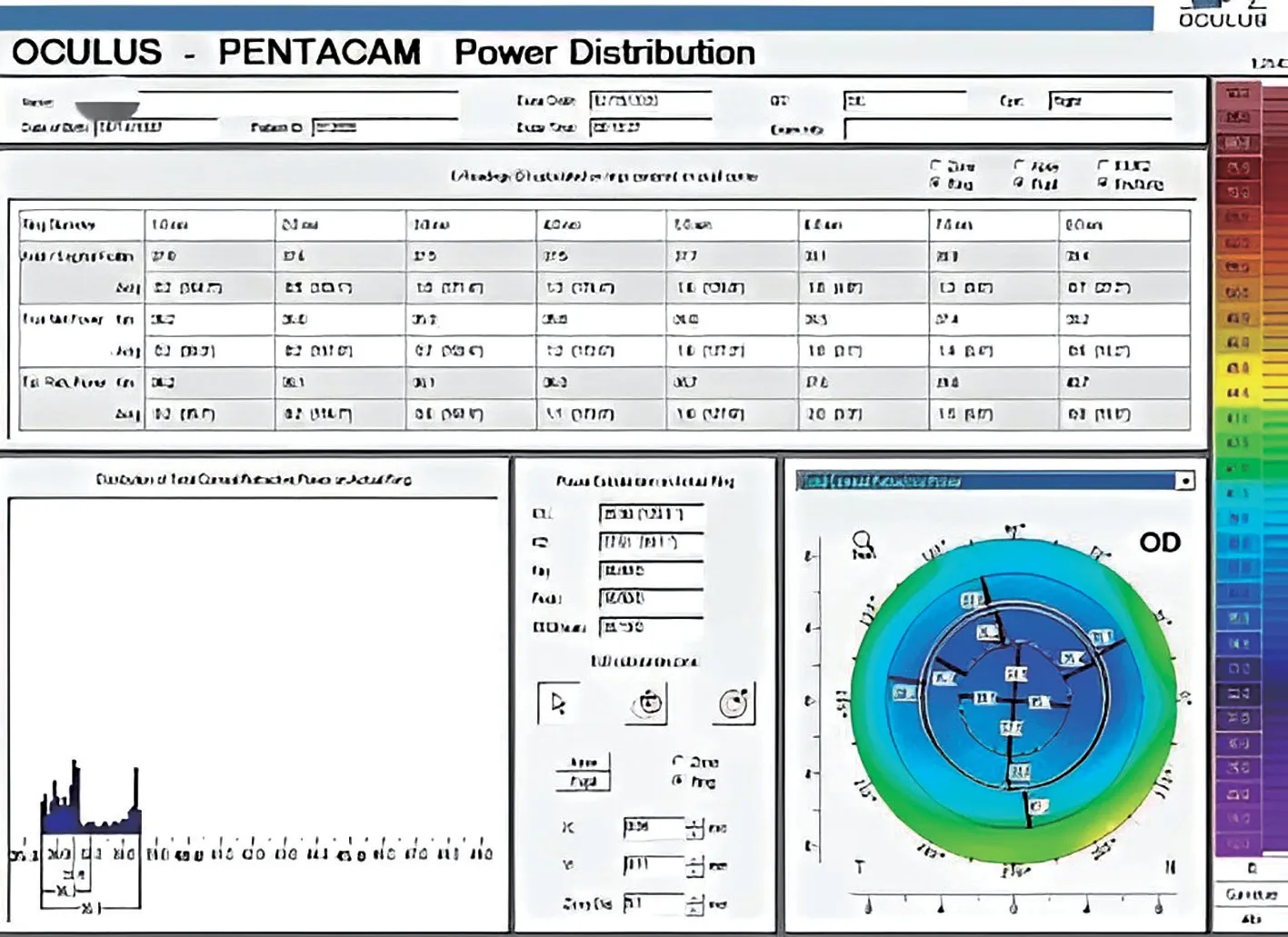
Figure 1 Pentacam power distribution screen The zone diameter was recorded when the actual ring Km was 0.5 D higher than the total refractive power at the central 4 mm of the cornea. This value was regarded as the diameter of achieved functional optical zone.
In the FS-LASIK group, flaps were cut using the FEMTO LDV femtosecond laser system (Ziemer. Ophthalmic Systems Group, Port, Switzerland), with energy set at <100 nJ,repetition rate set at <2 MHz, spot diameter set at <2 μm, and suction vacuum pressure set at 740 mbar. The diameter of the optical zone was planned to be 6.5 mm. The hinge was located superiorly with a width of 4.4 mm and a length of 0.6 mm. The applanation head was kept horizontal and placed properly on the cornea by manipulating the joystick. The assistant pressed“apply vacuum” to initiate suction and then “start resection” to initiate laser ablation. The flap was lifted to expose stroma bed after ablation was completed. Particle free LASIK sponge was used to fully absorb fluid on the corneal surface. WaveLight EX500 Excimer laser (Alcon Inc., US) performed corneal ablation for desired refractive correction. After treatment, the eye and the flap were irrigated with balanced salt solution,followed by reposition of the flap. A bandage contact lens was placed afterwards. The postoperative medication regimen was the same as that in SMILE group.
Statistical AnalysisPower analysis was performed using Minitab software (Version 20; State College, PA, USA)to verify the adequacy of the sample sizes in each group.Considering the impact of optical diameter on vision, we applied a difference of 0.1 mm between the two groups, and the power value was set at 0.95, with a significance level of 0.05. Statistical analysis was done by SPSS (IBM, Armonk,NY, USA, version 20). Continuous variables were normally distributed as determined by Kolmogorov Smirnov test and expressed as mean±SD. Pairedt-test was performed to compare pre- and post-operative data in each group, and independent samplet-test was used to compare inter-group differences. Pearson correlation analysis and multiple variable linear regression were performed to determine the relationship between △FOZ and associated factors.P<0.05 was considered statistically significant.
RESULTS
Basic InformationPreoperative spherical refractive error ranged from -0.50 to -8.00 D (-5.22±1.59 D); cylinder power ranged from 0 to -3.00 D (-0.87±0.69 D); spherical equivalent(SE) ranged from -0.75 to -9.00 D (-5.66±1.64 D). Patients entered either SMILE group (123 eyes) or FS-LASIK group(139 eyes) based on their own preferences.
Preoperative Comparisons Between the Two GroupsPower analysis results showed that both SMILE group and FS-LASIK group had adequate sample size. Table 1 shows basic information of the SMILE group and FS-LASIK group.
The differences of age, pre-UCVA, pre-BCVA, SE, CCT, Km,Q-value, and SA were not statistically signifciant between the two groups (allP>0.05).
Postoperative Comparisons at 3moThe SMILE group had better post-UCVA than the FS-LASIK group (P=0.002), while post-BCVA showed no significant differences between the 2 groups (P=0.988). FOZ in both groups reduced remarkably at 3mo after surgery compared with that before surgery (P<0.001for both groups). Given the same preoperative optical design,the decrease of FOZ was 1.45±0.27 mm in SMILE group and 1.67±0.25 mm in FS-LASIK group,i.e., FOZ was larger in SMILE group (P<0.001). Moreover, the differences of CCT, Km,Q-value and SA between the two groups were all statistically significant (allP<0.001), whereas SE showed no significant difference (P=0.098). Table 2 shows all parameters at 3mo after surgery for the two groups.

Table 1 Comparison of preoperative basic information between the two groups mean±SD
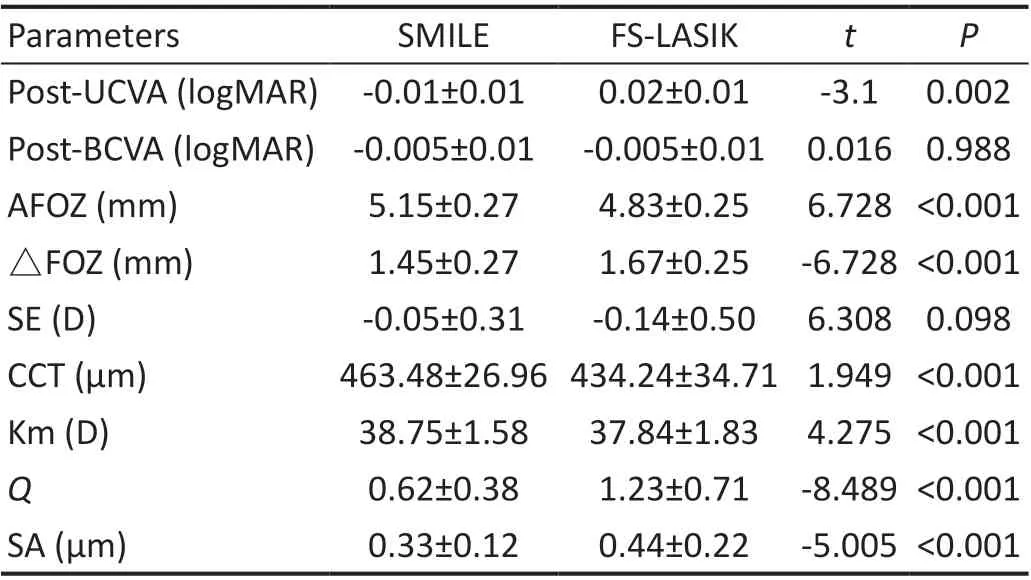
Table 2 Comparisons of parameters at 3mo after surgery between the two groups mean±SD
Changes in Functional Optical Zone and Correlation with its Associated Factors Correlation analysis was performed to explore the relationship between the variation of FOZ(△FOZ) and its associated factors. The results showed that preoperative SE was negatively correlated with postoperativeFOZ (P<0.001; Figure 2), while variation of CCT (△CCT),variation of Km (△Km), variation ofQ-value (△Q), and variation of SA (△SA) were all positively correlated with△FOZ (allP≤0.001; Figures 3-6).
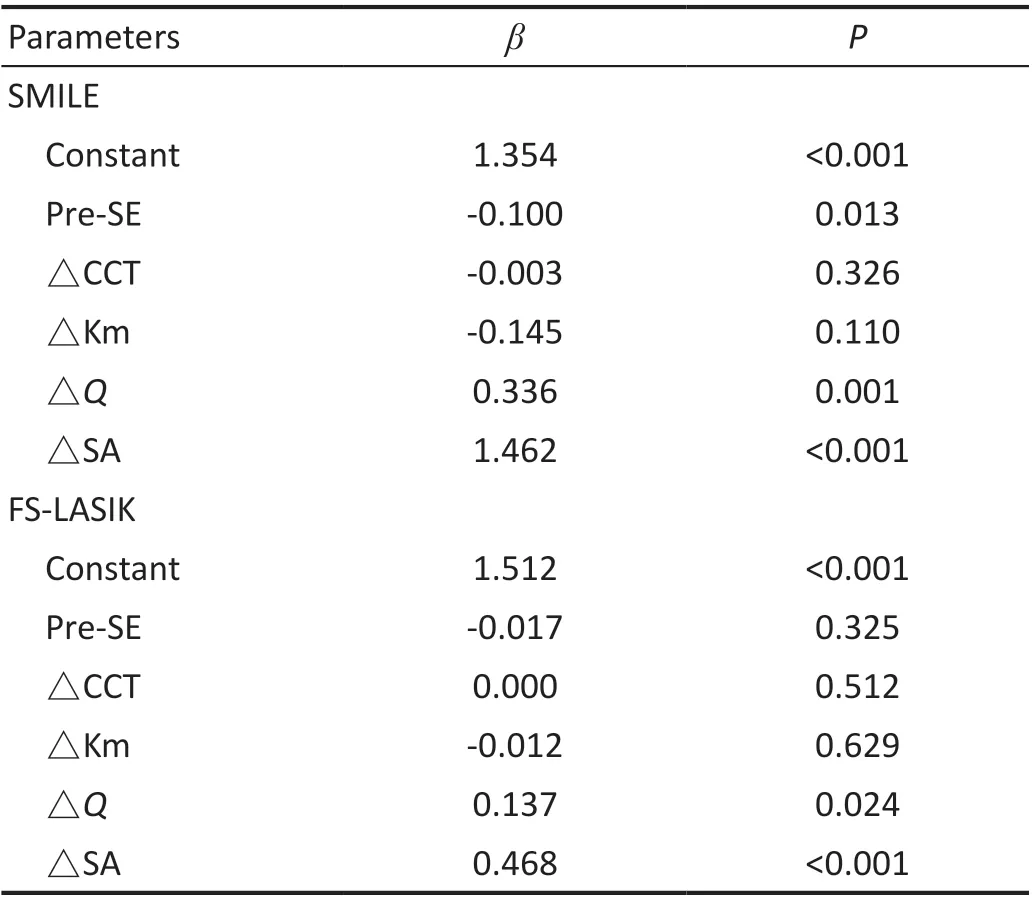
Table 3 Multiple variable linear regression analysis for △FOZ
Multiple Variable Linear Regression Model for FOZ at 3mo Given that preoperative SE, △CCT, △Km, △Q,and △SA were all associated with △FOZ, a multiple variable linear regression model was generated with these variables by Enter method for each surgical technique.The results showed that preoperative SE, △Q, and △SA significantly impacted postoperative FOZ in SMILE group.The regression equation was △FOZ=1.354-0.1×pre-SE+0.336×△Q+1.462×△SA. In FS-LASIK group, △Qand △SA were significant correlated to FOZ. The regression equation was △FOZ=1.512+0.137×△Q+0.468×△SA. Table 3 shows detailed analysis results.
DISCUSSION

Figure 2 Correlation between △FOZ and preoperative SE for SMILE and FS-LASIK groups FOZ: Functional optical zone; SE: Spherical equivalent; SMILE: Small incision lenticule extraction; FS-LASIK:Femtosecond laser assisted excimer laser keratomileusis.

Figure 3 Correlation between △FOZ and △CCT for SMILE and FSLASIK groups FOZ: Functional optical zone; SE: Spherical equivalent;SMILE: Small incision lenticule extraction; FS-LASIK: Femtosecond laser assisted excimer laser keratomileusis.
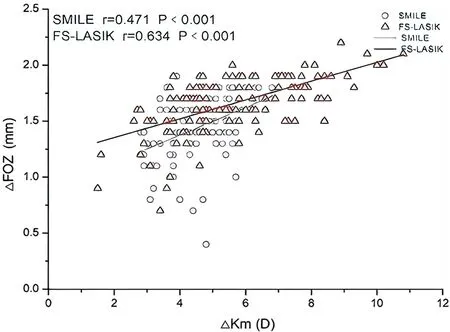
Figure 4 Correlation between △FOZ and △Km for SMILE and FSLASIK groups FOZ: Functional optical zone; SE: Spherical equivalent;SMILE: Small incision lenticule extraction; FS-LASIK: Femtosecond laser assisted excimer laser keratomileusis.

Figure 5 Correlation between △FOZ and △Q for SMILE and FSLASIK groups FOZ: Functional optical zone; SE: Spherical equivalent;SMILE: Small incision lenticule extraction; FS-LASIK: Femtosecond laser assisted excimer laser keratomileusis.

Figure 6 Correlation between △FOZ and △SA for SMILE and FSLASIK groups FOZ: Functional optical zone; SE: Spherical equivalent;SMILE: Small incision lenticule extraction; FS-LASIK: Femtosecond laser assisted excimer laser keratomileusis.
To date, there is no specific standard for measuring FOZ.Based on previous studies, measuring optical zone with corneal topography is a relatively direct method. In an earlier study, Partal and Manche[16]chose the color representing the highest curvature on the true color map as the rim of the optical zone measurement, and they used the internal scale system of the topography program to measure the horizontal and vertical diameters. In another study, Holladay[17]used local radius of curvature (ROC) map on the topographer and determined the enclosed area by the outer edge of the yellow zone as FOZ, corresponding to 2 color changes (from green to yellow) or 0.5 D steepening from the mean central radius.For a 6 mm PFOZ, the resulting AFOZ was 5.4 mm for -5.0 D myopia correction. Racine[13]used the refractive map of the Humphrey Atlas Topography system to measure the FOZ.They used the cursor on the computer screen instead of the color-coded scale to locate the measuring area. Periphery points at which a corneal power change of 0.50 D from pupil center were identified and used to outline the ablation area. The long and short axes of the ellipse were measured. On the other hand, Taberneroet al[11]compared optical zones measured by different methods and concluded that calculating the FOZ with corneal curvature measured by topographer was the most practical method. Therefore, in this study, we measured AFOZ by corneal topographer, and adopted a 0.50 D corneal power change from the pupil center to determine the margin. Our methods were consistent with aforementioned studies.
Findings of the present study showed that AFOZ decreased significantly compared with preoperative FOZ and PFOZ in both groups, which was consistent with previous studies.In SMILE group, AFOZ was 5.15±0.27 mm, which was 1.45±0.27 mm smaller than PFOZ. We searched for published studies that also measured AFOZ after SMILE surgery with Pentacam Power Distribution. The study by Qianet al[18]showed a postoperative AFOZ of 4.75±0.52 mm when the PFOZ was set as 6.5 mm. Their AFOZ results were smaller than those in our study, which might be attributable to a highly myopic population in their study (all preoperative SE ≤-10.0 D).Dinget al[19]divided patients into low astigmatism (≤-0.5 D)and high astigmatism (≤-2.0 D) groups; postoperative AFOZ at 6mo were 5.17±0.21 and 5.16±0.41 mm respectively. The result was comparable with findings at 3mo in our study,suggesting that AFOZ becomes stable at about 3mo after surgery. Qianet al[14]also used 6.5 mm as the preoperative PFOZ, but they defined postoperative AFOZ as the largest ring diameter when the difference between the mean ring power and the pupil center power was ≤1.50 D. Surprisingly, their study yielded a mean AFOZ of 5.09±0.83 mm, which was similar to the present study. Meanwhile, in the present study,AFOZ at 3mo postoperatively was 4.83±0.25 mm, which was 1.67±0.25 mm smaller than PFOZ in FS-LASIK group.In a previous study, Camellinet al[20]performed LASEK and Epipolis laserin situkeratomileusis (EPI-LASIK) surgeries using the aspherical ablation mode of excimer laser, and calculated AFOZ by corneal aberration. Their results showed that for planned optical zones <6.75 mm, the achieved optical zone was 0.25 mm smaller than expectation, and planned optical zones>6.75 mm result in effective optical zones at least as large as the planned optical zone. However, they used corneal surface aberration to define FOZ, whereas in this study,we calculated FOZ by TCRP. The results of these two studies can not be directly compared.
The reduction of FOZ after surgery might be associated with changes of the corneal curvature, wound healing, and variation of corneal biomechanics[21-22]. For SMILE surgery, as a result of operation design considerations and the need of lenticule extraction, the edges of the laser ablation area tend to be sharp,avoiding loss of laser energy when cutting the peripheral area.In theory, the diameter of the lenticule should be equivalent to the actual FOZ. For FS-LASIK, however, intrastromal ablation by excimer laser leads to more energy being transmitted to the adjacent tissue, hence a more remarkable wound healing response[23-24]. The relatively low laser energy applied in SMILE procedures can effectively mitigate postoperative corneal inflammation and stroma remodeling effect[25], which may contribute to the larger AFOZ in SMILE group.
According to Yinget al[26], change in corneal asphericity is the main reason for the reduction of FOZ after excimer laser refractive surgery. Our findings suggested that △Qand △SA were positively correlated with the extent of FOZ reduction.In other words, a more spheroidal postoperative cornea shape would result in a larger SA increment and a smaller FOZ size.SMILE surgery has less impact on the anterior cornea than FS-LASIK surgery, which might be another explanation for the larger AFOZ in SMILE group. Compared with FS-LASIK group, SMILE group had lowerQand SA values and better visual quality. Therefore, post- UCVA was better in the SMILE group than the FS-LASIK group.
Whether the variation of FOZ is associated with refractive error is still controversial. Study by Damgaardet al[27]demonstrated that AFOZs after both SMILE and FS-LASIK surgeries were not significantly associated with intended refractive correction. Qianet al[14]also found that magnitude of myopic refractive error was not related to AFOZ for SMILE,but when refractive error exceeded 7.50 D, postoperative FOZ could be significantly smaller. Our study found that higher preoperative SE was associated with smaller postoperative FOZ; multiple variable linear regression analysis showed that that preoperative SE negatively influenced AFOZ in SMILE group. Considering the indications of SMILE surgery, we did not enroll any patients with over -10.0 D of myopia. This study, therefore, lacked data on highly myopic population,and further studies with larger sample size and wider range of refractive error are warranted to investigate the relationship between FOZ and refractive power.
In conclusion, FOZ reduction can occur after both SMILE and FS-LASIK surgeries. Compared with FS-LASIK group,patients in SMILE group achieved larger postoperative FOZ,which was associated with preoperative refractive error and postoperative change in corneal asphericity. Future studies are needed to explore the impact of variation of FOZ after corneal refractive surgery on vision quality, especially that on night vision.
ACKNOWLEDGEMENTS
Foundation:Supported byScientific and Technological Innovation Programs of Higher Education Institutions in Shanxi (No.2022L201).
Conflicts of Interest: Song YW,None;Cui MF,None;Feng Y,None;Qu M,None;Gao Y,None;He R,None.
 International Journal of Ophthalmology2023年2期
International Journal of Ophthalmology2023年2期
- International Journal of Ophthalmology的其它文章
- Perspectives and clinical practices of optometrists in Saudi Arabia concerning myopia in children
- Progression of myopia among undergraduate students in central China
- Flipped classroom approach to global outreach: crosscultural teaching of horizontal strabismus to Chinese ophthalmology residents
- Topical ketotifen treatment for allergic conjunctivitis: a systematic review and Meta-analysis
- Pseudomembranous conjunctivitis in a patient with DRESS syndrome
- Two cases of persistent shallow anterior chamber after cataract surgery combined with goniosynechialysis
