Should ocular Demodex be checked and treated in refractory keratitis patients without blepharitis?
Ying-Ying Gao, Ting Wang, Yu-Ting Jiang, Ming-Jun Yang, Xiu-Hai Lu, Ling Zheng,Shu-Ting Wang, Wei-Yun Shi
1Department of Ophthalmology, the Second Affiliated Hospital, Fujian Medical University, Quanzhou 362000, Fujian Province, China
2Eye Hospital of Shandong First Medical University, Jinan 250021, Shandong Province, China
3State Key Laboratory Cultivation Base, Shandong Provincial Key Laboratory of Ophthalmology, Shandong Eye Institute,Shandong First Medical University & Shandong Academy of Medical Sciences, Qingdao 266071, Shandong Province,China
Abstract
●KEYWORDS: Demodex; keratitis; blepharitis; slit-lamp microscopy
INTRODUCTION
As early as 1971,Demodexwas disclosed to be implicated in blepharitis[1]. In 2005, Gaoet al[2]found that 100% of the people with cylindrical dandruff in the eyelash hadDemodexmites. There has been an increasing amount of evidence to support thatDemodexis an important cause of blepharitis and related ocular surface diseases[3-11]. In 2018, Lianget al[12]reported thatDemodexcaused blepharitis-associated keratoconjunctivitis, and the extent of keratopathy was related to the severity of blepharitis. In our practice, it was noticed that a high percentage of patients with refractory keratitis presented with a high density ofDemodexinfection despite the relatively clean eyelashes and no sign of blepharitis. This phenomenon is easy to be ignored by clinicians. We speculate that recurrence of keratitis might be related toDemodexinfestation. In the absence of appropriate treatment, the keratitis might become refractory. In this study, we used a modified slitlamp illumination technique for a quick assessment of ocularDemodex. We also achieved good results following mite killing therapy and discussed the pathogenesis of demodicosis.
SUBJECTS AND METHODS
Ethical ApprovalThis study was approved by the Ethics Committees of the Eye Hospital of Shandong First Medical University (20171031-3) and the Second Affiliated Hospital of Fujian Medical University (2016-53) and carried out according to the tenets of Declaration of Helsinki. Informed consent was obtained from each participant.
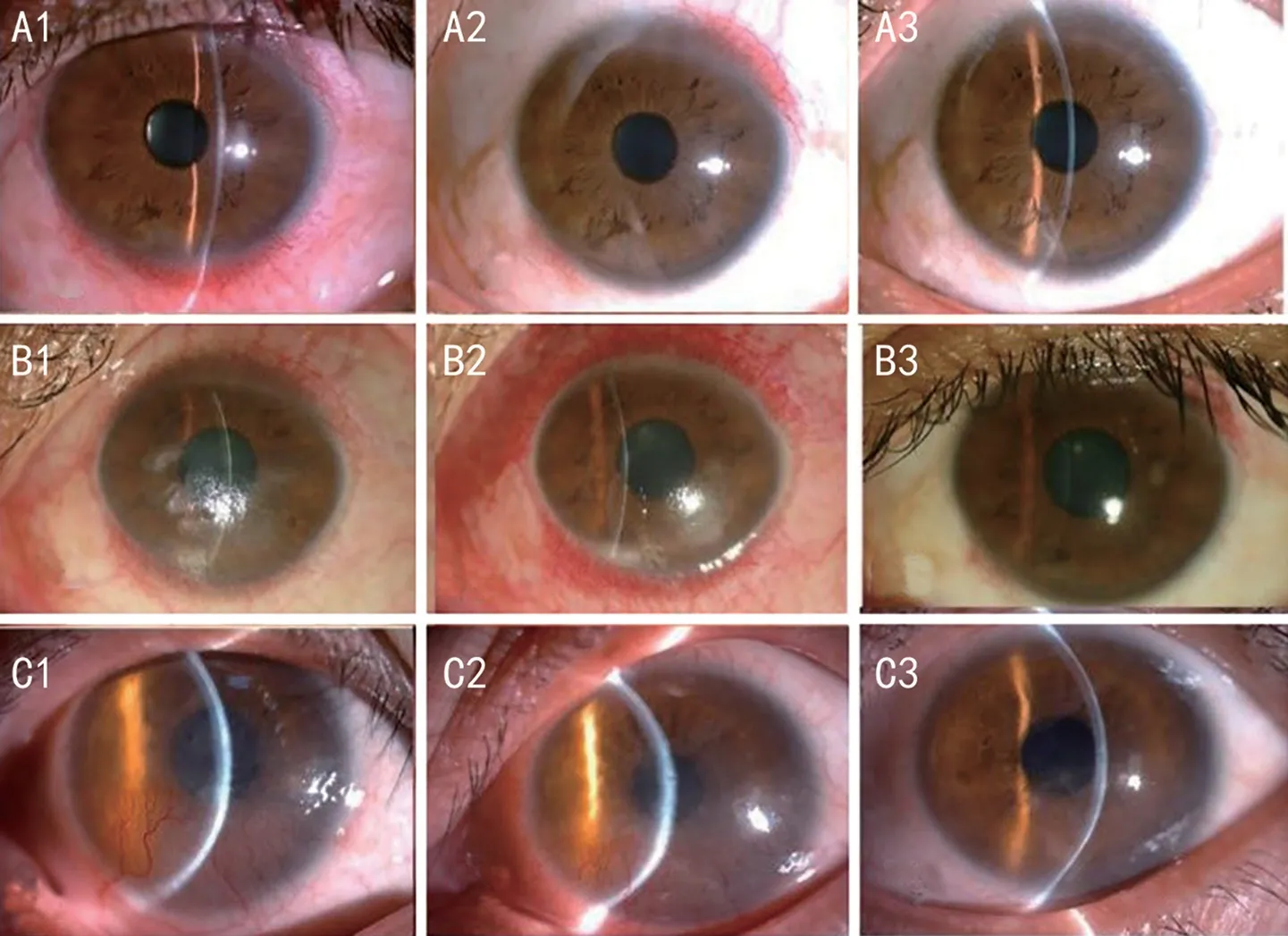
Figure 1 The severity of the cornea lesion was graded Mild: Infiltration was limited within the superficial corneal stroma with a diameter of the cornea lesion ≤4 mm (A1). Moderate: Limited corneal neovascularization might exist, corneal infiltration was in the superficial stroma, and the diameter of the cornea lesion ranged from 4 to 8 mm (B1). Severe: Infiltration was in the deep stroma accompanied by neovascularization,and/or the diameter of the cornea lesion was >8 mm (C1). A2, B2, and C2 present the outcomes at 2wk, and A3, B3, and C3 present the outcomes at 1mo after the treatment in the case of A1, B1, C1, showing the congestion subsided, most of the neovascularization disappeared,and the corneal infiltration was absorbed.
PatientsA total of 120 individuals were enrolled in this prospective study from January 2018 to May 2019. Forty of them, including 30 patients from the Eye Hospital of Shandong First Medical University and 10 patients from the Second Affiliated Hospital of Fujian Medical University, had refractory keratitis with or without combined blepharitis. Five patients developed bilateral keratitis, while 35 patients were unilaterally affected. All of these patients had been treated at the same hospital from the onset of the keratitis by the same medical team. Eighty healthy controls were from the Physical Examination Center of the Second Affiliated Hospital of Fujian Medical University.
Diagnosis of Refractory Keratitisand BlepharitisAnterior segment photographs of all patients were evaluated by two observers. When symptoms and signs of keratitis such as ocular pain, redness, photophobia, tearing, and different degrees of vision loss prevailed for more than 2mo, as well as slit-lamp examination showed infiltrates, epithelial defects, and ulcers on the cornea despite eyelid hygiene and the topical administration of artificial tears, antibiotics, antivirals, and anti-inflammatory and immunosuppressive agents, refractory keratitis was diagnosed.The severity of the corneal lesion was graded as mild if the infiltration was limited within the superficial corneal stroma and the cornea lesion was in a diameter of ≤4 mm (Figure 1A1), as moderate if there was infiltration in the superficial stroma, with or without limited corneal neovascularization, and the cornea lesion was in a diameter of 4 to 8 mm (Figure 1B1), and as severe if the infiltration existed in the deep stroma accompanied by neovascularization, and/or the diameter of the corneal lesion was >8 mm (Figure 1C1). When patients developed bilateral keratitis, the severity grade of the more severe eye was obtained for statistical analysis. Blepharitis was diagnosed when there was crusting at the lash root as well as congestion, thickening,and swelling at the lid margin.
Exclusion Criteria for Patients with Keratitis and the Normal Control GroupPatients with any of the following conditions as confirmed by slit-lamp microscopy, corneal sensation measurement or dry eye testing (data not shown) were excluded from this study: 1) acute infectious keratoconjunctivitis and corneal ulceration; 2) herpes simplex keratitis (with typical corneal morphological features and failure of previous antiviral treatment); 3) neurotrophic keratopathy (with corneal sensation no less than 20 mm as detected by the Cochet-Bonnet esthesiometer); 4) corneal dystrophy; 5) Sjögren Syndrome dry eye, other autoimmune-related diseases, and diabetic melitus;6) corneal degeneration caused by various reasons; 7) a history of ocular surgery; 8) contact lens wearers. Volunteers who had recurrent eye discomfort, congestion of the eyelid margin,positive corneal staining or previous ocular surgery were excluded from the normal control group.
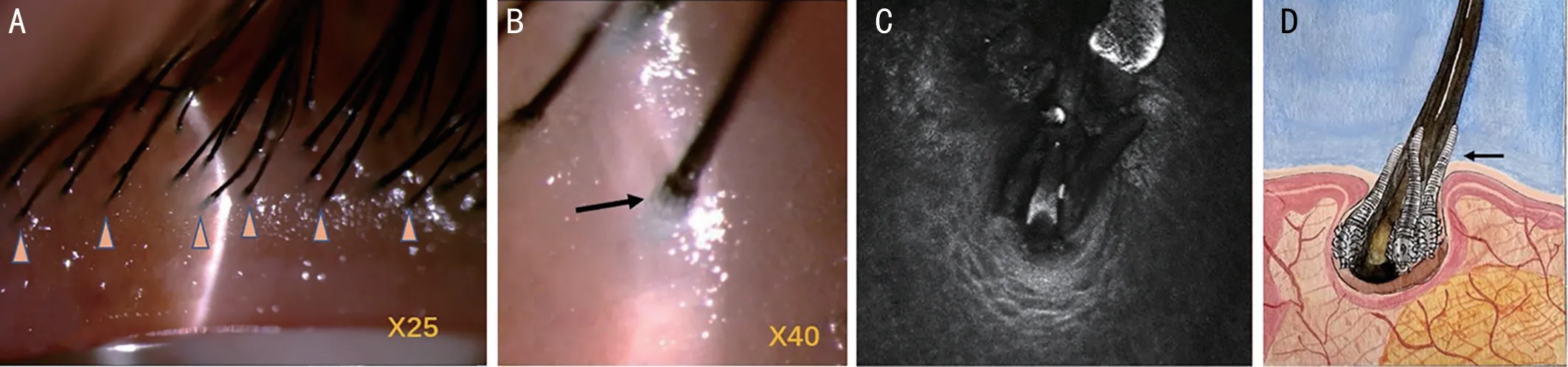
Figure 2 Illustration of Demodex at the lash roots A: Under a slit lamp microscope, six lashes of the inner line in the middle of the upper lid were observed; B: Tails of the Demodex mite were distinguished by observing translucent rod-like sticks extending above the skin surface closely to the eyelash follicles at a magnification of 40×; C: An in vivo confocal microscopic image of the Demodex tails; D: A painting demonstrates the scenario.
Judgment and Ranking of OcularDemodexInfestationWe modified the reported sampling and counting method for detection ofDemodex[2].Under a slit lamp microscope (Topcon,Tokyo, Japan), six lashes of the inner line in the middle of the upper lid of each participant (Figure 2A triangles) were observed. Tails of theDemodexmite were distinguished by observing translucent rod-like sticks extending above the skin surface closely to the eyelash follicles at a magnification of 40× (Figure 2B arrow). The severity ofDemodexinfestation ranked as none, mild, moderate, and severe. The mild degree was defined when there was 1 or 2 lashes showingDemodextails. The moderate degree was defined when there were 3 or 4 lashes showingDemodextails. The severe degree was defined when there were 5 or 6 lashes showingDemodextails.In vivoconfocal microscopy (IVCM) ofDemodexin the eyelash follicles at the middle part of the upper eyelid was performed in 40 patients[13].
Other ExaminationsBacterial smear and culture of the conjunctival sac and corneal lesion were performed in all patients with keratitis. Inflammatory cells and other pathogens in the cornea were observed by IVCM. Infiltration and the depth of cornea lesion were recorded on anterior segment optical coherence tomography.
Preparation of 5% Tea Tree Oil OintmentBecause the tea tree oil ointment (TTOO) and other mite killing agents for ophthalmic usage are not commercially available in China, 5% TTOO was prepared by the researchers following strict instructions. Briefly, 100% tea tree oil purchased from Essential Oil Company (Portland, OR, USA) was mixed with sterilized white petrolatum (Tianjin Zhiyuan Chemical Reagent Co., Tianjin, China) to achieve a concentration of 5% (vol/vol)in an aseptic container.
TreatmentsLid scrubs with 5% TTOO were recommended to be performed by patients with keratitis at home. After the face,eyelids, and hands were washed and cleaned, a small dollop of 5% TTOO was placed on the middle finger (or index finger) of both hands. Both eyes were closed loosely and simultaneously massaged at the lid margins in a nasal to temporal direction for 5min, twice daily, and the ointment was left overnight[14].The previous medical therapy with artificial tears, 0.1%fluorometholone eye drops, and/or immunosuppressant(cyclosporine A or FK-506) eye drops four times a day was continued. The combined treatment lasted for 8wk, during which the patients were seen every 2wk, and steroid eye drops were tapered according to the intraocular pressure and the changes of ocular inflammation. If the corneal ulceration and epithelial defect were not completely healed, the treatment was extended for up to three months. Follow-up evaluations were completed 8 to 12wk later. The severity ofDemodexinfestation was recorded at 8wk.
Statistical AnalysisThe normally distributed continuous variables were reported as means±SD.χ2test was used to analyze the gender difference, severity of keratitis, and prevalence ofDemodexbetween groups. Kruskal-WallisHtest was used to analyze the difference in age. Spearman correlation test was used to analyze the degree of demodicosis and corneal lesion. Statistical analyses were performed with SPSS 19.0 (Microsoft, Redmond, WA, USA), withP<0.05 being considered significant.
RESULTS
The age of the patients with refractory keratitis ranged from 17 to 50 years old. There was no difference in age (median,38yvs40y) and gender (male:female, 18:22vs40:40) between the keratitis group and the control group (bothP>0.05).
Before treatment,Demodextails were found in all patients(40/40, 100%), compared to 53% (42/80) of the controls(χ2=27.8,P<0.01). IVCM confirmed that all patients with keratitis hadDemodexinfestation. This was same as the slit lamp observation results (Figure 2C, 2D). However, only 17 out of 40 patients presented blepharitis. TheDemodexinfestation was mild in 8 patients, moderate in 19 patients,and severe in 13 patients in the keratitis group, compared tonone in 38 individuals and mild in 42 individuals in the control group (χ2=89.76,P<0.001). The keratitis was mild, moderate,and severe in 13, 19, and 8 patients, respectively. The severity ofDemodexinfestation was not correlated to the severity of keratitis (χ2=0.56,P=0.126; Table 1).
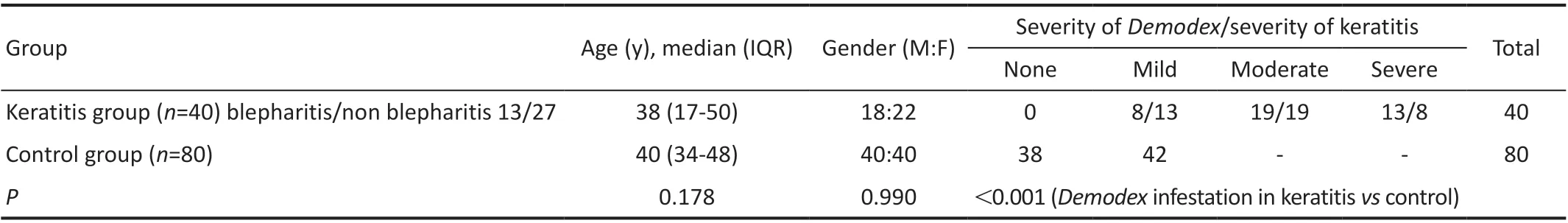
Table 1 Baseline characteristics of participants and severity of Demodex infestation and keratitis
After TTOO treatment, the incidence ofDemodexdropped from 100% (40/40) to 47.5% (19/40) in patients with refractory keratitis (χ2=28.5,P<0.01), similar to 53% in the control group(χ2=0.27,P=0.60). TheDemodexseverity demoted from severe or moderate to mild in the 19 patients.
Bacterial culture of the corneal lesion and conjunctival sac revealedStaphylococcusgrowth in nine eyes, which did not react to antibiotic eye drops. Inflammatory cells including dendritic cells (DCs) were detected at the corneal stroma in all patients by IVCM. The corneal lesions were superficial, and the thickness of the cornea at the lesion was 385±68 μm as recorded by anterior segment optical coherence tomography.After adding 5% TTOO lid scrub to the treatment, the keratitis got under control, inflammatory cells in the cornea decreased in number, typical DCs gradually became atypical, the corneal lesion resolved, and the neovascularization was absorbed in all 40 patients. Figure 1 presents the outcomes of patients with different severity levels of keratitis, showing the congestion subsided, most of the neovascularization disappeared, and the corneal infiltration was absorbed at 2wk (Figure 1A2, 1B2,1C2) and 1mo (Figure 1A3, 1B3, 1C3) after treatment. The signs and symptoms resolved within a month in all patients except for 7 patients suffering severe keratitis, the course in whom was prolonged to 2 (n=4) to 3mo (n=3). Recurrence was observed in two patients with severe keratitis during the 6mo of follow-up.
Typical CaseA 48-year-old male complained of recurrent redness and decreased vision in his left eye for 1y. He was preliminarily diagnosed with herpes simplex keratitis and treated with antiviral and antibiotic eye drops together with steroids, but the treatment was unsuccessful. Then refractory keratitis with an unknown reason was diagnosed.On examination, his visual acuity was 20/20 and 20/40 in the right and left eyes, respectively. There was no sign of blepharitis in either eye. Severe corneal lesions were present in the left eye, with neovascularization and a lot of DCs and inflammation cells in the inferior cornea (Figure 3A1, 3B1).Demodexinfestation was observed to be severe by slit lamp examination. After 3mo of lid scrubs with 5% TTOO and antiinflammatory treatment, the ranking ofDemodexinfestation reduced to none. The corneal neovascularization and DCs decreased gradually (Figure 3A2-3A4, 3B2-3B4). The livingDemodexmites of this patient before lid scrubs with TTOO were stained with calcium fluorescent white, and a beautiful outline was demonstrated under a fluorescent microscope.TheD. folliculorumlarva presented a higher fluorescent stain on the head and body, suggesting a higher level of engulfing and metabolism. The excretion process (Figure 3C) and the digestive tract morphology (Figure 3D) ofD. folliculorumwere contoured.
DISCUSSION
Nowadays,Demodex-related keratoconjunctivitis with blepharitis has become increasingly familiar to ophthalmologists.However, for patients suffering keratitis but no blepharitis,Demodexcan be ignored easily. OcularDemodexinfestation has been mostly judged with epilated eyelashes on light microscopy or IVCM[2,5-7,13], but eyelash removal is invasive and may cause pain. Moreover,Demodexmites harbor at lash follicles and sometimes do not go with the epilated lashes, which might lead to underestimated results and misdiagnosis. IVCM is usually performed by a technician and the manipulation of IVCM requires specific skills, which restricts its popularization. In our series, we performed slit lamp microscopy at high magnification (40×) to discern theDemodextail. This simple and non-invasive approach enables ophthalmologists to quickly assess theDemodexinfestation.
Regarding the judging system, we classified the severity of ocularDemodexas none, mild, moderate, and severe, instead of the averageDemodexcount, by observingDemodextails under a slit lamp. The severity ofDemodexin the control group was found to be in the range of none to mild degree,which was different from that in patients with keratitis in the range of mild to severe. AndDemodexevenly distributed bilaterally. After adding the TTOO lid scrubs to the treatment,the severity ofDemodexin the keratitis group reduced to none and mild degree accompanied with resolved symptoms and signs. Collectively, we believe that the presence of small amount ofDemodexmites is not pathogenic. When the degree is upgraded, a link with ocular surface disorders should be considered. In eyes without clear sources of chronic ocular surface inflammation, even if theDemodexinfection is mild, a mite killing therapy is still recommended.

Figure 3 Changes at the cornea after mite-killing therapy and vital staining of Demodex In a severe case, there was neovascularization in the inferior cornea (A1). IVCM showed dendritic cells and inflammation cells (B1). One month (A2, B2), two months (A3, B3), and three months(A4, B4) after the treatment, the corneal neovascularization and dendritic cells gradually diminished. The living Demodex mites stained with calcium fluorescent white presented a beautiful outline under a fluorescent microscope. The D. folliculorum larva had a higher fluorescent stain on the head and body (C, triangle), and the excretion process (C, arrow) and the digestive tract morphology (D, arrows) of D. folliculorum were contoured. IVCM: In vivo confocal microscopy.
According to the literature,Demodex-related keratopathy and other ocular surface diseases were closely related to blepharitis[12,15], presenting with inflammation at the lid margin and dandruff on the lash root, an area closest to their habitat.Therefore, the lid margin is considered to be the first and major afflicted area. A plausible mechanism for ocular demodicosis involves causing direct damage, acting as a vector for bacteria,and inducing hypersensitivity byDemodexmites[5,16-17].Despite the fact that all our patients hadDemodex, blepharitis was diagnosed in fewer than half of them. The reason thatDemodexmites caused chronic ocular surface inflammation and keratitis without typical signs at the lid margin as we observed might be the ability ofDemodexmites in digesting and absorbing part of their own debris and metabolites which resulted in little dandruff. Although theseDemodexmites do not cause visible inflammation at the lid margin, the metabolic debris can constantly discharge to the ocular surface, leading to ocular surface inflammation. In this study, most of the corneal lesions progressed slowly, and the inflammation presented a chronic course, which were presumed to be associated with the relatively weak pathogenicity and the long procedure of the immune response triggered by ocularDemodex.
Our patients with keratitis were administered with antibiotics,antivirals, anti-inflammatory and immunosuppressive ophthalmic agents, but the condition was uncontrolled or aggravated, until the intervention of eyelid scrub with 5%TTOO. We had once developed a strategy of weekly office lid scrubs with 50% tea tree oil solution to achieve a marked reduction ofDemodexcounts[14,18]. In the current study,domestic lid massage with 5% TTOO twice per day was introduced. Better tolerance and compliance were obtained, the symptoms and signs of keratitis were effectively controlled,andDemodexinfestation was demoted. Although the killing effect of 5% TTOO is much weaker than 50% tea tree oil[18],it can weaken theDemodexvitality. Furthermore, leaving 5%TTOO on the lid skin overnight might prevent copulation that takes place at the lash follicle orifice at night and achieve a favorable therapeutic result. We believe the subsidence of inflammation and neovascularization in patients with keratitis was mainly due to the demodecocide effect of the tea tree oil, together with the aid of anti-inflammatory eye drops that had been used but had not worked well. Despite the optimistic results, recurrence was observed in two patients,which is consistent with a previous report[18], and this might be attributed to the reflourishing ectoparasites.
In our study, bacterial culture of the corneal lesion and conjunctival sac revealed staphylococcus growth in nine patients. All 40 patients had been given antibiotic eye drops but the effect was not favorable, and they all had a prolonged course and relatively superficial lesions that can be seldom seen in bacterial keratitis. Hence, we did not attribute these keratitis cases to bacterial infection. Normally, a persistent course happens in viral keratitis. However, our patients did not respond to antiviral and steroid eye drops, demonstrating a loose link to viral infection.
In most cases, infectious keratitis occurs monocularly[19-21].Nevertheless, five of 40 patients developed bilateral keratitis in our study. It might be due to the fact that ocularDemodexhappens bilaterally and is similarly distributed. As for why not all patients developed binocular corneal infection, we speculate it is associated with the asymmetrical ocular surface conditions and patients’ personal habits such as sleeping posture and eye rubbing.
Demodexmites are full of granules unevenly distributed inside the body as shown under a slit lamp microscope[22].But little has been known about their internal structure under a light microscope. We used calcofluor white staining,which was reported for rapid detection of yeasts, fungi, and parasites, to observe the livingDemodexmite, a non-specific fluorescent chromophore that binds to chitin and cellulose on the cell wall[23]. Interestingly,Demodexdisplayed a beautiful contour under the fluorescent microscope. Its digestive tract morphology and excretion process were also outlined.Calcofluor white staining seems to be a promising research tool forDemodex-related diseases.
There were limitations in this series. We did not perform tear break-up time measurement, Schirmer tests, and meibomian gland infrared imaging in the study, considering that the breakup time could not be accurately measured with an uneven ocular surface in keratitis, the reflective tear secretion caused by keratitis may lead to great variability, and there would be obvious discomfort in the diseased eye. The examination approach toDemodexin our study was somewhat subjective,and a high resolution slit lamp was required. Moreover, the definition of refractory keratitis need be further specified,and the etiology need be ruled out with more evidence before addressing its relationship withDemodex. It is also necessary to verify the inspiring results in this study with more specific tests and a larger sample size.
In conclusion, ocularDemodexneeds to be checked and treated in refractory keratitis patients with or without blepharitis.DistinguishingDemodexmites under a slit lamp at high magnification (40×) is beneficial in assessing the prevalence and pathogenic role ofDemodexif keratitis is refractory with an unclear cause.
ACKNOWLEDGEMENTS
The authors thank Ping Lin for her linguistic and editorial assistance and Su Liu for his statistical assistance.
Authors’ contribution:Study concept and design by Gao YY and Shi WY. Data collection by Jiang YT, Yang MJ, Lu XH,Zheng L, and Wang ST. Analysis or interpretation of data by Gao YY, Wang T, and Shi WY. Drafting and critical revision by Gao YY and Shi WY. Funding obtained by Shi WY and Wang T.
Foundations:Supported by the National Natural Science Foundation of China (No.82271052; No.82271058;No.U20A20386); the Taishan Scholar Program (No.tspd20150215; No.tsqn201909188).
Conflicts of Interest:Gao YY,None;Wang T,None;Jiang YT,None;Yang MJ,None;Lu XH,None;Zheng L,None;Wang ST,None;Shi WY,None.
 International Journal of Ophthalmology2023年2期
International Journal of Ophthalmology2023年2期
- International Journal of Ophthalmology的其它文章
- Perspectives and clinical practices of optometrists in Saudi Arabia concerning myopia in children
- Progression of myopia among undergraduate students in central China
- Flipped classroom approach to global outreach: crosscultural teaching of horizontal strabismus to Chinese ophthalmology residents
- Topical ketotifen treatment for allergic conjunctivitis: a systematic review and Meta-analysis
- Pseudomembranous conjunctivitis in a patient with DRESS syndrome
- Two cases of persistent shallow anterior chamber after cataract surgery combined with goniosynechialysis
