Symptoms and comorbidities associated with abnormal levels of serum calcium, magnesium, and phosphate in the emergency department: a prospective observational study
Korsin Laohavisudhi, Phichayut Phinyo, Borwon Wittayachamnankul, Boriboon Chenthanakij, Theerapon Tangsuwanaruk, Parinya Tianwibool, Pavita Laohakul, Wachira Wongtanasarasin,4
1 Department of Emergency Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai 50200, Thailand
2 Department of Family Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai 50200, Thailand
3 Center for Clinical Epidemiology and Clinical Statistics, Faculty of Medicine, Chiang Mai University, Chiang Mai 50200, Thailand
4 Department of Emergency Medicine, University of California Davis School of Medicine, Sacramento, California 95817, USA
Emergency departments (EDs) play a significant role in hospital healthcare systems.[1]According to the US Centers for Disease Control and Prevention, 130 million individuals visited the ED in 2018.[2]A previous study has demonstrated that unnecessary laboratory tests did not change the management plan.[3]These actions led to ED overcrowding, causing consequences to patient outcomes.
Serum calcium (Ca2+), magnesium (Mg2+), and phosphate (PO42-) are frequently tested in EDs.[4,5]However, these tests are often found to be within normal limits and do not significantly affect decision-making.[5]The efficacy and cost-effectiveness of these serum electrolyte tests have been questioned in the previous literature.[4]One study observed abnormal results of Ca2+, Mg2+, and PO42-levels in patients with some clinical and risk variables, such as seizure, palpitation, vomiting, etc.[6]The laboratory tests were sent more than usual, especially in EDs.[5]Thus, this study aims to investigate symptoms and comorbidities associated with abnormal Ca2+, Mg2+, and PO42-levels and treatments given.
METHODS
We conducted a prospective cohort study on adult patients (≥18 years) who visited the ED of a tertiary university hospital between August and November 2020. This study was prepared and reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.[7]Patients were included if at least one of the following tests was ordered: serum Ca2+, Mg2+, and PO42-, and reported during their ED stays. Patients with traumatic complaints were excluded since the tests might be sent per specific protocols or preoperative assessments.
We gathered information on age, sex, specific signs and symptoms, comorbidities, laboratory results, and treatments given to patients. Symptoms and comorbidities were extracted from previous literature, such as vomiting, muscle weakness, seizure, and chronic kidney disease. The primary outcome was the diagnostic performance of symptoms and comorbidities associated with abnormal Ca2+, Mg2+, and PO42-levels and treatments that had been given.
According to a previous study, we calculated a sample size of 474 patients based on a finite population correction and a two-percent margin of error. Laboratory data were divided into abnormal and normal levels according to our laboratory reference ranges. We used STATA16 to perform all statistical analyses. Means with standard deviations or medians with interquartile ranges were used based on the data distribution. Positive predictive values (PPVs), negative predictive values (NPVs), positive likelihood ratios (PLRs), and negative likelihood ratios (NLRs) of abnormal levels of Ca2+, Mg2+, and PO42-associated with the treatments given were calculated, with 95% confidence intervals (CIs). We performed comparative analyses using the Chi-square test or Fisher’s exact test for categorical variables and Wilcoxon rank-sum test for continuous variables. AP-value of less than 0.05 was considered statistically significant.
RESULTS
During the study period, 11,498 adults presented to the ED. Of these, Ca2+, Mg2+, or PO42-tests were requested for 673 (11.6%) patients, and 598 (10.3%) tests were reported before they left the ED. The patients’ mean age was 62 years, and 288 (48.2%) patients were men. Four hundred fifteen patients were tested for serum albumin levels to determine corrected Ca2+levels. The serum Ca2+level was 8.9±1.0 mg/dL, with a corrected serum Ca2+level of 9.2±1.0 mg/dL. The serum Mg2+level was 1.7±0.3 mg/dL, and the serum PO42-level was 3.3±1.4 mg/dL. Thirty-two percent of all corrected tests were abnormal. Most of these abnormalities were hypophosphatemia (20.8%). The study fl ow chart and descriptive characteristics of the included patients are summarized in supplementary Figure 1 and supplementary Table 1.
Table 1 demonstrates the PLR, NLR, PPV, and NPV of symptoms and comorbidities for abnormal Ca2+, Mg2+, and PO42-levels and treatments given. Overall, patients without any symptoms of abnormal Ca2+, Mg2+, and PO42-levels rarely received treatments for these tests (NPVs for Ca2+, Mg2+, and PO42-were 100%, 95%CI97.6%-100%, 93.9%, 95%CI90.6%-96.4%, and 99.7%, 95%CI98.2%-100%, respectively). Noticeably, only abnormal Ca2+patients with at least one symptom significantly received treatments compared to those without (PLR 1.6, 95%CI1.5-1.8).
Symptoms associated with abnormal corrected Ca2+levels were fatigue (P=0.03). Symptoms and comorbidities associated with abnormal levels leading to the treatments were handfoot spasms, fatigue, hypoparathyroidism, and malignancy (P=0.001, 0.003, 0.03, and 0.05, respectively). The probability of getting treated (either hypocalcemia or hypercalcemia) differed significantly between those with at least one symptom and those without (5.0% vs. 0,P=0.003). Symptoms and comorbidities associated with abnormal Mg2+levels were nausea, hand and foot spasm, chronic liver disease, and alcohol use (P=0.02, 0.10, 0.005, and 0.02, respectively). Symptoms and comorbidities associated with abnormal PO42-levels were nausea and alcohol use (bothP=0.02). The details of symptoms and comorbidities associated with these abnormalities and treatments are shown in supplementary Tables 2-4.
DISCUSSION
In this study, patients with at least one symptom of abnormal Ca2+levels had a higher chance that treatments had been given than those without. Interestingly, up to 26% of the study population without symptoms had abnormal Ca2+levels. However, none of the patients were treated for laboratory abnormalities at the ED. Approximately 10% of the study patients were sent at least one of these tests in the ED.
Abnormal Ca2+, Mg2+, and PO42-levels varied noticeably (18.5%, 15.2%, and 29.5%, respectively, supplementary Table 1). For abnormal serum Ca2+levels, only 12 (2.9%) out of 415 patients had extremely abnormal levels (<7.0 mg/dL or >14.0 mg/dL). Our study shows that fatigue was the only symptom associated with abnormal Ca2+levels. Additionally, fatigue, hand and foot spasm, hypoparathyroidism, and malignancy were associated with abnormal levels that had been treated. These findings support the evidence that only a small proportion of patients with abnormal Ca2+levels received treatments. Conforming with a previous study, it is demonstrated that the rate of detecting clinically significant abnormal levels is very low, and patient management is rarely changed.[5]The details of patients to whom treatments were given for their abnormal Ca2+levels are described in supplementary Table 5.
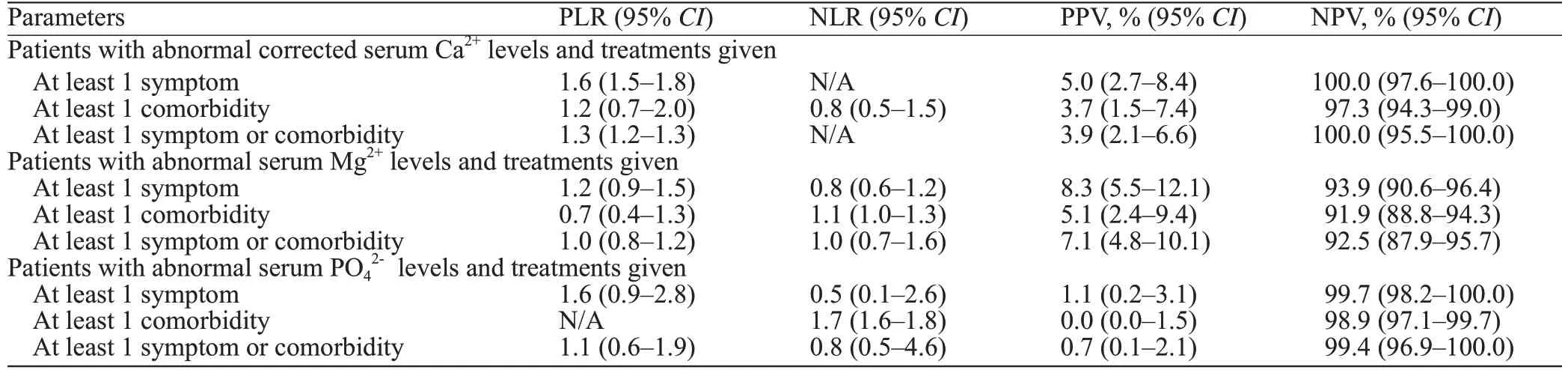
Table 1. The PLR, NLR, PPV, and NPV of symptoms and comorbidities for abnormal Ca2+, Mg2+, and PO42- levels and treatments given
Furthermore, alcohol intake was associated with abnormal Mg2+levels and the treatments given (P=0.02 andP=0.05, respectively). It has been reported that heavy alcohol drinking was linked to lower Mg2+levels.[8]Alcohol would explain this as an acute Mg2+diuretic, resulting in a rapid and vigorous increase in urinary excretion and certain other electrolytes.[8]Abnormal serum Mg2+levels were mostly treated as an electrolyte abnormality (7.2%). The reason for this finding may be that Mg2+was often prescribed to patients with normal Mg2+levels. Patients with cardiac arrhythmias, such as atrial fibrillation (AF) or atrial fl utter, benefit from a high-normal level of Mg2+. Moreover, there is evidence concerning the effectiveness of Mg2+in AF treatment in the ED.[9]Medical management was infrequently changed despite serum PO42-levels beingmore commonly abnormal than Ca2+and Mg2+. However, the association between serum PO42-levels and management outcomes in the ED was inconsistent. A previous study reported that the treatment is unnecessary unless the PO42-levels are extremely low.[10]
Based on our findings, targeting specific electrolyte abnormalities resulted in very few treatments. Since our study’s testing rate was higher than expected, it will be crucial to initiate proper clinical guidelines for better managing patients most at risk for abnormal levels. Furthermore, it would be more purposeful to conduct before and after the study after implementing a protocol to see if unnecessary tests can be reduced. The most common risk factors for abnormal levels are fatigue, nausea, chronic liver disease, and alcohol use. For treated abnormalities, the risk factors are hand and foot spasms, fatigue, hypoparathyroidism, malignancy, alcohol use, and muscle weakness. Further interventions are warranted to reduce inappropriate Ca2+, Mg2+, and PO42-testing in the ED. Several studies have documented some clinical variables associated with the benefit of ordering these labs in the ED.[4,11,12]ED personnel should be encouraged to order the tests individually as indicated according to the patient’s symptoms and comorbidities.
This study had some limitations. First, this study’s findings came from only a single-center setting and might not be applicable in other EDs. Second, this study was conducted relatively short, which may affect the results since the frequency of several diseases varies depending on the seasons. Third, the definition of abnormal electrolyte levels was retrieved from our laboratory reference. Small abnormal levels outside the range are not truly aberrant and are unlikely to significantly affect patient management. Furthermore, some clinical risks mentioned in this study were barely detected. The number of patients experiencing perioral numbness, hand and foot spasm, hyperparathyroidism, and hypoparathyroidism was less than 10. Finally, we have yet to obtain the true changes in patient management in this study. We only collected data on treatments given for those abnormal laboratory levels.
CONCLUSION
Approximately ten percent of the study population was tested for at least one of the three tests. We suggest that clinicians request serum Ca2+, Mg2+, and PO42-only for patients with potential symptoms and comorbidities (fatigue, nausea, chronic liver disease, and alcohol use) to reduce unnecessary costs and overcrowding situations in the ED. Moreover, a future study on the impact of these management changes is warranted.
Funding:None.
Ethical approval:This study was approved by the Institutional Review Board (IRB) of the Faculty of Medicine, Chiang Mai University (Exemption 7418/63).
Confl icts of interest:None declared.
Contributors:KL, PP, BW, BC, TT, PT, PL, and WW designed and coordinated the study. KL, BW, and WW participated in IRB proposal submission and data collection. KL verified the data. KL, PP, and WW performed statistical analysis and table and figure design. BW and BC supervised the study process. KL and WW drafted the initial manuscript. WW critically revised the manuscript. All authors reviewed and approved the final version.
All the supplementary files in this paper are available at http://wjem.com.cn.
 World journal of emergency medicine2023年1期
World journal of emergency medicine2023年1期
- World journal of emergency medicine的其它文章
- Patient care during interfacility transport: a narrative review of managing diverse disease states
- Endothelial cell metabolism in sepsis
- Nutritional status and prognostic factors for mortality in patients admitted to emergency department observation units: a national multi-center study in China
- Prolonged dual antiplatelet therapy after drug-eluting stent implantation improves long-term prognosis for acute coronary syndrome: five-year results from a large cohort study
- Efficacy and safety of remimazolam-based sedation for intensive care unit patients undergoing upper gastrointestinal endoscopy: a cohort study
- Glutamine supplementation attenuates intestinal apoptosis by inducing heat shock protein 70 in heatstroke rats
