Patient care during interfacility transport: a narrative review of managing diverse disease states
Quincy K. Tran, Francis O’Connell, Andrew Hakopian, Marwa SH Abrahim, Kamilla Beisenova, Ali Pourmand
1 Department of Emergency Medicine, University of Maryland School of Medicine, Baltimore 21201, USA
2 Program in Trauma, the R Adams Cowley Shock Trauma Center, University of Maryland School of Medicine, Baltimore 21201, USA
3 Department of Emergency Medicine, George Washington University School of Medicine and Health Sciences, Washington DC 20037, USA
KEYWORDS: Critically ill patients; Interfacility transfer; Interhospital transfer; Extracorporeal membrane oxygenation; Obstetric emergencies; Hypertensive emergencies
INTRODUCTION
The transfer of critically ill patients between hospitals (interfacility transfer) involves getting patients to the appropriate level of care in the most efficient amount of time. Interfacility transfers often occur when the patient’s care requires specialized treatment or resources that exceed the capability of the hospital to which the patient first presents. Interfacility transports of critical patients often demand rigorous resources and intensive driving mileage,[1]and ensure the safe transport of patients from one facility to another.[2]
Recent studies have focused on the safety and necessity of critical interfacility transfers, essential equipment needed, and the possibility of adverse events, including the causes and frequency of their occurrence.[3-5]However, these studies did not provide specific recommendations for the best practices for potential issues during the interfacility transfer process. Common technical difficulties included restricted space, low-light conditions, loud noise, and equipment malfunctions.[6,7]Medical adverse events during interfacility transport include procedural errors, drug errors, and loss of intravenous (IV) access. Furthermore, patients experienced life-threatening events from bradycardia, hypotension, and cardiac arrest.[6,7]Difficulties with cardiac monitoring and electrocardiograms were also observed, indicating that cardiac events may go unnoticed during transport due to monitoring methods as well as the mechanics of transport.[8]Consequently, proposed solutions to decrease the risk of complications included improving monitoring capabilities and using specialized transport teams.[6]
With evolving advancements in stabilizing and treating critically ill patients and increased use of interfacility transport services, there is a need for evidence-based guidelines for transporting patients to ensure the best possible treatment enroute.[9]The purpose of this paper is to review available evidence-based practices for the safest and most efficient interfacility transfer of critically ill patients.
METHODS
For this literature review, we searched the PubMed, Cumulative Index of Nursing and Allied Health (CINAHL), and Scopus databases to assess literature on “interfacility transport” as it relates to patients with emergent/critical medical conditions. The terms “transport”, “transfer”, “interfacility”, and “emergency” were used. Boolean operators and medical subject headings (MeSH) terms were used to combine search terms. Search results were further limited to English language, human, and adult. The result revealed 75 matches. Database searches were supplemented by screening the reference lists of relevant studies and reviews, but we did not contact any corresponding authors for more information. This resulted in more eligible articles for inclusion. In total, 48 studies were included in the analysis.
Two reviewers independently screened titles and abstracts using the following criteria: Adult patients who had emergency department (ED)-to-ED transfer in critical condition were included. Articles were not included if they were not primarily in English or did not have an English translation, were focused on pediatric patients or were preliminary/unpublished results. Any discrepancies were resolved by discussion among the investigators. Additionally, we excluded articles not involving critically ill adult patients or articles not relating to urgent and/or emergent medical conditions.
RESULTS
Respiratory failure and prone positioning
Acute respiratory distress syndrome (ARDS) is a common condition associated with critical illnesses, which causes substantial mortalities.[10]Placing patients in the prone position improves oxygenation and reduces mortality in ARDS patients.[11]As the prone position becomes a more common practice for patients with hypoxic respiratory failure, new challenges are arising as traditional transportation systems are designed for supine patients. The challenges for transporting teams include preparing and situating the patient for transport, loss of established airway for patients receiving invasive ventilation, and performing cardiopulmonary resuscitation (CPR) on prone-positioned patients.
Transporting patients in the prone position can be a timeconsuming affair, with on-scene time reported to be 1-3 h.[12]Patients requiring invasive mechanical ventilation need to be adequately sedated and secured to the stretcher to prevent them from shifting during transport, which can dislodge lines/tubes.[13]Patients may also require vasopressor agents such as norepinephrine during transport.[13]
Since prone positioning interferes with being able to access patients’ airways and endotracheal tubes, care must be taken to prevent dislodgement of any airway devices by supporting the head. Transport clinicians need to ensure that the intubated patient’s airway or mechanical ventilator has not been compromised, such as dislodgment or blocking of the endotracheal tube.[14]Preventive methods include the use of an anesthesia pillow or turning of the head slightly to one side and supporting it with towel rolls.[13]Although earlier reports indicated an increased risk of airway compromise in prone-positioned patients, recent literature suggests that there is no increase in accidental extubation, accidental catheter removal, endotracheal tube obstruction, barotrauma, or ventilator-associated pneumonia.[10]
In the event of a proned patient’s cardiac arrest, chest compressions can be performed with patients in the prone position. It is likely beneficial to a patient’s outcome to begin CPR immediately, rather than to supinate the patient before starting CPR. There is, however, conflicting evidence as to the method of performing chest compressions for proned patients. Compressions performed between the level of the T7-T10 vertebrae, below the inferior angle of the scapula,[14-17]were reported to be effective. However, the European Resuscitation Council (ERC) suggests performing compressions between the scapulae at the usual depth and rate.[18]Defibrillator pads can be placed either anterior-posterior or bi-axillary.[16,18]Support under the sternum may be needed to allow for proper chest compression. After initiating CPR, there may be a need to supinate the patient. The American Heart Association (AHA) recommendation for prone-positioned patients without an advanced airway is to supinate the patient and resume CPR; in the case of a prone-positioned patient with an advanced airway, it is recommended to continue CPR in the prone position to prevent dislodging the airway.[17]Another recommendation by the ERC is to continue prone CPR until supination is needed for an intervention, e.g., airway complications, or when chest compressions are ineffective and spontaneous circulation is not restored rapidly within minutes ( supplementary Figure 1).[18]
Recommendation for personnel:transport clinicians with advanced cardiac life support (ACLS) experienced with difficult airways.
Recommendation for equipment:cardiac monitoring, advanced airway equipment, advanced sedative, paralytic medications, and portable ventilator.
Aortic dissection and blood pressure management
Acute aortic dissection (AAD) is an emergent lifethreatening condition with a high mortality rate. As urgent surgical care is often the definitive treatment for patients with type A AAD, patients receiving care at hospitals with a high volume of aortic surgeries are associated with improved outcomes and should be strongly considered.[19]Interfacility transfer is not associated with a change in operative mortality, although patients transferred from low-volume facilities to high-volume centers experienced delays in receiving surgery. Transferring patients from a low-volume facility to a high-volume hospital is associated with a 7.2% absolute risk reduction in operative mortality.[19]Nonetheless, transport by air is not associated with faster time to surgical intervention[20]or better outcome.[21]Therefore, the type of transfer that provides the most effective transport for patients with AAD should be considered.
The 2010 AHA guidelines call for a desired systolic blood pressure (SBP) range 100-120 mmHg (1 mmHg=0.133 kPa) and a heart rate less than 60 beats/min for patients with acute dissection.[22]Patients undergoing interfacility transfer for suspected acute aortic dissection (SAAD) have heart rates exceeding 80 beats/min in 41.9% of cases and an SBP exceeding 120 mmHg in 67.7% of cases by the time the medical transport team arrived at the referral facility.[23]Poor blood pressure management prior to transfer can lead to delays in medical transport of SAAD and AAD and may lead to worsening outcomes. Patients with SAAD and invasive arterial blood pressure (IABP) monitoring undergo more aggressive hemodynamic management with a higher frequency of meeting hemodynamic goals upon arrival at the accepting facility.[24]The same study reports that invasive arterial cannulation by transport clinicians increases bedside care by 6 min,[24]thus supporting the placement of IABP catheters at the referring facility prior to transport.
Recommendation for personnel:clinicians with knowledge about AHA’s guidelines, experience with pharmacokinetics of common anti-hypertensive agents such as esmolol, nicardipine, clevidipine. Transport personnel may be trained on how to insert arterial line catheters and how to set up arterial blood pressure monitoring.
Recommendation for equipment and drugs:cardiac monitoring, arterial blood pressure monitoring; desired choice of antihypertensive agents based on the destination facility protocol.
Extracorporeal membrane oxygenation (ECMO)
ECMO is a treatment typically reserved for patients with severe respiratory or circulatory compromise. While transport of patients on ECMO has been studied for some time, challenges exist in the interfacility transfer of ECMO patients. One of the biggest hurdles is the preparation of an ECMO patient for transport. Transport teams need to be experienced in critical care transport in addition to having ECMO-specific training. Teams consisting of a critical care transport nurse, a paramedic, and an ECMO specialist (perfusionist, specially trained nurse, or respiratory therapist) are sufficient and are associated with similar patient outcomes when compared to teams without a physician, nurse practitioner, or physician assistant.[25]
Complications during transport of ECMO patients occur between 28% and 40% of transports. The majority (62%-65%) of patient-related complications include loss of tidal volume, hypovolemia, and circulatory instability, which can be associated with failures or limitations of medical equipment or issues associated with air transport. Transport via aircraft can cause complications due to forces associated with aircraft acceleration and deceleration and the changes in atmospheric pressure at altitude, which can create vibrations and dislodgement of tubes and lines.[26]Additional largebore venous access should be established for immediate fl uid resuscitation before transport, and infusions of vasoactive drugs must be immediately available if hypovolemia occurs.[27]
Recommendation for personnel:a perfusionist, a critical care transport nurse who is familiar with ECMO clinical scenarios and ventilator management, and a respiratory therapist recommended but not mandatory.
Recommendation for equipment:a backup ECMO circuit, ventilator, cardiac equipment. A point-of-care system for arterial blood gas analysis is also recommended.
Intracranial hemorrhage
Acute intracranial hemorrhages (either spontaneous or traumatic) require transfer to a facility with neurosurgical and neurocritical care for both diagnostic and therapeutic reasons.[28]Advanced monitoring, clinical experience, 24-hour magnetic resonance imaging (MRI) availability, and neurosurgical backup are necessary resources in managing patients with intracranial hemorrhages. Transporting patients with moderate to severe traumatic brain injury (TBI) (Glasgow Come Scale [GCS] <12) to a trauma center is well supported.[29-31]Admission of spontaneous intracranial hemorrhage (sICH) patients to a neurologic ICU is associated with reduced mortality rates.[32]Referring medical centers should thoroughly evaluate the patient prior to transfer as the ideal service at the accepting facility (neurology, neurosurgery, etc.) is determined prior to the transfer of the patient to ensure a quick and smooth transfer of care.[29]
sICH accounts for 20% of strokes and is typically associated with an aneurysmal rupture.[33]A third of patients with sICH demonstrate acute neurological deteriorations (ND) with factors such as blood pressure variability (BPV) contributing to outcomes. Transfer of patients with TBI with CT findings of hemorrhage to a Level I (the highest level) or II trauma center is associated with survival benefits.[34]Transferring facilities need to monitor the maximum systolic blood pressure (SBPmax), as 75% of patients with an SBPmax> 240 mmHg develop ND.[32]Prolonged and severe hypertension can contribute to growing intracranial pressure (ICP), increase the risk of sICH, and worsen existing sICH. For this reason, the current guidelines from the American Stroke Association (ASA)[35]state that the SBP of patients with sICH should be reduced to 160 mmHg or less. Another important variable includes the difference between the highest and the lowest SBP (SBPmax-min) and patient age. An external ventricular drain, if neurosurgical resources are available, may be placed at the first facility to continuously monitor ICP or divert cerebrospinal fl uid (CSF).
The main interventions initiated by the transport team for patients with ICH are pharmacotherapy and ventilator management. The most common medication administration includes sedative management (27%), followed by antihypertensive medication management (26%).[36]Patients received antiepileptics (P=0.030) and hyperosmolar therapy (P=0.031), with a significantly greater number of ND patients receiving interventions.[32]For the transport crew, the medical control (MC) physician determines the number and type of monitoring devices, such as ICP monitors, and the need for additional staff (i.e., second paramedic, nurse, or physician). ICP monitors need to be observed during the whole transport time to avoid dislodgement of the catheter. If dislodgement occurs, sterile dressing must be applied as CSF may leak from the site. A large-bore IV catheter should be established for fl uids to maintain a minimum blood pressure or medications such as mannitol to reduce cerebral edema with increased ICP. Steps such as pre-transport checklists should be taken to avoid mistakes such as mannitol dosing errors.[37]
Recommendation for personnel:transport critical care nurses who are familiar with AHA/ASA guidelines for target blood pressure, pharmacokinetics of commonly used antihypertensive agents for these patients (nicardipine, clevidipine), ICP management, ventilator management in cases of increased ICP.
Recommendation for equipment:cardiac monitoring with the capability to measure cuff pressure every 2-3 min. Arterial blood pressure monitoring is optional but not mandatory.
Uncontrolled vaginal/uterine hemorrhage
While most ED visits for vaginal bleeding are managed at their respective facilities, there are situations where vaginal bleeding requires transfer. As an example, there are instances where menorrhagia can result in symptomatic anemia.[38]Serious bleeding can occur as a result of anatomical disruptions (polyps, fibroids), systemic hematological/oncological or endocrine etiologies, or trauma.[39]Severe uterine or vaginal bleeding may also occur post-partum in circumstances of multiple gestations, multiparity, prior history of post-partum bleeding, prolonged labor, and medications that can cause bleeding.[38]
The primary steps in managing vaginal hemorrhage are to identify the etiology, achieve source control and effect stabilization, and in cases where that cannot be done effectively at the local ED, initiate transport. This generally includes an external and internal (speculum) exam to better identify and address the source of bleeding. Symptomatic patients should also receive a transfusion of red blood cells or other necessary blood products.[38]With menorrhagia, if there is heavy bleeding and the cause is unknown, the focus of the treatment should look to reduce the amount of blood loss. This can be achieved through the use of non-steroidal anti-inflammatory drugs, oral tranexamic acid, combined or progesterone oral contraceptive pills, or a progesteroneeluting intrauterine device.[39]Transport teams should be ready to manage simultaneous administration of blood products and medications, and the receiving facility should have an interprofessional team ready for the patient’s arrival.
Recommendation for personnel:transport critical care nurses or paramedics with knowledge of blood products, blood transfusion, allergic reaction to blood products. Transport clinicians familiar with managing shock is strongly recommended. Knowledge about tamponade devices is optional but not mandatory.
Obstetric emergencies
Interfacility transport of obstetric emergencies presents significant challenges due to the numerous changes, both anatomically and physically, of pregnant patients. Other complications may include trauma, with 6% to 7% of all pregnancies having trauma complications.[40]Transporting a pregnant patient is often more beneficial than transporting the postpartum mother and neonate from the referring facility. Neonates who are transferred post-delivery are associated with higher rates of complications and greater morbidities when compared with those who were transferred antenatally.[41]As a result of the difficulties in the management of pregnant patients, transport to a higher level of care should be considered in a willing, stable patient where impending delivery is not expected during transport, and the benefits of transport outweigh the risks.[41-43]
High-risk obstetric patients had a lower risk of maternal morbidity when treated at high-acuity centers compared to low-acuity centers.[44]Hospitals with the number of highrisk deliveries comprising >7.1% of their total number of deliveries were considered high-acuity centers. Using an established comorbidity index, high-risk conditions had a weight ≥3. High-risk conditions included severe preeclampsia/eclampsia (weight 5), chronic congestive heart failure (weight 5), congenital heart disease (weight 4), pulmonary hypertension (weight 4), and age >44 (weight 3).[44]Another study reported that transfer to a higher level of care may improve the outcome or change the course for 11% of all pregnancy-related deaths recorded in the study, with recommendations that maternal transport protocols should include earlier transfer to a higher level of care.[45]
Ground transport is the preferred method for obstetric transport due to more direct hospital-to-hospital transfer, a larger area to work in an ambulance, greater availability in number and utility in all weather conditions, and incidentally, lower cost.[43]Air transport is preferred over ground transport when long distances increase transport time. Transport personnel should be advanced life support (ALS) capable, including ACLS, IV cannulation, endotracheal intubation, neonatal evaluation and resuscitation skills.[43]They should be trained in obstetric and neonatal emergencies and be able to perform skills including interpretation of fetal monitors, performance of vaginal delivery, and administration of obstetric drugs such as tocolytics, anti-hypertensive agents, hemostatic agents, and magnesium sulfate.[41,46]
The frequency of adverse events in pregnant patients during both air (8.1%) and ground (4.8%) transport is relatively low. Exacerbation of hypertensive conditions is the most common adverse event, occurring in 4.5% of all transports.[47]Other adverse events included hypotension (1.3% of transports), altered mental status (0.2%), and dysrhythmia (0.1%); no other adverse events were reported for either air or ground transfers (n=1,101).[47]All hypotensive episodes were resolved with an IV fluid bolus. One study found that the rate of deliveries during the transport of obstetric patients, even those in advanced labor and fully dilated, was zero.[41]Another study found that the likelihood of delivery during interfacility transport is low, although screening patients for a high probability of delivery during transport is an important factor.[47]It is possible to transport obstetric patients in advanced labor if all factors, such as transport time and transport personnel skill, are considered and deemed acceptable by the care teams.[41]However, it is still recommended to delay transport if delivery is anticipated to occur during transport.[43]
Maternal and fetal monitoring and intervention are crucial in effecting an optimal transport. Fetal heart rate monitoring is recommended for the transport of critical obstetric patients, including trauma patients ≥23 weeks’ gestation, preterm labor, hemorrhage, sepsis, preeclampsia and eclampsia.[41,43,46,48]Continuous fetal heart rate monitoring is the preferred method; if continuous fetal monitoring is unavailable, fetal heart rate auscultation at least every 15 min can be sufficient.[41,43]Placing the patient in the left lateral position will avoid episodes of reduced cardiac output, hypotension and episodes of hypoperfusion.[41,43,46,48,49]In the case of obstetric trauma, the severity of maternal injuries and gestational age should be considered; interventions for maternal health should take priority over interventions for the fetus.[41,49]When major injuries are present, the patient should be transferred to a trauma center or ED regardless of the gestational age of the fetus. Ideally, the trauma obstetric patients should be transferred to a Level I trauma center combined with obstetrics capabilities. If there are no life- or limb-threatening injuries and the fetus is viable (>23 weeks’ gestation), the mother should be transported to a maternity facility; if the fetus is considered non-viable (and/or <23 weeks’ gestation), then the mother can be transferred to an ED instead.[49]
Although delivery should be delayed for transport, if delivery becomes imminent during transport, then preparation for necessary equipment such as an obstetric delivery kit is necessary. Providers should prepare for neonatal resuscitation and administration of oxytocin to reduce postpartum bleeding.[43]In the case of cardiac arrest during transport, transport teams should focus on maternal resuscitation. High-quality CPR should be initiated with left lateral uterine displacement, prioritization of airway management and oxygenation, and termination of fetal monitoring.[50]Transport should be to a facility with the capability to immediately perform perimortem cesarean delivery while continuing resuscitation.[50]
Recommendation for personnel:Transport clinicians are required to perform vaginal delivery, be familiar with the pharmacokinetics and adverse events of magnesium sulfate, tocolytics, and anti-hypertensive agents (labetalol and nicardipine), and be skilled in adult and neonatal airway management. The ability to interpret fetal monitoring tracing is strongly recommended.
Recommendations for equipment:Cardiac monitoring, neonatal airway equipment, obstetric delivery kit, and fetal monitoring are strongly recommended.
DISCUSSION
Interfacility transfer is an essential part of the spectrum of patient care. Although numerous studies evaluated the safety and necessity of these transfers, they did not provide specific guidelines for the best practices during the interfacility process. With technological advancements and the increased use of interfacility transport services, it is vital to establish evidence-based transport guidelines.[9]The transfer process can be lifesaving tools that connect the patient to services and treatments not available at their current facility. The higher risk transfers include respiratory failure requiring prone positioning, aortic dissection, ECMO, intracranial hemorrhage, uncontrolled uterine/vaginal hemorrhage, and obstetrics (Table 1). Interfacility transport does not come without complications. These complications can be divided into four categories: pulmonary/airway, cardiovascular, infectious, and endocrine.[51]Airway complications may include desaturation, pneumothorax, lung collapse, or accidental extubation leading to airway loss.[52]Important transport precautions to target these issues should include a full oxygen tank, appropriate sedation of the patient, confirmation of proper endotracheal tube placement, and a working pulse oximeter. Cardiovascular complications include tachycardia, hypotension or hypertension, arrythmias, and cardiac arrests. It is vital to have appropriate cardiac monitoring as well as hemodynamic monitoring tools and the equipment required to perform resuscitation in cases of cardiac arrest.[53]Infectious complications may arise both to a transported patient with improper use of sterile equipment and to the providers taking care of a patient who may have a transferable disease.[51]This is best avoided with attention to equipment and supplies used in the patient’s care and good communication between the transport team and the receiving team on the patient’s medical condition. Last, endocrine complications such as hypoglycemia and hyperglycemia and acid-base changes may occur during transfer due to discontinuation or altering of insulin or fluid therapy or the interruption of other vital infusions such as vasopressor or sedation medications.[51]This may be prevented by attending to infusion alterations as well as stat checks of blood glucose, blood gases, and electrolytes. By selecting appropriate transport care teams, equipment, and tools for patients in transfer, the referring facility can ensure the safest transfer of patients.
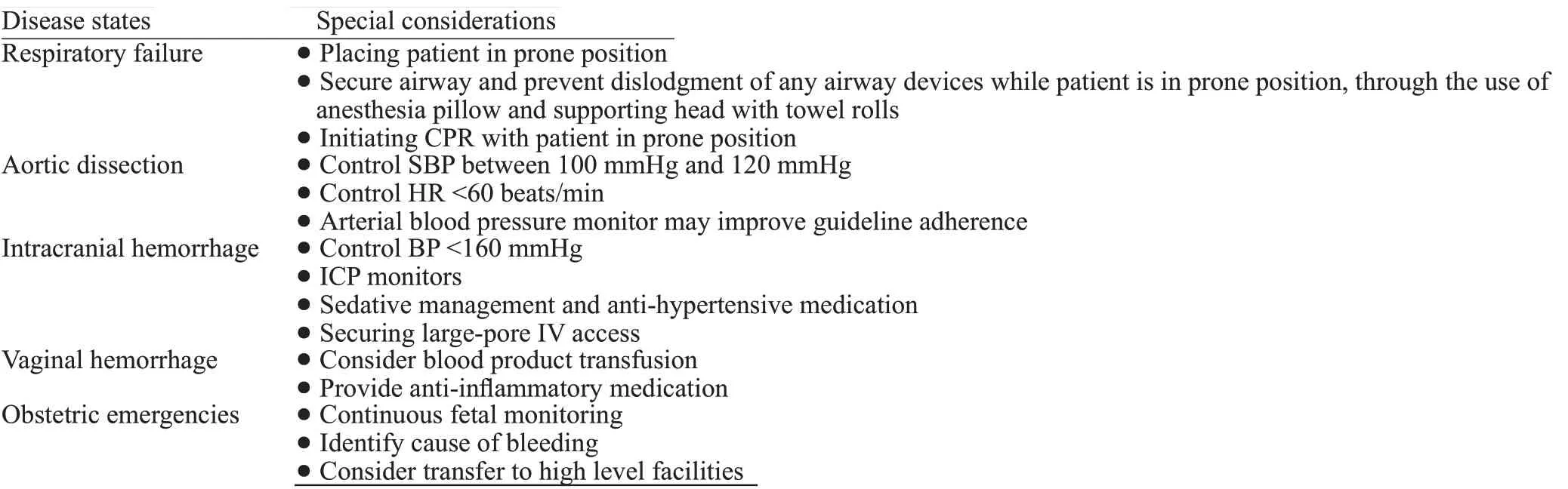
Table 1. Special consideration in critically ill patients prior to and during transportation
Funding:None.
Ethical approval:Not needed.
Conflicts of interest:The authors do not have a financial interest or relationship to disclose regarding this research project.
Contributors:QKT wrote the first draft of this paper. All authors approved the final version.
The supplementary file in this paper is available at http://wjem.com.cn.
 World journal of emergency medicine2023年1期
World journal of emergency medicine2023年1期
- World journal of emergency medicine的其它文章
- Endothelial cell metabolism in sepsis
- Nutritional status and prognostic factors for mortality in patients admitted to emergency department observation units: a national multi-center study in China
- Prolonged dual antiplatelet therapy after drug-eluting stent implantation improves long-term prognosis for acute coronary syndrome: five-year results from a large cohort study
- Efficacy and safety of remimazolam-based sedation for intensive care unit patients undergoing upper gastrointestinal endoscopy: a cohort study
- Glutamine supplementation attenuates intestinal apoptosis by inducing heat shock protein 70 in heatstroke rats
- Development and validation of a nomogram for predicting survival in patients with acute pancreatitis
