Successful outcomes of unilateral vs bilateral pedicle screw fixation for lumbar interbody fusion: A meta-analysis with evidence grading
Lei Sun, Ai-Xian Tian, Jian-Xiong Ma, Xin-Long Ma
Lei Sun, Ai-Xian Tian, Jian-Xiong Ma, Xin-Long Ma, Orthopedic Research Institute, Tianjin Hospital, Tianjin University, Tianjin 300050, China
Abstract BACKGROUND Whether it’s better to adopt unilateral pedicle screw (UPS) fixation or to use bilateral pedicle screw (BPS) one for lumbar degenerative diseases is still controversially undetermined.AIM To make a comparison between UPS and BPS fixation as to how they work efficaciously and safely in patients suffering from lumbar degenerative diseases.METHODS We have searched a lot in the databases through 2020 with index terms such as “unilateral pedicle screw fixation” and “bilateral pedicle screw fixation.” Only randomized controlled trials and some prospective cohort studies could be found, yielding 15 studies. The intervention was unilateral pedicle screw fixation; Primarily We’ve got outcomes of complications and fusion rates. Secondarily, we’ve achieved outcomes regarding total blood loss, operative time, as well as length of stay. Softwares were installed and utilized for subgroup analysis, analyzing forest plots, sensitivity, heterogeneity, forest plots, publication bias, and risk of bias.RESULTS Fifteen previous cases of study including 992 participants have been involved in our meta-analysis. UPS had slightly lower effects on fusion rate [relative risk (RR) = 0.949, 95%CI: 0.910 to 0.990, P = 0.015], which contributed mostly to this metaanalysis, and similar complication rates (RR = 1.140, 95%CI: 0.792 to 1.640, P = 0.481), Δ visual analog scale [standard mean difference (SMD) = 0.178, 95%CI: -0.021 to 0.378, P = 0.080], and Δ Oswestry disability index (SMD = -0.254, 95%CI: -0.820 to 0.329, P = 0.402). In contrast, an obvious difference has been observed in Δ Japanese Orthopedic Association (JOA) score (SMD = 0.305, 95%CI: 0.046 to 0.563, P = 0.021), total blood loss (SMD = -1.586, 95%CI: -2.182 to -0.990, P = 0.000), operation time (SMD = -2.831, 95%CI: -3.753 to -1.909, P = 0.000), and length of hospital stay (SMD = -0.614, 95%CI: -1.050 to -0.179, P = 0.006).CONCLUSION Bilateral fixation is more effective than unilateral fixation regarding fusion rate after lumbar interbody fusion. However, JOA, operation time, total blood loss, as well as length of stay were improved for unilateral fixation.
Key Words: Unilateral pedicle screw fixation; Bilateral pedicle screw fixation; Meta-analysis; Spinal fusion surgery; Discectomy; Lumbar interbody fusion
INTRODUCTION
Lumbar interbody fusion (LIF) or spinal fusion surgery was independently proposed by Hibbset al[1] in 1911. To date, this surgical procedure has been used to treat spinal disorders including degenerative vertebral disease, trauma, infection, and tumors for more than a century. The main procedures include discectomy, endplate preparation, bone grafting, cage insertion, pedicle screw placement, or standalone. Patient expectations and the increasing demand for shorter hospital stays have led to more innovative surgical techniques. There are five major surgical approaches: posterior LIF, anterior LIF, lateral LIF, transforaminal LIF, and oblique LIF or anterior to the psoas. The choice of surgical approach is often determined by surgeon preference and patient factors, as there has been no clear or strong evidence regarding which approach is superior[2-5]. The most common internal fixation method for fusion is posterior pedicle screw fixation, and bilateral pedicle screw (BPS) fixation is considered a standard procedure. However, excessive rigidity is suspected to result in clinically adverse effects, such as adjacent segment degeneration, device-related osteoporosis, and a higher risk of other complications[6]. While there is plenty of research exploring two pedicle screw fixations, most studies were limited by their retrospective nature, lack of a comparison group, or inadequate follow-up[7,8]. Previous metaanalyses also included the limitations of not including all prospective studies and incorporating many retrospective studies, and the results may be biased[8,9]. We retrieved all the literature about unilateral and BPS fixation after lumbar fusion in recent years and included the latest randomized controlled trials (RCTs) and prospective cohort studies. The results were meta-analyzed to provide a reference for future clinical work.
MATERIALS AND METHODS
Literature search
We retrieved relevant studies using “Unilateral Pedicle Screw fixation,” “lumbar interbody fusion,” “lumbar degenerative diseases” along with “Bilateral Pedicle Screw fixation,” as key words with Boolean operators “AND” or “OR” in electronic databases, namely, EMBASE, the Cochrane Library and PubMed as of January 2020. While only prospective cohort studies and RCTs carried out upon human subjects were kept for further use. For presenting the flowchart of the trial selection, Figure 1 has been worked out. PRISMA guidelines, Cochrane Handbook and GRADE system are adopted as well for assessing qualities from involved study so as for convincing that the data herein presented were not only reliable but verifiable as well[10-12].
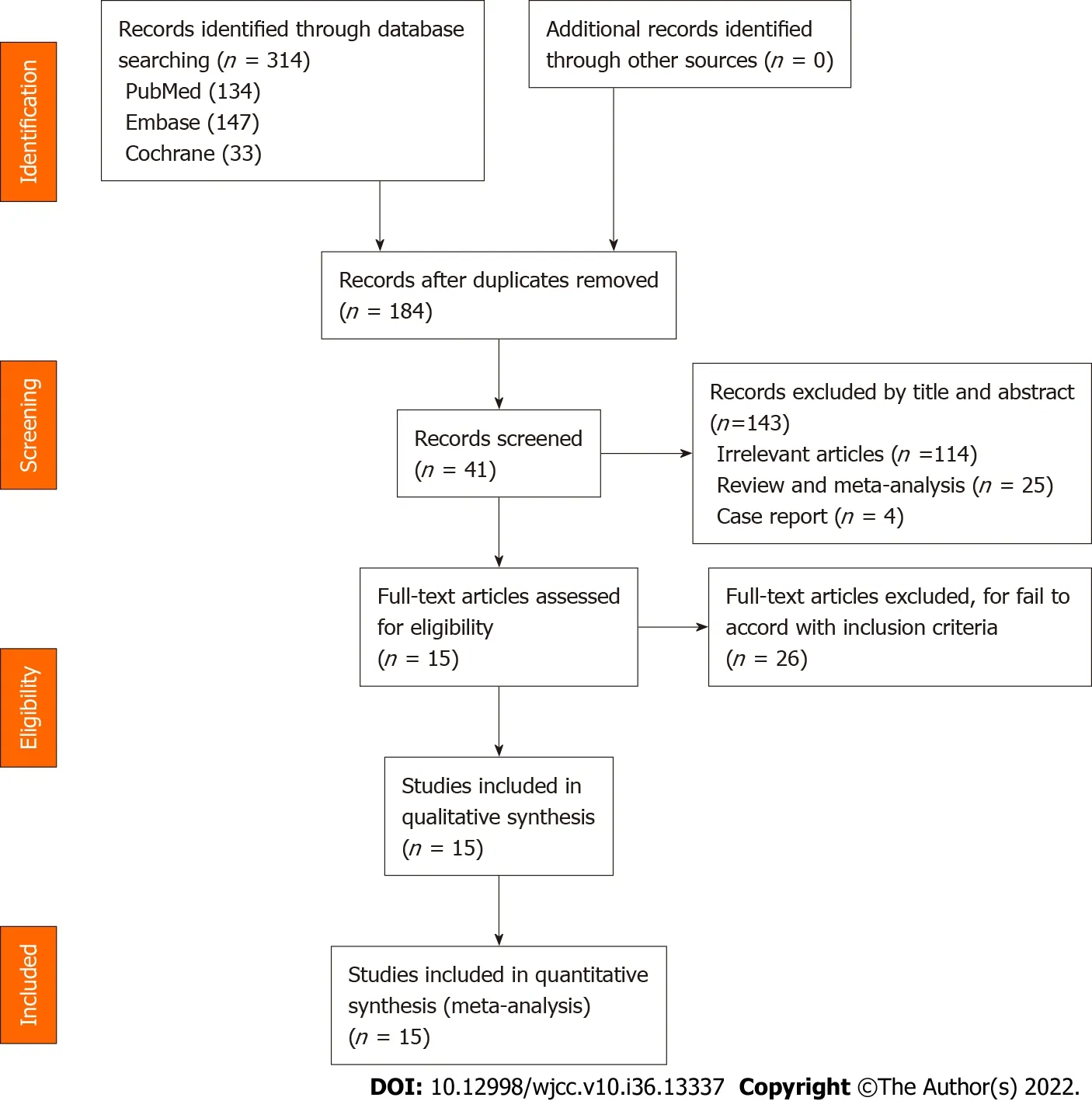
Figure 1 Flow diagram of study searching and selection process.
Selection criteria
The PICOS (Population, Intervention, Comparison, Outcome, and Study design) outline was used for including studies in the review. Inclusion criteria: (1) RCTs or prospective cohort studies; (2) The study population was patients with BPS fixation or UPS one after lumbar interbody fusion; (3) The intervention was UPS fixation, UPS fixation was also adopted for comparison; and (4) The primary outcomes were fusion rate and complications such as screw loosening, cage migration, infection, psoas, and neural symptoms. The secondary outcomes included changes in the following: Visual Analog Scale (VAS) score, Oswestry Disability Index (ODI) score, Japanese Orthopedic Association (JOA) score, operation time, total blood loss, as well as in-hospital duration. Exclusion criteria were: (1) No report on fusion rate or complication rate; (2) Study on recurrent lumbar diseases or revision surgeries; and (3) Repeated studies.
Data extraction
Two independent researchers searched the papers independently using the same search strategy, and a third researcher resolved any disagreement. Two reviewers collected the obtainable data from the involved studies independently, and any disagreement between the two reviewers was resolved by a third reviewer. Relevant data consist of names of the authors, dates of publication, types of intervention, ages, sample sizes, outcomes, follow-up duration, and types of reference. we obtained the outcome data, or estimated statisticsviathe data provided either in tables or in figures if we could not obtain the data directly from the statements of the articles. We present the baseline characteristics of the involved trials in Table 1.
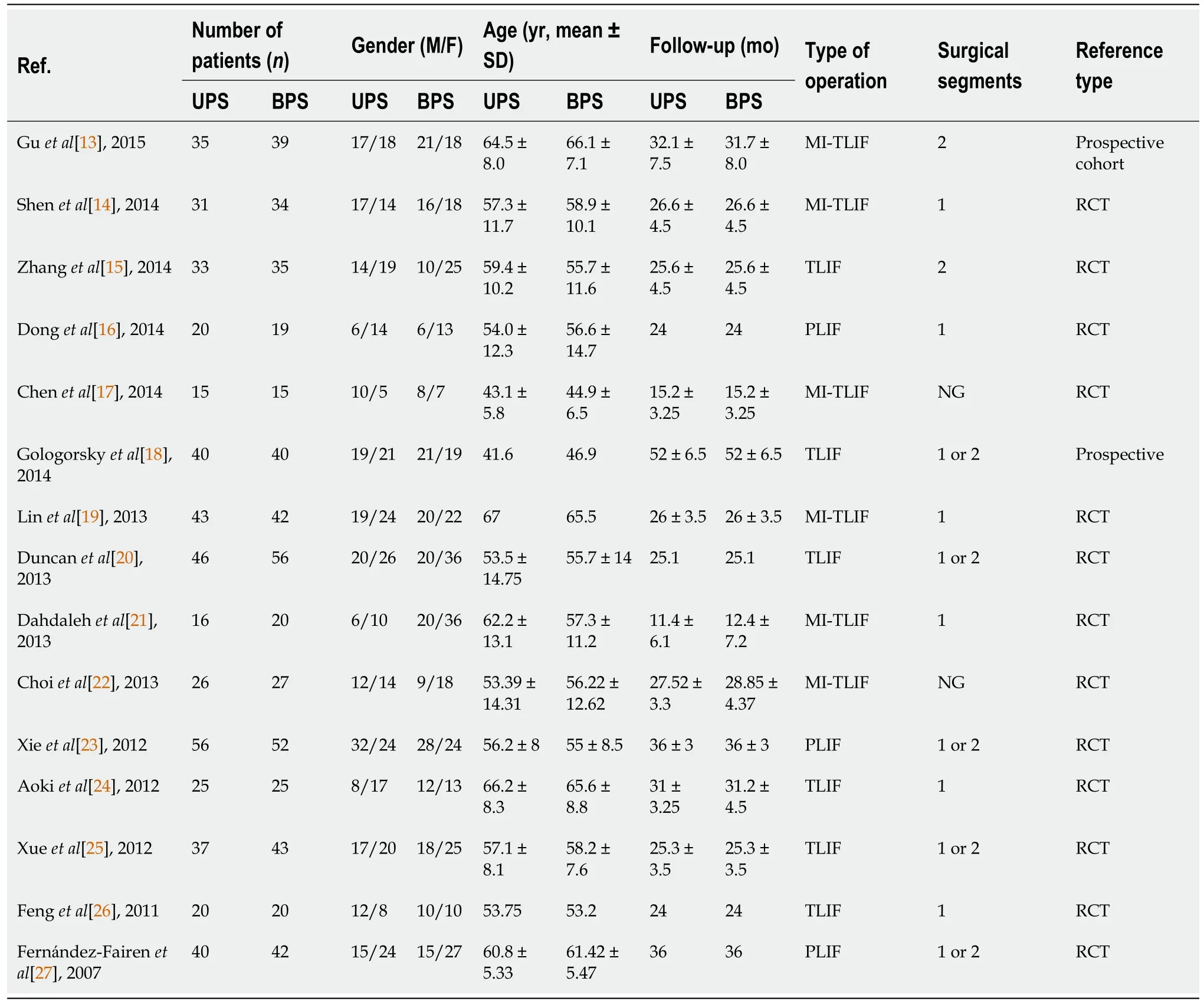
Table 1 Characteristics of included randomized controlled trial
Risk of bias assessment
The methodological qualities and foundation of the involved studies were assessed in accordance with the Cochrane Handbook for Systematic Reviews of Interventions. Based on the included literature, the two researchers evaluated adequate sequence generation, allocation concealment, binding, selective reporting, and other bias as being at high, low, or unclear risks of bias. If there were any inconsistency, the third researcher would be consulted to deal with it (Figures 2 and 3).

Figure 2 Risk of bias graph.

Figure 3 Risk of bias summary.
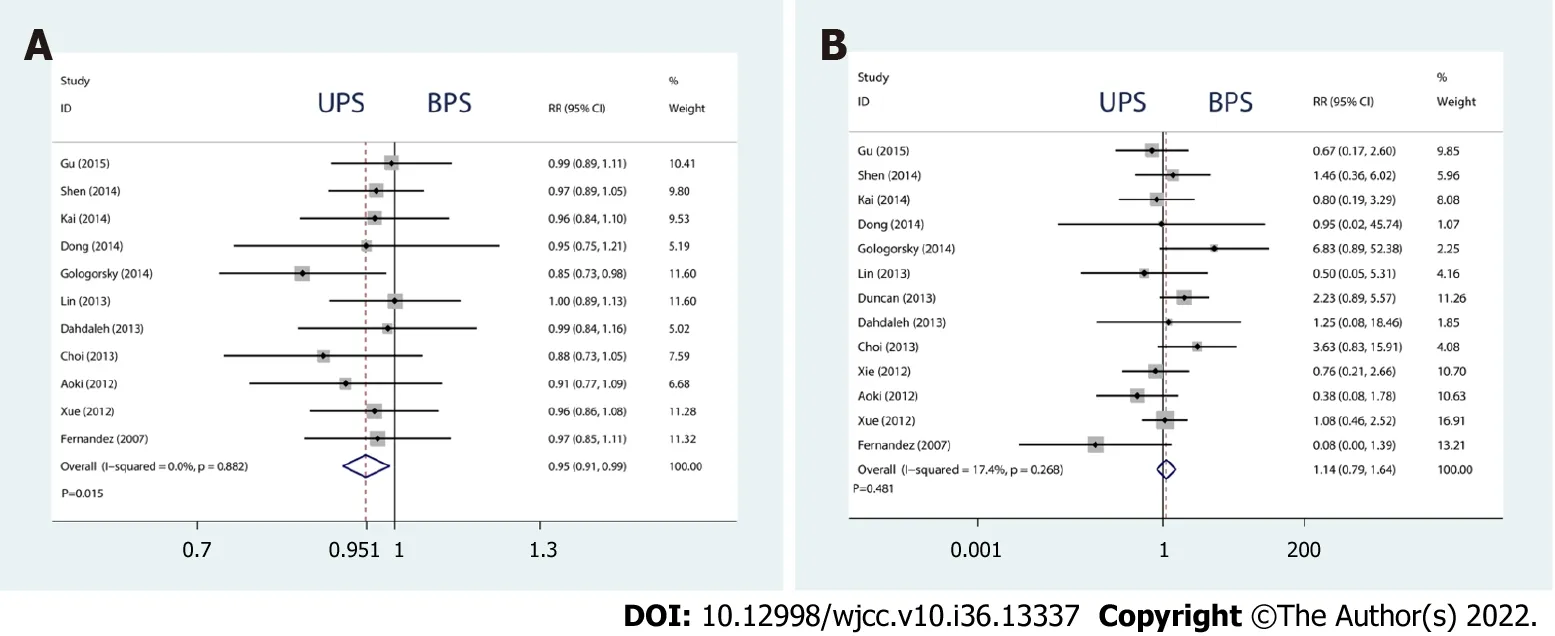
Figure 4 Forest plots of fusion rates and complications. A: Fusion rates; B: Complications.
Grading quality of evidence
The GRADE software has been used to conduct evaluation on the convincing level of evidence and strength of recommendations for the involved outcomes. Initially, RCTs were considered to have high confidence, and cohort studies low confidence as for the estimate of effect. Factors which may have decreased the level of confidence level included inconsistency, limitations, imprecision, indirectness, as well as publication bias. Factors that may have raised confidence level consisted of plausible confounding, large effect and dose-response. We present the results of GRADE analysis in Table 2.
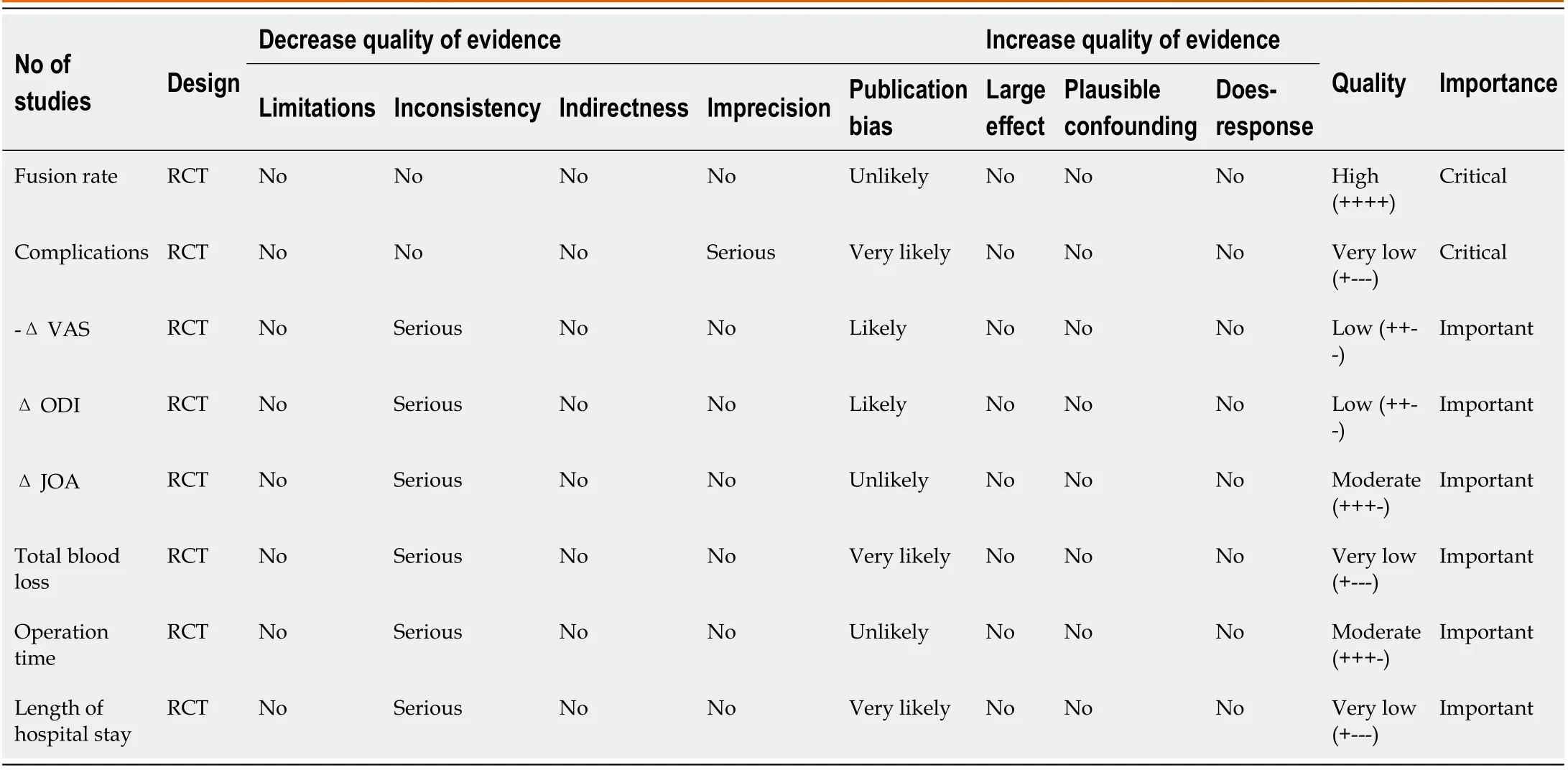
Table 2 The GRADE evidence quality for each outcome
Statistical analysis
Meta-analyses have been conducted using RevMan 5.3 software and STATA 13.1. The Standard Mean Difference (SMD) has been applied to make assessment of consecutive outcomes, with 95% Confidence Interval (CI). Relative Risk (RR) with 95%CI was adopted to make assessments of the dichotomous outcomes. The inverse variance, Mantel-Haenszel, and DerSimonian-Laird approaches have been applied to make combination of separated statistics. The results have been considered statistically important atPvalues < 0.05.
Investigation of heterogeneity and publication bias
Heterogeneity out of studies has undergone evaluationviaI2values and and considered high ifI2≥ 50% or low ifI2< 50%, respectively. An fixed-effects model was adopted whenI2≥ 50%, whereas an effect model of random type was used whenI2< 50%. Subgroup analyses and sensitivity analysis ones have been conducted to figure out the heterogeneity source, whileI2≥ 50%. Stata13.1 adopted for evaluation of the publication bias.
RESULTS
Search results
According to the index words, 314 citations were identified from the electronic databases. A total of 130 citations were duplicated, and 143 citations were excluded from the title and abstract, such as irrelevant articles, reviews, and case reports. Additionally, 26 retrospective studies were excluded from the analysis. Ultimately, 15 RCTs were included[13-27]. However, the limitation is that not every study included contains every outcome of interest. We summarized the characteristics of the involved studies and presented in Table 1.
Primary outcome
The complications and fusion rate of the two internal fixations were the primary outcomes from the meta-analysis, used for evaluating efficacy and safety.
Fusion rate
Eleven studies assessed the fusion rate of 708 patients followed up for at least 12 mo. Compared with BPS, UPS had a slightly lower fusion rate (RR = 0.949, 95%CI: 0.910 to 0.990,P= 0.015, Figure 4A). The age subgroup analysis indicated that the significant difference disappeared in patients aged > 60 years (RR = 0.975, 95%CI: 0.914 to 1.041,P= 0.455, Figure 5A). The type of operation subgroup analysis showed that TLIP significantly reduced the fusion rate of the UPS (SMD = 0.921, 95%CI: 0.857 to 0.988,P= 0.022, Figure 5B).
Complications
Thirteen studies assessed the fusion cage migration rate of 918 patients followed up for at least 12 mo. No drastic difference has been observed between both internal fixation approaches (RR = 1.140, 95%CI: 0.792 to 1.640,P= 0.481, Figure 4B).

Figure 5 Forest plots of subgroup analysis.
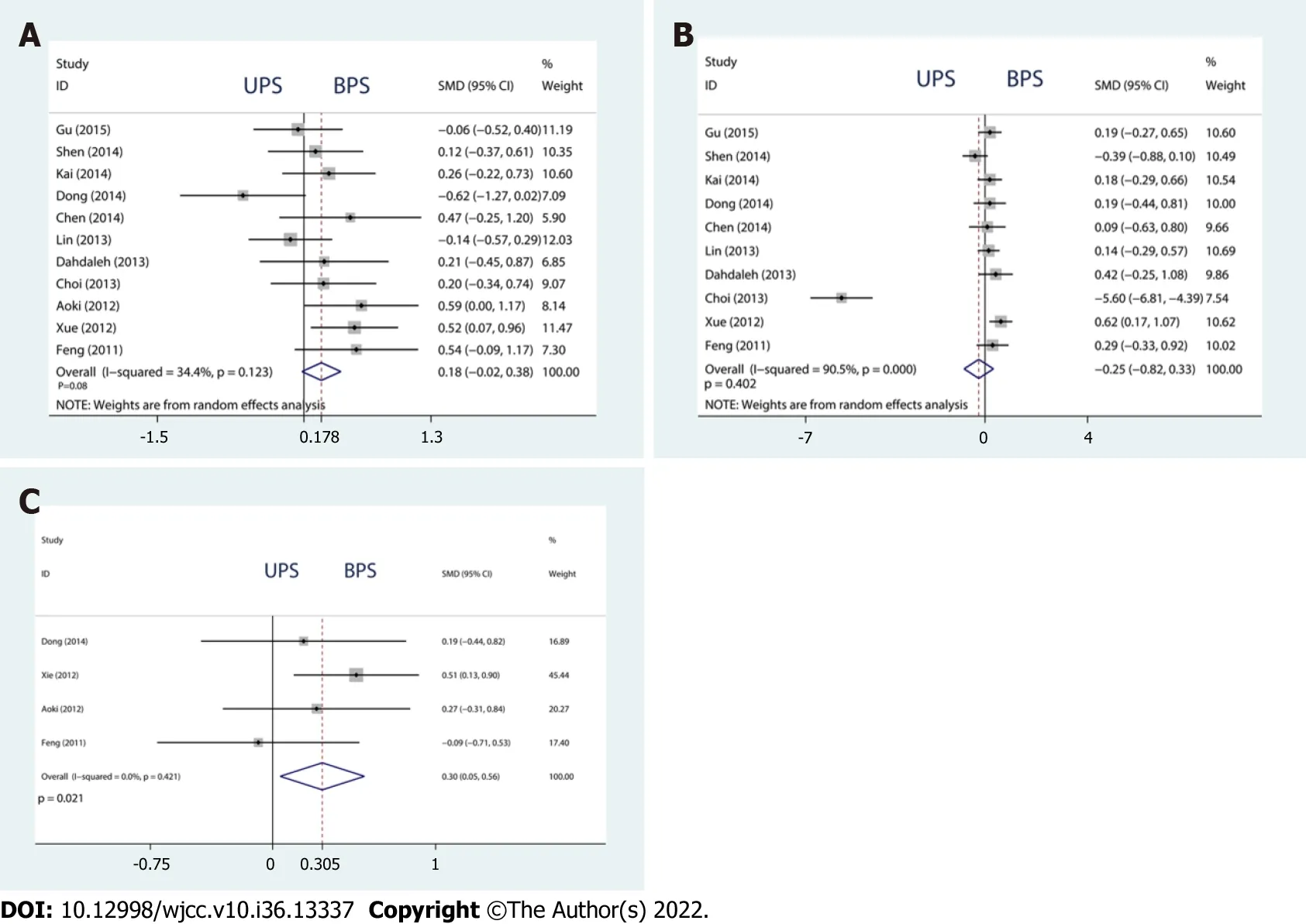
Figure 6 Forest plots of Δ visual analog scale, Δ Oswestry disability index, and Δ Japanese Orthopedic Association. A: Δ visual analog scale; B: Δ Oswestry disability index; C: Δ Japanese Orthopedic Association.
Secondary outcome
The enhancements in VAS, JOA, and ODI scores were considered subjective. To some extent, operation, blood loss, as well as in-hospital duration depended upon the surgeon’s proficiency. Therefore, these outcomes are secondary but essential indicators of prognosis in clinical practice.
Improvement of VAS, ODI and JOA:There was no significant difference in ΔVAS or ΔODI (ΔVAS, SMD = 0.178, 95%CI: -0.021 to 0.378,P= 0.080; ΔODI, SMD = -0.254, 95%CI: -0.820 to 0.329,P= 0.402, Figure 6A and B). However, compared with BPS, UPS significantly improved ΔJOA (SMD = 0.305, 95%CI: 0.046 to 0.563,P= 0.021, Figure 6C).
Total blood loss, operation time, as well as in-hospital duration:Compared with BPS, UPS significantly reduced the total blood loss, operation time, and length of hospital stay (total blood loss, SMD = -1.586, 95%CI: -2.182 to -0.990,P= 0.000; operation time, SMD = -2.831, 95%CI: -3.753 to -1.909,P= 0.000; length of hospital stay, SMD = -0.614, 95%CI: -1.050 to -0.179,P= 0.006, Figure 7A-C).
Quality assessment
We present baseline characteristics of the involved trials in Table 1, and results of GRADE analysis are presented in Table 2. The included studies met the principles of randomized controlled trials with a high level of evidence (Figures 2 and 3). Given medical ethics and patients’ informed consent rights, these RCTs rarely mention whether to adopt allocation concealment and blind methods, especially single-blind methods. We used the Harbord method and considered that no significant publication bias has been observed in the fusion rate (P= 0.710, Figure 8A). We conducted a sensitivity analysis with metatrim and metaninf and considered the included studies to be steady (Figure 8B and C).
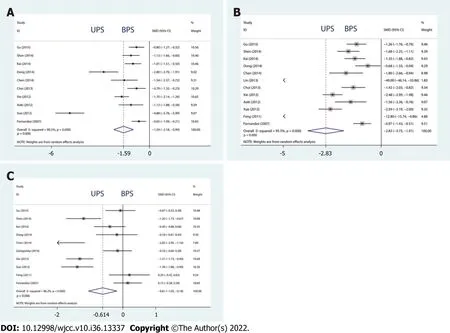
Figure 7 Forest plots of total blood loss, operation time, and length of hospital stay. A: Total blood loss; B: Operation time; C: Length of hospital stay.

Figure 8 Publication bias, metatrim, and metaninf of fusion rate. A: Publication bias; B: Metatrim; C: Metaninf.
DISCUSSION
This study suggested that UPS had a poorer fusion rate but significantly improved prognosis regarding several clinical outcomes.
However, the choice between unilateral and BPS fixation after lumbar fusion remains controversial. The BPS provides greater immediate stability, and the UPS significantly decreases the stiffness of the instrumented segment and surgical trauma. In recent years, many clinical follow-up studies and human cadaver studies have shown that UPS is as effective as BPS, and that UPS can achieve biomechanical stability comparable to that of BPS[28-32]. Computer simulation studies, such as finite element studies, also support UPS[33].
However, there are some objections to this approach. Kasai reported that UPS offers only uneven fixation in a human cadaver study, whereas BPS may allow excellent fixation in all directions[34]. Schleicher performed stiffness testing in fresh-frozen human cadaveric lumbar spine motion segments and concluded that BPS offers significantly more stability than UPS in the majority of test modes[35]. Many studies have found no significant difference in only one- or two-level interbody fusion[36]. Our study shows that there is a slightly lower fusion rate in UPS, even with short-segment fixation, which is different from those reported previously[37,38]. In terms of the rate of fusion cage migration, previous studies have found that UPS generates more cage migration than BPS[39]. After synthesizing the newly published studies, our evidence shows no difference in the rate of fusion cage migration between UPS and BPS. In terms of Improvement of VAS, ODI and JOA, there was no difference between UPS and BPS, which was consistent with the conclusion of previous studies[39]. In terms of total blood loss, operation time, and the length of hospital stay, UPS was lower than BPS, which was consistent with the actual clinical situation. Unilateral PS fixation avoided contralateral exposure and reduced trauma. Therefore, UPS fixation can not only shorten the operation time and reduce surgical trauma, but also reduce the recovery time[40]. GRADE is one of the widely adopted approaches in industries of public health and medicine to make assessment of the evidence’s outcome-specific certainty through systematically conducted reviews[41]. Our results show that the level of evidence is high. Therefore, we believe that this is the main contribution of the present meta-analysis. Although UPS has many advantages, BPS is much preferred, assuming there isn’t sufficient stability, such as during long segment fixation. However, current data only provide weak support, if any, favoring BPS over UPS for clinical improvement in fusion rates.
Within aging populations, there is a significant increase in lumbar degenerative diseases (LDD), resulting in great pain and reduced quality of life for patients[42]. Early increase of fusion rate and relief of pain, so that patients can move early, can effectively reduce venous thrombosis, pulmonary infection, pressure sores, and other complications[7,43]. Shortening hospital stay and reducing nosocomial infections are particularly important for the recovery of elderly patients[44]. Thus, it is urgently demanded to explore feasible, secure, and effective treatments for LDD.
Our study also has some limitations. First, all studies were single-center studies with small sizes of samples, which could possibly bring about selection bias. Second, none of the RCTs included in this study used blinding methods. Because of the type of intervention, blinding could not be performed to prevent the placebo effect or observer bias, resulting in low quality of the methodology. Third, different studies had different follow-up times, and the follow-up time of some studies was short. Finally, differences in diagnostic criteria, inclusion and exclusion criteria and details of treatment resulted in heterogeneity in the meta-analysis. Although subgroup and sensitivity analyses have been conducted, confounding statistical outcomes resulted from heterogeneity cannot be excluded to a complete extent.
CONCLUSION
According to our meta-analysis, UPS had a slightly poorer fusion rate but significantly improved prognosis regarding many important clinical outcomes, possibly associated with minimal invasion. To clarify whether UPS has the same reliability and effectiveness as BPS, longer follow-up and more clinical trials, especially RCTs, are required to provide stronger evidence regarding this observation. Further multicenter studies with more patients are required to obtain more reliable results.
ARTICLE HIGHLIGHTS
Research background
The use of unilateral pedicle screw (UPS) or bilateral pedicle screw (BPS) fixation for lumbar degenerative diseases remains controversial.
Research motivation
To provide objective evidence for the selection of UPS or BPS fixation for lumbar degenerative diseases.
Research objectives
To compare the efficacy and safety of UPS and BPS fixation in patients with lumbar degenerative diseases.
Research methods
We used meta-analysis to systematically review the current evidence.
Research results
UPS had slightly lower effects on fusion rate, which was the main contribution of this meta-analysis, and similar complication rates, Δ visual analog scale, and Δ Oswestry disability index. In contrast, there was a significant difference in Δ Japanese Orthopedic Association (JOA) score, total blood loss, operation time, and length of hospital stay.
Research conclusions
Unilateral fixation is less effective than bilateral fixation regarding fusion rate after lumbar interbody fusion. However, JOA, total blood loss, operation time, and length of stay were improved for unilateral fixation.
Research perspectives
To clarify whether UPS has the same reliability and effectiveness as BPS, longer follow-up and more clinical trials, especially RCTs, are required to provide stronger evidence regarding this observation. Further multicenter studies with more patients are required to obtain more reliable results.
FOOTNOTES
Author contributions:Sun L, Tian AX and Ma JX designed research, performed research, and wrote the paper; Ma XL was a major contributor in writing the manuscript and analyzed data, and all authors read and approved the final manuscript.
Supported bythe Health Science and Technology of Tianjin Municipality, No. RC20204; Tianjin Institute of Orthopedics, No. 2019TJGYSKY03; and the National Natural Science Foundation of China, No. 818717771177226.
Conflict-of-interest statement:The authors declare no competing interests.
PRISMA 2009 Checklist statement:The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Xin-Long Ma 0000-0002-6289-018X.
S-Editor:Zhang H
L-Editor:A
P-Editor:Zhang H
 World Journal of Clinical Cases2022年36期
World Journal of Clinical Cases2022年36期
- World Journal of Clinical Cases的其它文章
- Liver injury in COVID-19: Holds ferritinophagy-mediated ferroptosis accountable
- Amebic liver abscess by Entamoeba histolytica
- Living with liver disease in the era of COVID-19-the impact of the epidemic and the threat to high-risk populations
- Cortical bone trajectory screws in the treatment of lumbar degenerative disc disease in patients with osteoporosis
- Probiotics for preventing gestational diabetes in overweight or obese pregnant women: A review
- Effectiveness of microwave endometrial ablation combined with hysteroscopic transcervical resection in treating submucous uterine myomas
