Thoracic para-aortic lymph node recurrence in patients with esophageal squamous cell carcinoma: A propensity score-matching analysis
Xu-Yuan Li, Li-Sheng Huang, Shu-Han Yu, Dan Xie
Xu-Yuan Li, Shu-Han Yu, Department of Medical Oncology, Shantou Central Hospital, Shantou 515041, Guangdong Province, China
Li-Sheng Huang, Department of Radiation Oncology, Cancer Hospital of Shantou University Medical College, Shantou 515041, Guangdong Province, China
Dan Xie, Department of Radiology, Shantou Central Hospital, Shantou 515041, Guangdong Province, China
Abstract BACKGROUND Thoracic para-aortic lymph node (TPLN) recurrence in esophageal squamous cell carcinoma (ESCC) is rare and its impact on survival is unknown. We studied survival in patients with ESCC who developed TPLN recurrence.AIM To study the survival in patients with ESCC who developed TPLNs recurrence.METHODS Data were collected retrospectively for 219 patients who had undergone curative surgery for ESCC during January 2012 to November 2017 and who developed recurrences (36.29% of 604 patients who had undergone curative surgeries for ESCC). The patients were classified into positive (+) and negative (-) TPLN metastasis subgroups. We also investigated TPLN recurrence in 223 patients with ESCC following definitive chemoradiotherapy during 2012-2013. Following propensity score matching (PSM) and survival estimation, factors predictive of overall survival (OS) were explored using a Cox proportional hazards model.RESULTS Among the patients with confirmed recurrence, 18 were TPLN (+) and 13 developed synchronous distant metastases. Before PSM, TPLN (+) was associated with worse recurrence-free (P = 0.00049) and OS [vs TPLN (-); P = 0.0027], whereas only the intergroup difference in recurrence-free survival remained significant after PSM (P = 0.013). The Cox analysis yielded similar results. Among the patients who had received definitive chemoradiotherapy, 3 (1.35%) had preoperative TPLN enlargement and none had developed recurrences.CONCLUSION TPLN metastasis is rare but may be associated with poor survival.
Key Words: Esophageal cancer; Surgery; Thoracic para-aortic lymph node; Overall survival; Metastasis
INTRODUCTION
Esophageal cancer is the fourth most common cause of cancer-related deaths in China[1]. Although the incidence of esophageal squamous cell carcinoma (ESCC) has decreased in Western countries[2], this subtype accounts for more than 90% of the esophageal cancer diagnoses in China. Currently, surgical resection is the mainstay of curative treatment, and preoperative chemoradiotherapy followed by esophagectomy is considered the standard treatment for locally advanced esophageal cancer based on the accumulated evidence over the past 15 years[3-5].
Lymph node metastasis is among the most crucial negative prognostic factors affecting cancer patients[6]. Thoracic para-aortic lymph node (TPLN) metastasis, a rare complication of esophageal cancer, has only been described in a few case reports[7,8], although in one case report, it was observed that there was a higher incidence of metastasis with recurrent disease[9]. Generally, two-field lymphadenectomy is commonly performed in Western countries and China[3-5], whereas extended three-field lymphadenectomy is performed in Japan[10]. A Chinese consensus recommends the dissection of nine stations of mediastinal lymph nodes to achieve better local control and survival outcomes[11]. However, extensive lymph node dissection increases the number of postoperative complications[12]. Nevertheless, the established guidelines in China and Western countries do not specify dissection of the TPLNs, likely because of the low incidence of TPLN metastasis.
In this study, we reviewed the outcomes of patients who had undergone curative surgery for ESCC at our center to determine the incidence of TPLN metastasis and its impact on survival outcomes. We also reviewed patients who had received definitive chemoradiotherapy for ESCC and compared the effects of different treatment modalities on TPLN metastasis.
MATERIALS AND METHODS
This was a retrospective cohort study of anonymized data extracted from medical records. Approval for the use of medical records was obtained from the Ethics Committees of Shantou Central Hospital, China, prior to the study. All study protocols were approved by this committee.
We reviewed the medical records of consecutive patients who had undergone curative esophagectomy for pathologically proven ESCC between January 2012 and November 2017 at our Department of Surgery. The following information was extracted: Patient age, sex, work-up, treatments, and follow-up. Patients who met the following inclusion criteria were considered eligible: (1) Pathological diagnosis of squamous cell carcinoma; (2) Disease stage I-III; and (3) Surgical treatment with curative intent. The main exclusion criteria were a diagnosis of adenocarcinoma or other pathological type and stage IV disease. We further reviewed the records of consecutive patients who had received definitive chemoradiotherapy between January 2012 and December 2013 at the Department of Radiation Oncology. The inclusion criteria were as follows: (1) Pathological diagnosis of squamous cell carcinoma; (2) Disease stage I-III; and (3) Radiochemotherapy with curative intent.
At our center, the operative procedure for ESCC compriseden blocesophagectomy with two-field (mediastinal and upper abdominal) lymphadenectomy, gastric tube reconstruction, and cervical anastomosis. Mediastinal lymphadenectomy was performedviaa right thoracic approach and included the left and right recurrent, paraesophageal, paratracheal, and subcarinal regions and the inferior pulmonary ligament, as per the Chinese expert consensus on mediastinal lymph node dissection[11]. The pathological tumor stage was determined according to the seventh edition of the American Joint Committee on Cancer TNM classification (2009).
The location of the TPLN was defined as previously described[13], namely, the posterior mediastinum surrounded by the descending thoracic aorta, inferior pulmonary vein, pericardium, and thoracic duct. Positive recurrent TPLN was determined based on any of the following computed tomography (CT) findings: (1) Presence of lymph nodes in an area where they were not detected preoperatively, irrespective of size; and (2) Enlargement of preexisting lymph nodes in this area.
Recurrence was defined as the first documented radiographic evidence of disease relapse. The recurrence-free survival (RFS) and overall survival (OS) rates were estimated using the Kaplan-Meier method and compared using the log-rank test. Comparisons of categorical data were performed using the chi-squared test. APvalue < 0.05 indicated statistical significance.
A Cox regression model was used to identify prognostic factors, and logistic regression was used to explore the relationships between clinicopathological factors and TPLN recurrence. We performed a propensity score-matching analysis (with variables including age, sex, tumor location, tumor grade, T stage, nodal status, and type of adjuvant therapy) based on the one-to-many nearest neighbor method (caliper width: 0.1)[14]. AllPvalues were two-sided, and all statistical analyses were performed using R software (version i386 3.3.2; R Project for Statistical Computing, Vienna, Austria).
RESULTS
Between January 2012 and November 2017, 604 patients who had been diagnosed with pathologically proven ESCC underwent curative esophagectomy and lymphadenectomy at our center. The R0 reaction rate was 98.34% (594/604). Regarding perioperative mortality, no deaths occurred within 30 d after surgery. A median of 20 lymph nodes were harvested, and positive lymph nodes were observed in 294 (48.68%) of the 604 patients. The median follow-up was 38.63 mo. Among the patients (Supplementary Table 1), we recorded 89 (14.74%) deaths without a known cause, 39 (6.46%) patients lost to follow-up, 257 (42.55%) patients who remained alive without radiographic evidence of recurrence, and 219 (36.26%) patients who developed recurrences. The patients with recurrence were separated into two groups based on the presence of TPLN recurrence: TPLN (+) and TPLN (-). Eighteen of the six hundred and four patients (2.98%) had TPLN recurrence, and 13 of these patients developed synchronous distant metastases.
Figure 1 shows an example of TPLN recurrence after surgery in a representative patient. In the TPLN (+) group, 4 (4/604, 0.66%) patients presented with small TPLNs before surgery. The diameters of these small TPLNs ranged from 5.5 to 8.2 mm (mean, 6.73 mm). The TPLNs in these 4 patients were not dissected during surgery. Two patients received adjuvant chemoradiotherapy postoperatively, and two received no adjuvant treatment.
Of the 223 patients diagnosed with thoracic ESCC who had undergone definitive chemoradiotherapy between January 2012 and December 2013, 3 (1.35%) presented with enlarged TPLNs before treatment (diameters: 5.4, 6.2, and 11.0 mm). After definitive therapy, all the TPLNs shrank and did not relapse during follow-up. No other TPLN recurrences were observed in this group. The characteristics of the two groups are shown in Table 1. The groups were well balanced before and after propensity score matching, and the logistic regression analysis did not indicate that any of these characteristics contributed to TPLN metastasis.
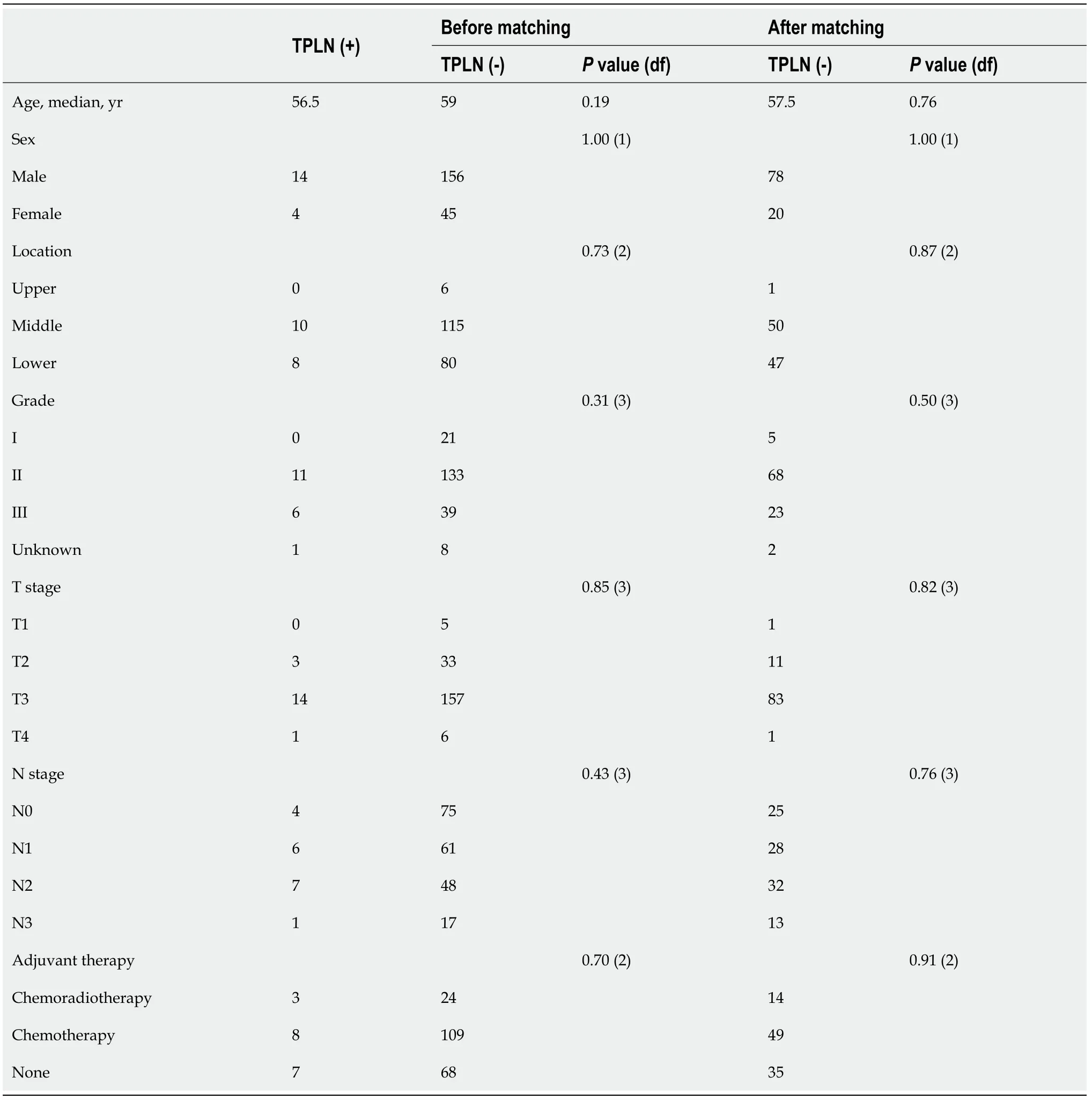
Table 1 Main characteristics
Before matching, the median RFS duration was significantly longer in the TPLN (-) group than in the TPLN (+) group [12.83 mo, 95% confidence interval (CI): 11.5-14.6vs6.35 mo, 95%CI: 3.4-15.4,P= 0.00049; Figure 2A). Similarly, the median OS duration was significantly longer in the TPLN (-) group than in the TPLN (+) group (21.47 mo, 95%CI: 19.37-26.60,vs15.30 mo, 95%CI: 11.90-28.30,P= 0.0027; Figure 2B).
After matching, the median RFS duration remained significantly longer in the TPLN (-) group than in the TPLN (+) group (12.00 mo, 95%CI: 9.8-14.0vs6.35 mo, 95%CI: 3.4-15.4,P= 0.013; Figure 2C). However, the difference in OS duration between the TPLN (-) and TPLN (+) groups was only borderline significant, despite the longer duration in the former group (18.25 mo, 95%CI: 16.7-24.1vs15.30 mo, 95%CI: 11.90-28.30,P= 0.051; Figure 2D). A Cox model analysis of potential prognostic factors similarly indicated the presence of TPLN metastasis as a risk factor for OS before matching but not after matching.
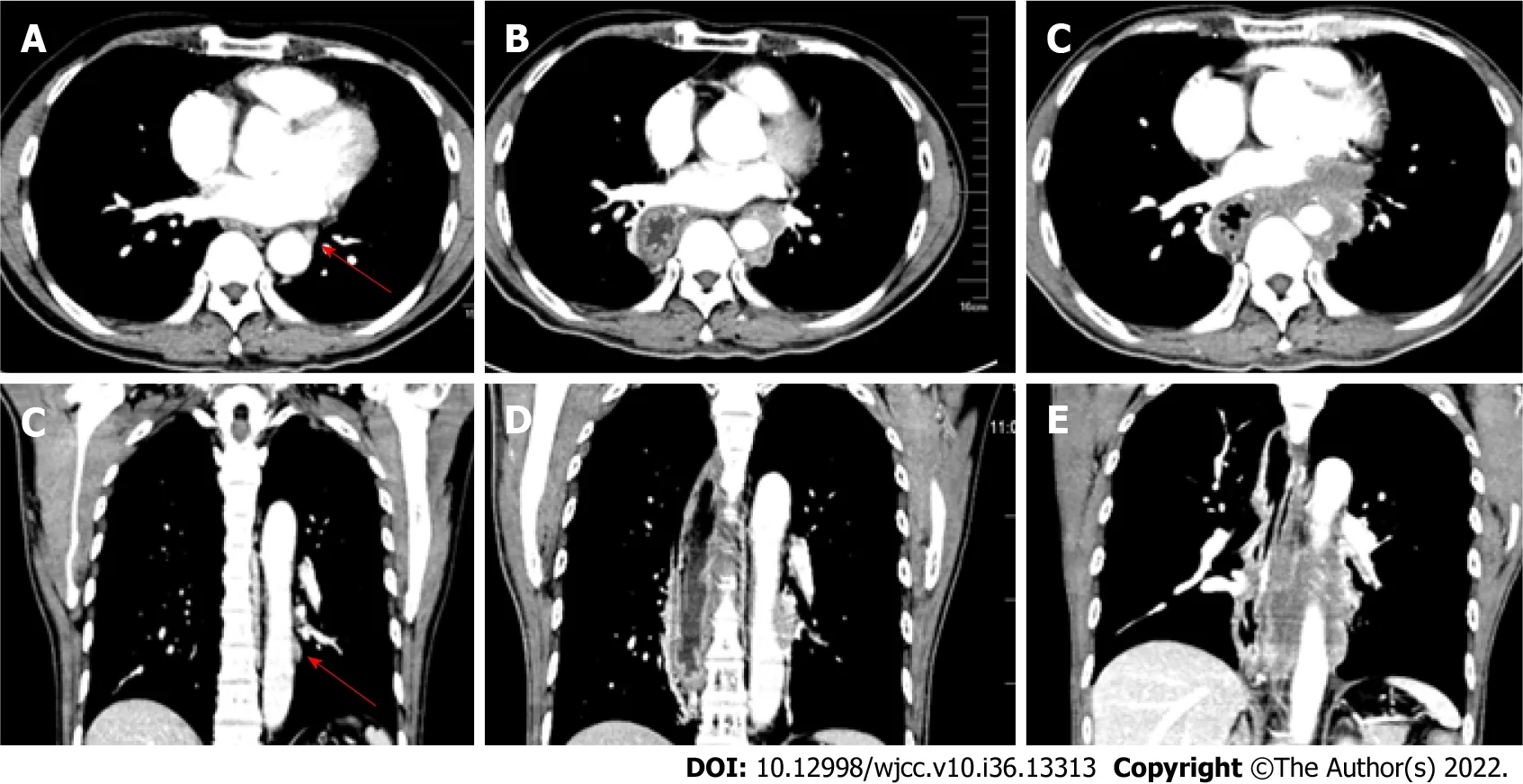
Figure 1 Computed tomography scan results. A and B: Small thoracic paraaortic lymph node (TPLN, arrow) in a patient before surgery; C and D: TPLN recurrence 3 mo after surgery; E and F: TPLN recurrence 5 mo after surgery.
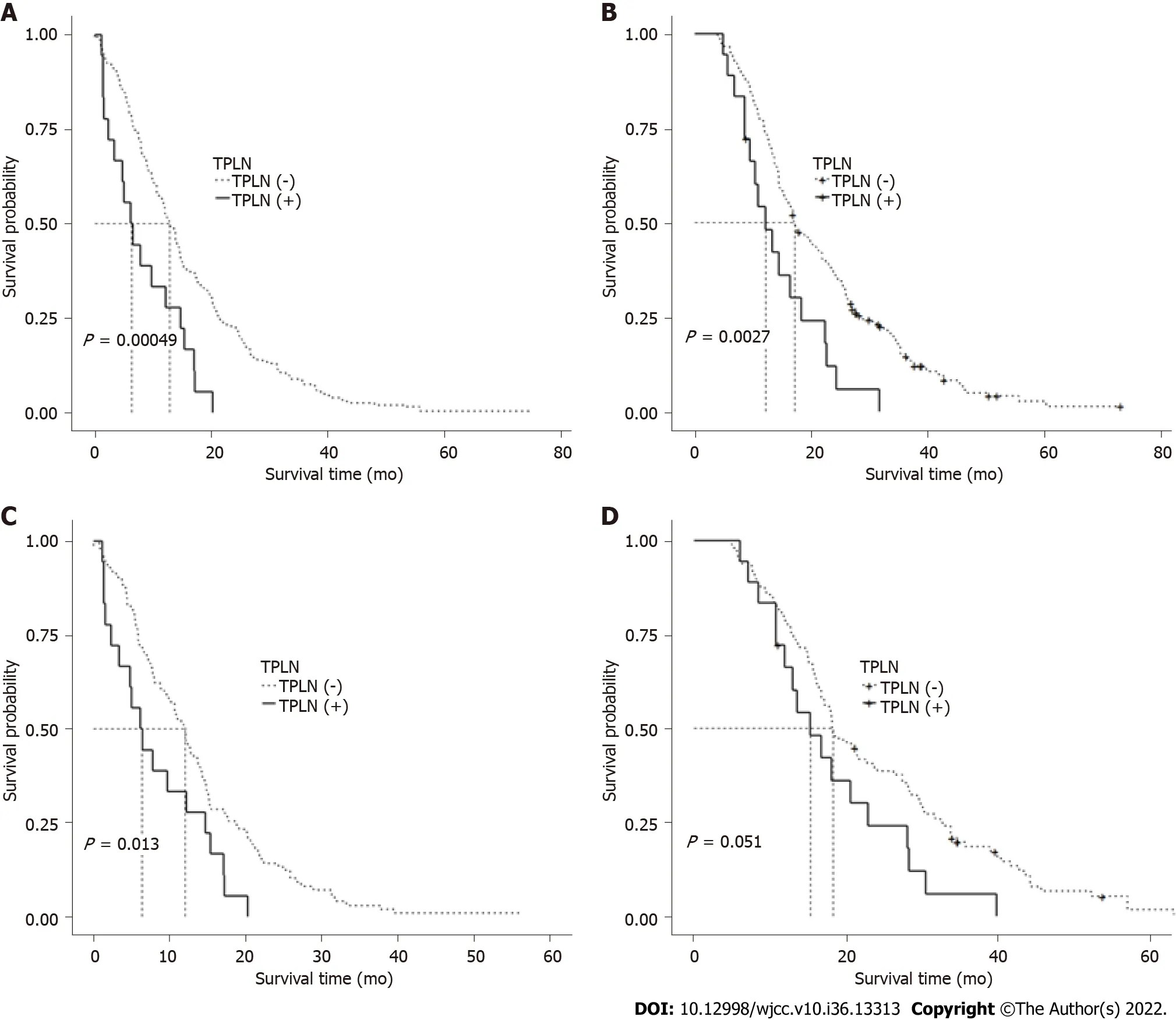
Figure 2 Comparison of recurrence-free survival and overall survival before propensity score matching. A: Comparison of recurrence-free survival (RFS) before propensity score matching; B: Comparison of overall survival (OS) before propensity score matching; C: Comparison of RFS after propensity score matching; D: Comparison of OS after propensity score matching. TPLN: Thoracic paraaortic lymph node.
DISCUSSION
Globally, the treatment of esophageal cancer remains challenging. For patients with locally advanced esophageal cancer, neoadjuvant chemoradiotherapy or chemoradiotherapy followed by surgery has led to significant improvements in survival relative to surgery alone[15]. However, in some scenarios, surgery represents mainly a curative method, along with definitive chemoradiotherapy.
As noted previously, lymph node metastasis is a strong prognostic factor in cancer cases. A higher number of dissected lymph nodes and increased station clearance are associated with more precise staging, better local control, and perhaps better OS, although these benefits may come at the cost of an increased risk of complications[16]. Consequently, efforts to enhance the radical dissection of lymph nodes include the progression from two-field to three-field lymphadenectomy[17] and a shift from a limited left thoracic approach to an extended right thoracic approach[18]. Despite these advances, surgeons might neglect stations associated with a low incidence of lymph node metastasis, such as TPLN. Few reports have described TPLN recurrence in cases of resectable esophageal cancer.
To the best of our knowledge, our study is the largest cohort study of TPLN recurrence, and our findings demonstrate that TPLN recurrence is associated with poor RFS and OS. We observed a TPLN recurrence rate of approximately 3%. In our cohort, TPLN recurrence did not occur in tumors located in the upper thoracic esophagus, in low-grade tumors (grade 1), or in tumors that had invaded the lamina propria, muscularis mucosae, or submucosa (T1 stage). However, we failed to identify any parameters significantly predictive of TPLN recurrence.
Despite our inability to identify predictive factors, our results have several implications for clinical practice. Previously, Shishidoet al[8] reported on 2 patients with enlarged TPLNs (10 mm) that were confirmed pathologically after dissection. In contrast, we identified small TPLNs (longest transverse diameter < 10 mm) in 4 patientsviaCT scans. Although such small TPLNs had not been previously considered indicative of a metastasis-positive status[19], all 4 of the TPLNs in our patients were swollen after surgery, indicating that the lymph nodes in the thoracic para-aortic area should be treated cautiously, irrespective of the transverse diameter. Moreover, in cases of esophageal cancer, we always intraoperatively harvest small lymph nodes that are pathologically proven to be positive after surgery. However, the value of positron emission tomography/CT scans has not been validated, and therefore, this imaging technique is not routinely applied at our center.
As mentioned above, TPLN is not included in the description of standard lymph node dissection in the guidelines used in China or Western countries, and the extent of LN station nine (i.e.,the pulmonary ligament area) does not necessarily include TPLNs[20]. Although we have performed esophageal surgery in more than 1700 cases at our center, we do not routinely clear this area. Moreover, some small lymph nodes in this area are often overlooked, which might explain the poor survival outcomes among our patients with TPLN recurrence.
In Japan, TPLNs are further classified as anterior or posterior. Posterior TPLNs are associated with worse RFS and OS outcomes than anterior TPLNs[13]. Currently, a left thoracic approach is recommended for the eradication of TPLNs. As reported, the posterior TPLNs were successfully dissectedviathis approach in 3 cases[7,8]. We support the recommendation for the left approach to posterior TPLNs; however, we consider the right thoracic approach to anterior TPLN dissection to be feasible.
Our study had several limitations. First, this was a retrospective study of a small sample of patients at a single treatment center, which had an inherent risk of bias by the nature of the study design. To overcome this limitation, we are currently building a database dedicated to capturing data on TPLNs. Second, before 2017, nearly all the patients with resectable esophageal cancer at our center were offered surgery as an initial treatment. This practice contrasts with the preferred initial treatment options in Western countries. However, most patients in Western countries present with esophageal adenocarcinoma, but the majority of patients in China have ESCC. Additionally, the benefit of neoadjuvant chemoradiotherapy in Chinese patients with ESCC has been confirmed only recently[5]. A further evaluation of TPLN is needed once this treatment paradigm has been fully introduced into clinical practice.
CONCLUSION
Our study results confirm the low incidence of TPLN metastasis and reveal a potential relationship between this complication and survival outcomes.
ARTICLE HIGHLIGHTS
Research background
Thoracic para-aortic lymph nodes (TPLNs) recurrence in esophageal squamous cell carcinoma (ESCC) is rare but with poor survival outcomes in clinical observation.
Research motivation
TPLNs recurrence had negative impact on survival outcomes in patients with ESCC.
Research objectives
TPLN (+) was associated with worse recurrence-free and overall survival (OS) in patients with ESCC.
Research methods
The propensity score-matching and survival estimation were applied, and factors predictive of OS were explored using a Cox proportional hazards model.
Research results
To study survival in patients with ESCC who developed TPLNs recurrence.
Research conclusions
To determine TPLNs recurrence rate and its impact on survival.
Research perspectives
TPLNs recurrence in ESCC is rare but with poor survival outcomes in clinical observation.
FOOTNOTES
Author contributions:Li XY and Huang LS contributed equally to this work; Li XY designed the research study; Xie D and Yu SH performed the research; Li XY, Huang LS, Xie D and Yu SH analyzed the data and wrote the manuscript; and all authors have read and approve the final manuscript.
Institutional review board statement:Approval for the use of medical records was obtained from the Ethics Committees of Shantou Central Hospital, China, prior to the study. All study protocols were approved by this committee.
Informed consent statement:Informed consent was waived by the IRB of the Shantou Central Hospital.
Conflict-of-interest statement:All the authors report having no relevant conflicts of interest for this article.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Xu-Yuan Li 0000-0003-2674-0974.
S-Editor:Wang JJ
L-Editor:Filipodia
P-Editor:Wang JJ
 World Journal of Clinical Cases2022年36期
World Journal of Clinical Cases2022年36期
- World Journal of Clinical Cases的其它文章
- Liver injury in COVID-19: Holds ferritinophagy-mediated ferroptosis accountable
- Amebic liver abscess by Entamoeba histolytica
- Living with liver disease in the era of COVID-19-the impact of the epidemic and the threat to high-risk populations
- Cortical bone trajectory screws in the treatment of lumbar degenerative disc disease in patients with osteoporosis
- Probiotics for preventing gestational diabetes in overweight or obese pregnant women: A review
- Effectiveness of microwave endometrial ablation combined with hysteroscopic transcervical resection in treating submucous uterine myomas
