Classification of rectal cancer according to recurrence types -comparison of Japanese guidelines and Western guidelines
Hiroshi Miyakita, Yutaro Kamei, Lin Fung Chan, Kazutake Okada, Hajime Kayano, Seiichiro Yamamoto
Hiroshi Miyakita, Yutaro Kamei, Lin Fung Chan, Kazutake Okada, Hajime Kayano, Seiichiro Yamamoto, Department of Digestive System Surgery, Tokai University School of Medicine,Isehara 259-1193, Kanagawa, Japan
Abstract BACKGROUND Rectal cancer is characterized by more local recurrence (LR) and lung metastasis than colon cancer. However, the diagnosis of rectal cancer is not standardized as there is no global consensus on its definition and classification. The classification of rectal cancer differs between Japanese and Western guidelines.AIM To clarify the characteristics of rectal cancer by comparing the tumor location and characteristics of rectal cancer with those of colon cancer according to each set of guidelines.METHODS A total of 958 patients with Stage II and III colorectal cancer were included in the analysis: 607 with colon cancer and 351 with rectal cancer. Localization of rectal cancers was assessed by enema examination and rigid endoscopy. According to Japan guidelines, rectal cancer is classified as Rb (below the peritoneal inversion), Ra (between the inferior margin of second sacral vertebrae and Rb) or RS (between Ra and sacral promontory).RESULTS There were no significant differences between RS rectal cancer and colon cancer in the rates of liver and lung metastasis or LR. Lung metastasis and LR were significantly more common among Rb rectal cancer (in Japan) than in colon cancer (P = 0.0043 and P = 0.0002, respectively). Lung metastases and LR occurred at significantly higher rates in rectal cancer measuring ≤ 12 cm and ≤ 10 cm than in colon cancers (P = 0.0117, P = 0.0467, P = 0.0036, P = 0.0010). Finally, the rates of liver metastasis, lung metastasis, and LR in rectal cancers measuring 11 cm to 15 cm were 6.9%, 2.8%, and 5.7%, respectively. These were equivalent to the rates in colon cancer.CONCLUSION High rectal cancer may be treated with the same treatment strategies as colon cancer. There was no difference in the classification of colorectal cancer between Japan and Western countries.
Key Words: Colon cancer; Metastasis; Local recurrence; Classification of rectal cancer; Western guidelines;Japanese guideline
INTRODUCTION
Colorectal cancer is the third major cause of death in the United States and has the third highest rate of new cases[1]. Similar numbers are observed in Japan, where colorectal cancer is the third major cause of mortality and the highest cause of morbidity among cancers[2]. Due to its anatomical characteristics, rectal cancer has significantly higher rates of local recurrence (LR) than colon cancer. However, the diagnostic criteria for rectal cancer have not been globally standardized. In Japan, rectal cancer is classified into Rb (below the peritoneal inversion), Ra (between the inferior margin of second sacral vertebrae and Rb) and RS (between Ra and sacral promontory) categories, and the localization of the bulk of the tumor is determined by enema examination[3]. According to guidelines in Western countries, such as the National Comprehensive Cancer Network (NCCN) and American Joint Committee on Cancer (AJCC) guidelines, rectal cancers are defined as lesions within ≤ 12 cm of the anal verge and are assessed by rigid endoscopy[4,5]. According to the European Society for Medical Oncology (ESMO), lesions from 0 cm to 5 cm of the anal verge are defined as low rectal cancer, and those from 5 cm to 10 cm of the anal verge are defined as mid-rectal cancer; indeed, none of the definitions are standardized[6].
In Europe, according to the ESMO guidelines, the standard therapy for patients with mid- or low rectal cancer is total mesorectal excision (TME) after chemoradiotherapy[6]. Cancers located more orally to this location are generally treated as colon cancer. Following the NCCN guidelines, in North America, patients with rectal cancer ≤ 12 cm from the anal verge undergo chemoradiotherapy followed by TME surgery[4,5]. In Japan, the standard therapy for rectal cancers located orally to Ra cancers is TME monotherapy. Moreover, rectal cancers located more anally than Rb cancers are treated by TME surgery and lateral lymph node dissection (LLND)[7,8]. This presents a further lack of standardization in the treatment of rectal cancer. Abdelsattaret al[9] noted inconsistencies in the guidelines for rectal cancer diagnosis and treatment. Although similar comparisons of guidelines for colorectal cancer have been made, a consensus on the topic has yet to be reached[10].
Although 80% of Ra and Rb rectal cancers are reported to correspond to mid- and low rectal cancer, respectively, the diagnoses of Ra and Rb rectal cancers are not necessarily compatible with those of midrectal and low rectal cancer, respectively[11]. Furthermore, tumors diagnosed as RS rectal cancer in Japan may also include tumors that correspond to cancers of the mid-rectum.
This study thus aimed to elucidate how rectal cancer is managed by investigating the relationship between rectal cancer localization in patients treated with radical resection at our facility using the various guidelines and their recurrence type and by subsequently comparing them with patients with colon cancer.
MATERIALS AND METHODS
This study was approved by the institutional review board of our university (20R-238), and all patients were provided written informed consent.
Patients
A total of 958 patients with Stage II and III colorectal cancer who underwent radical surgery between January 2005 and December 2014 were included in the analysis. A total of 607 patients that had colon cancer and 351 patients that had rectal cancer. A total of 217 patients with rectal cancer underwent preoperative chemoradiotherapy (CRT). Rectal cancer was treated surgically by TME monotherapy and none of the patients underwent LLND.
Classification
The segments of the colon including the cecum, ascending colon, transverse colon, descending colon, and sigmoid colon can all be involved in colon cancer. Rectal cancer was classified into RS, Ra, and Rb categories according to the Japanese Classification of Colorectal, Appendiceal, and Anal Carcinoma (JCCRC)[3]. The localization of rectal cancer was assessed by enema examination and rigid endoscopy. The type of recurrence was evaluated by comparing the rates of liver and lung metastasis as well as LR. LR included intrapelvic recurrences.
Enema examination
A double-contrast barium enema was performed by radiologists in all patients to determine the rectal division in which the main part of the tumor was located in accordance with the JCCRC guidelines (second English edition translated from the 7thJapanese edition of the general rules)[3,12,13]. Tumors that involved two divisions, such as “Rb-Ra,” were assigned to the major division,i.e.the one in which the bulk of the tumor was located. The tumor size was measured as the vertical extension on the lateral view of the barium enema. The location of the tumor in the bowel wall was described as involving the anterior, lateral, or posterior quadrants.
Statistical analysis
Fisher’s exact test or theχ2test was used to analyze categorical variables, and the Mann-Whitney U test or Kruskal-Wallis test and the Wilcoxon signed rank sum test were used for continuous variables. In all analyses,P <0.05 was considered statistically significant. The software package JMP10 (SAS Institute Inc., NC, United States) was used for statistical analysis.
RESULTS
Patient characteristics
Of the 958 patients, 580 were men and 378 were women, with a median age of 68 years. Of these, 607 had colon cancer, 351 patients had rectal cancer, and 281 underwent CRT. Overall, 482 patients had Stage II disease, and 379 had Stage III disease; 38 had ypStage 0 disease, and 59 had ypStage I disease. These were patients with rectal cancer who underwent CRT and for whom down staging was achieved (Table 1).
Distance to the lower border of the tumor according to localization by rigid endoscopy and enema examination
Rigid endoscopy was performed on 104 of the 351 patients with rectal cancer, and an enema examination was performed on all patients; the results are displayed in Table 2. The mean (SD) distance for RS, Ra, and Rb rectal cancer on rigid endoscopy was 10.3 cm, 7.7 cm, and 3.5 cm, respectively; and that for RS, Ra, and Rb rectal cancer on enema examination was 12.3 cm, 7.2 cm, and 3.2 cm respectively. There was almost no difference between the distances measured by rigid endoscopy and enema examination for Ra and Rb tumors, but there was a 2 cm difference for rectal cancers in the RS segment (Table 2).
Table 2 presents the distances from the anal verge to the lower border of the tumor in various segments measured by enema examination. The tumor was located ≥ 11 cm from the anal verge in 77 patients (73.2%) with RS cancer and ≤ 10 cm from the anal verge in 28 (26.6%) patients. For Ra and Rb cancers, tumors were located ≤ 10 cm from the anal verge in 84 (93.2%) patients and 156 (100%) patients, respectively.
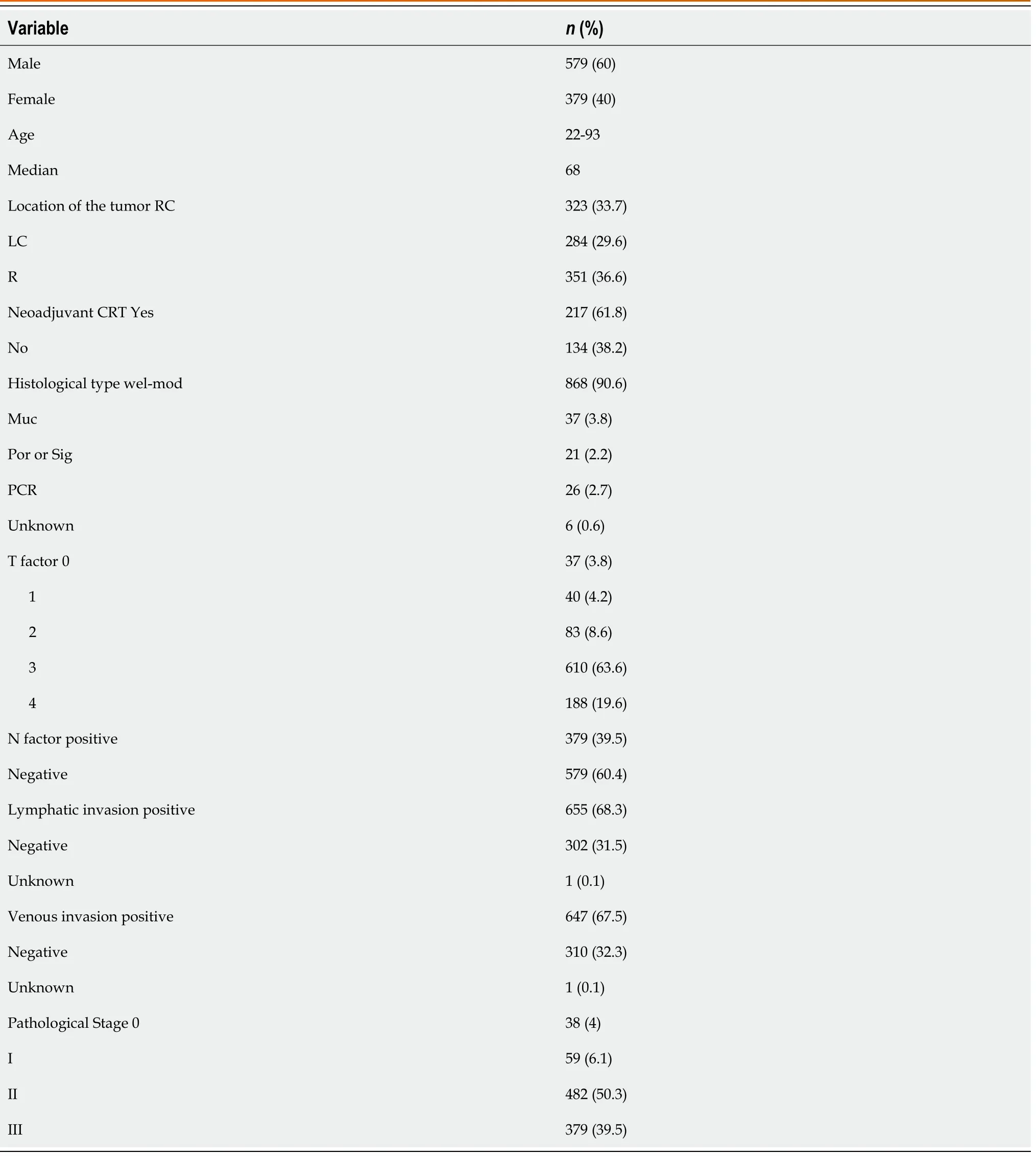
Table 1 Patients’ characteristics
Tumor localization and recurrence type
The recurrence type was classified according to colon cancer and rectal cancer. Rectal cancer was distinguished by CRT administration as it is associated with the LR rate, and they were classified according to the JCCRC, NCCN, AJCC, and ESMO guidelines. Since local recurrence is affected markedly by CRT, it was compared to patients who did not undergo CRT.
The rates of colon cancer with liver metastasis, lung metastasis, and LR were 12.6%, 5.4% and 3.4%, respectively. The rates of liver and lung metastasis in patients with rectal cancer who underwent CRT were 8.7% and 10.1%, respectively. The LR rate was 5.5% among patients who underwent CRT and 8.2% in patients who were treated with surgery alone.
Recurrence pattern according to the JCCRC guidelines
The rates of liver metastasis, lung metastasis, and LR in RS cancers according to the JCCRC guidelines were 7.5%, 4.7% and 5.7%, respectively. In Ra and Rb cancers, including in patients who underwent CRT, the liver metastasis, lung metastasis, and LR rates were 9.3%, 10.5% and 6.9%, respectively. The LR rate was 17.2% among patients who underwent surgery alone and 5.5% among patients who also underwent CRT. There were no significant differences between the rates of liver metastasis, lung metastasis, and local recurrence between RS cancer and colon cancer (P= 0.1491,P= 0.7737, andP= 0.2657, respectively) (Table 3).
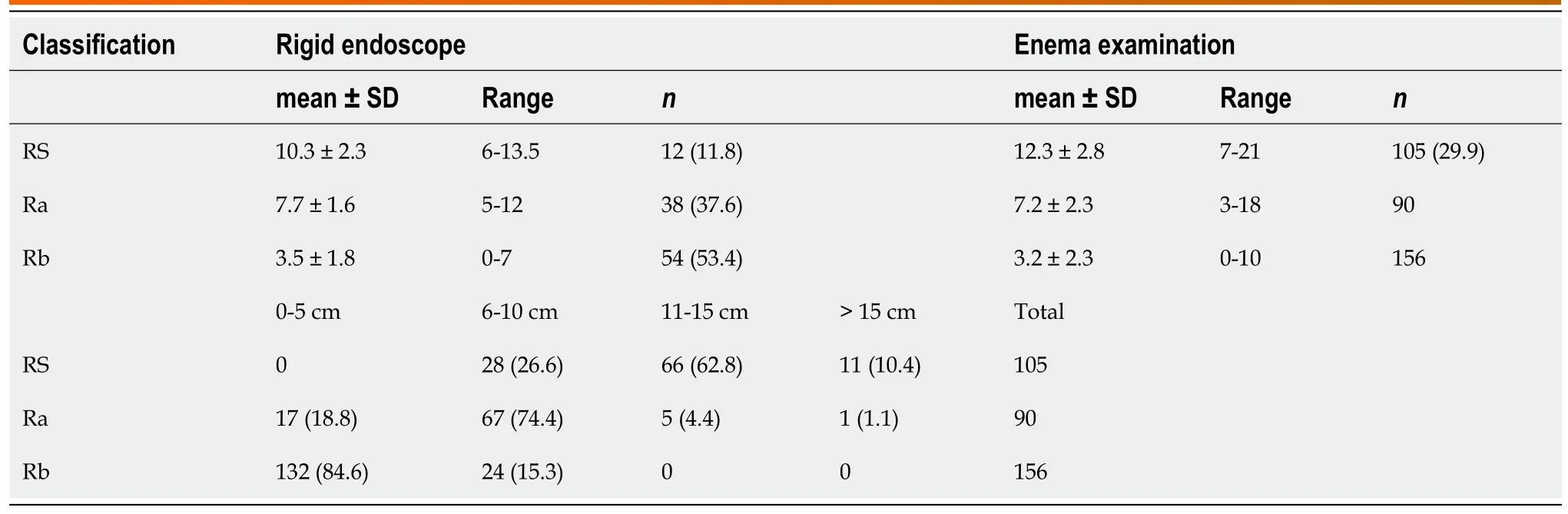
Table 2 Distance to the lower border of the tumor according to localization by rigid endoscopy and enema examination
Patients with Ra and Rb rectal cancer had significantly higher rates of lung metastasis than those with colon cancer (P= 0.0043). Ra and Rb cancer treated by surgery alone had significantly higher rates of local recurrence than colon cancer (P= 0.0002).
Recurrence pattern according to the NCCN and AJCC guidelines
According to the NCCN and AJCC guidelines, rectal cancer located ≤ 12 cm from the anal verge showed rates of liver and lung metastasis of 8.3% and 10.7%, respectively. The rate of liver and lung metastasis was significantly higher in rectal cancer ≤ 12 cm from the anal verge than in colon cancer (P= 0.0631,P= 0.0117). The LR rate was 8.5% in rectal cancer located ≤ 12 cm from the anal verge treated with surgical monotherapy. Therefore, the LR rate was significantly higher than that in colon cancers located orally less than 12 cm from the anal verge (P= 0.0467) (Table 4).
Recurrence pattern according to the ESMO guidelines
According to the ESMO guidelines, tumors ≤ 15 cm from the anal verge are classified as rectal cancer. Mid- or low rectal cancers are treated surgically, whereas lesions located more orally than ≥ 10 cm from the anal verge are generally treated the same as colon cancer. Consequently, comparisons were made based on rectal cancers located ≤ 10 cm from the anal verge. The rates of liver and lung metastasis of rectal cancer located ≤ 10 cm from the anal verge were 8.9% and 10.4%, respectively. Rectal cancer located ≤ 10 cm from the anal verge had significantly higher rates of liver and lung metastasis than colon cancer (P= 0.1752,P= 0.0036). The LR rate in rectal cancer located ≤ 10 cm from the anal verge treated with surgical monotherapy was 13.2%. This was significantly higher than the LR rate of colorectal cancer located more than 10 cm oral to the anal verge (P= 0.0010) (Table 5).
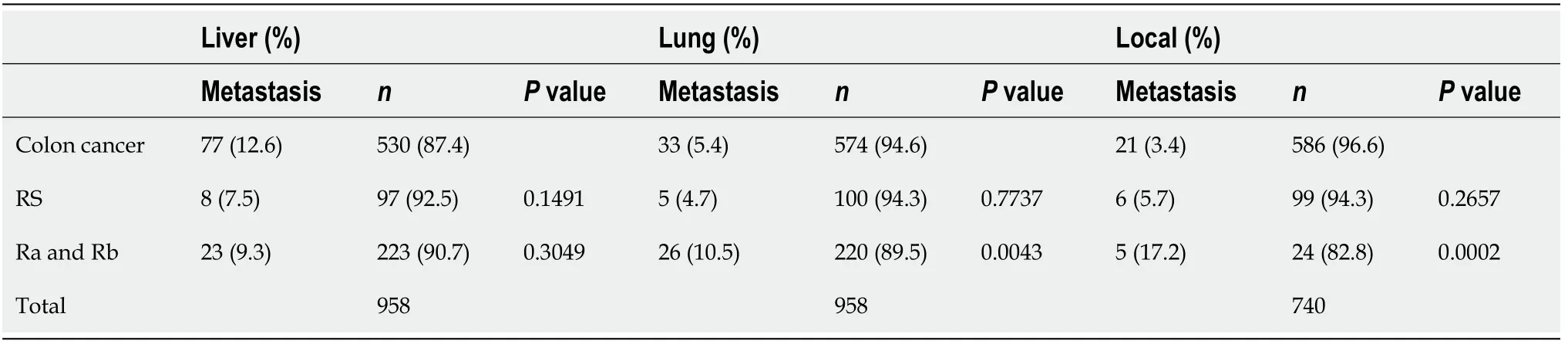
Table 3 Reccurence pattern according to Japanese Classification of Colorectal, Appendiceal, and Anal Carcinoma guidelines
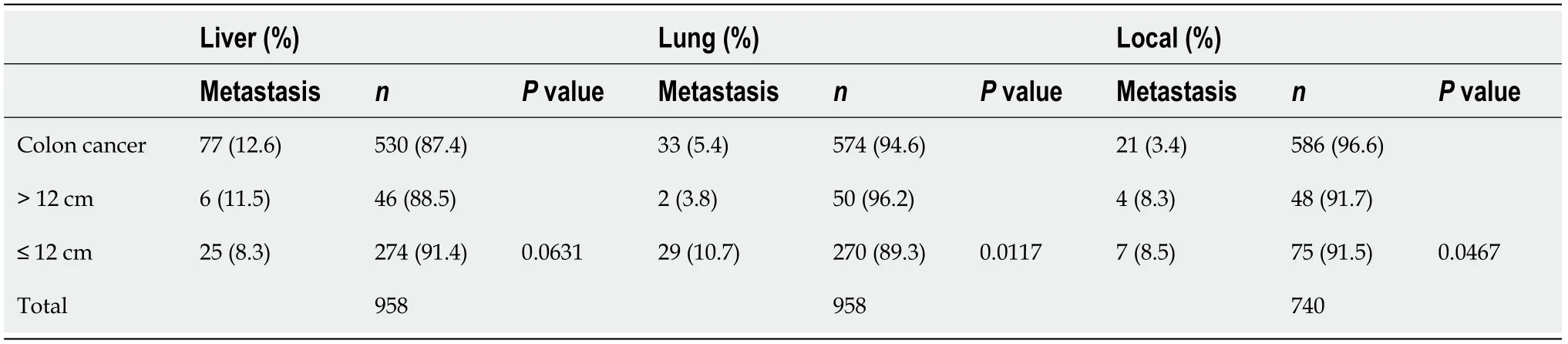
Table 4 Recurrence pattern according to National Comprehensive Cancer Network and American Joint Committee on Cancer guidelines

Table 5 Recurrence pattern according to European Society for Medical Oncology guidelines
The rates of liver metastasis, lung metastasis, and LR in rectal cancer located 11 cm to 15 cm from the anal verge were 6.9%, 2.8%, and 5.7%, respectively. There was no significant association with the liver metastasis, lung metastasis, and LR rates of colon cancer (P= 0.1714,P= 0.3357, andP= 0.3400, respectively).
DISCUSSION
Lung metastases and LR were more common in rectal cancer than in colon cancer, and TME is performed for rectal cancer as a common operative method to reduce LR[14-16]. Furthermore, although therapeutic strategies for colon cancer are standardized worldwide, those for rectal cancer vary from CRT and LLND to post-CRT watch and wait. Among these treatments, the indications for CRT are notably different between classification systems; while the NCCN and AJCC guidelines recommend this procedure for advanced rectal cancer located ≤ 12 cm from the anal verge, the ESMO guidelines recommend it for advanced rectal cancer ≤ 10 cm from the anal verge, and the JCCR guidelines only make a weak recommendation in cancers that are T3 or deeper or are cN+ with a high risk of LR. In addition, the localization of the lesion for this recommendation is not specified[3-6].
This study compared the recurrence type of rectal cancer according to various diagnostic criteria.
Approximately 26.6% of the tumors diagnosed as RS were located between 6 cm and 10 cm from the anal verge. They likely include more mid- and low rectal cancers that should be treated with CRT rather than tumors classified according to other guidelines. However, according to our current findings, the LR rates of RS cancers and rectal cancers considered “high rectal” cancers (i.e.those located more orally than 12 cm, 10 cm from the anal verge) after surgical monotherapy were 5.7%, 8.3% and 5.7%, respectively. These results were similar to the results for colon cancer. There was no significant difference in the recurrence type between RS and colon cancers. In light of its characteristic recurrence types (i.e.LR and lung metastasis), rectal cancer can be treated similarly to high rectal and colon cancers as presented by other guidelines. This suggests that the Japanese convention is as reliable as its Western counterparts.
The LR rates of RS cancers, tumors located ≤ 12 cm from the anal verge, and those located ≤ 10 cm from the anal verge after surgical monotherapy were 17.2%, 8.5% and 13.2%, respectively. These results were significantly higher than those for colon cancer (P =0.0002,P= 0.0467, andP= 0.0010). However, the LR rate of rectal cancers decreased to 5.5% when CRT was added. This value is equivalent to the recurrence rate of colon cancer. Unlike other guidelines, the JCCRC criteria classify rectal cancers according to the location of the tumor relative to the sacrum and the peritoneal reflection[3]. A large proportion of Rb rectal cancers are defined as tumors located below the peritoneal reflection. Measurements performed in this study according to these guidelines showed that 84.6% of Rb cancers were located within 0 cm to 5 cm of the peritoneal reflection. However, Najarianet al[17] reported that the mean distance between the anal verge and the peritoneal reflection was 9.7 cm in men and 9.0 cm in women. Although differences in the relationships between peritoneal reflection locations and Ra cancer and Rb cancers are possible, the findings of our investigation on recurrence types generally seemed to suggest that Ra cancer and Rb cancers had higher local recurrence rates according to the JCCRC guidelines than according to other guidelines. In addition, this study found that this diagnosis should be considered valid for caution in rectal cancer. In terms of therapeutic modalities, the findings of this study showed that in Western countries, nCRT is administered for the majority of tumors located below the peritoneal reflection, whereas in Japan, LLND is only performed for tumors diagnosed as Rb. This suggests that tumors diagnosed as Ra may include tumors for which LLND should be performed, assuming that CRT and LLND are performed as treatments for local control.
In conclusion, based on recurrence types, rectal cancers diagnosed as RS according to the JCCRC guidelines can be treated as colon cancer in terms of therapeutic strategies, similar to other guidelines. Rectal cancers diagnosed as Ra and Rb generally correspond to rectal cancer as defined by the NCCN and AJCC guidelines and to mid-rectal and low rectal cancer as defined by the ESMO guidelines. However, the retrospective, single-center design is a limitation of this study, and further research of patients in a multi-center study is warranted for more detailed investigations.
CONCLUSION
Our findings suggest that rectal cancers classified as RS under the JCCRC guidelines and rectal cancers classified as high rectal cancer under ESMO guidelines can be treated in the same way as colon cancer. The recurrence types of various lesions that require treatment as rectal cancer under the different guidelines were generally consistent; no major differences were found.
ARTICLE HIGHLIGHTS
Research background
Rectal cancer is characterized by more local recurrence and lung metastasis than colon cancer. However, the diagnosis of rectal cancer is not standardized as there is no global consensus on its definition and classification. The classification of rectal cancer differs between Japanese and Western guidelines.
Research motivation
To clarify the characteristics of rectal cancer by comparing the tumor location and characteristics of rectal cancer with those of colon cancer according to each set.
Research objectives
To make the management of rectal cancer a common understanding and to help determine the optimal treatment strategy. To that end, each guideline was compared.
Research methods
A total of 958 patients with Stage II and III colorectal cancer were included in the analysis: 607 with colon cancer and 351 with rectal cancer. Localization of rectal cancers was assessed by enema examination and rigid endoscopy.
Research results
Rectal cancer, which is indicated for chemoradiotherapy in the Western country, is consistent with middle-lower rectal cancer in Japan, and the recurrence rate was characterized by local recurrence and lung metastasis more than colon cancer.
Research conclusions
High rectal cancer may be treated with the same treatment strategies as colon cancer. There was no difference in the classification of colorectal cancer between Japan and Western countries.
Research perspectives
Chemoradiotherapy and lateral lymph node dissection are available for rectal cancer. Although many studies are being conducted around the world, clarifying the correct diagnosis will help in selecting the optimal treatment.
FOOTNOTES
Author contributions:Miyakita H designed the research; Miakita H and Chan LF performed the research; Miyakita H and Kamei Y contributed new reagents/analytic tools; Miyakita H, Okada K and Kayano H analyzed the data; Miyakita H and Yamamoto S wrote the paper.
Institutional review board statement:Approval code issued by the institutional review board: 20R-238 Tokai University.
Informed consent statement:Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement:All authors have no conflict of interest to declare in association with this study.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Japan
ORCID number:Hiroshi Miyakita 0000-0001-6541-2944; Hajime Kayano 0000-0002-8304-1136.
Corresponding Author's Membership in Professional Societies:The Japanese Society of Gastroenterological Surgery,G0351969.
S-Editor:Wang LL
L-Editor:Filipodia
P-Editor:Wang LL
 World Journal of Clinical Cases2022年36期
World Journal of Clinical Cases2022年36期
- World Journal of Clinical Cases的其它文章
- Liver injury in COVID-19: Holds ferritinophagy-mediated ferroptosis accountable
- Amebic liver abscess by Entamoeba histolytica
- Living with liver disease in the era of COVID-19-the impact of the epidemic and the threat to high-risk populations
- Cortical bone trajectory screws in the treatment of lumbar degenerative disc disease in patients with osteoporosis
- Probiotics for preventing gestational diabetes in overweight or obese pregnant women: A review
- Effectiveness of microwave endometrial ablation combined with hysteroscopic transcervical resection in treating submucous uterine myomas
