Analysis of the clinical efficacy of two-stage revision surgery in the treatment of periprosthetic joint infection in the knee: A retrospective study
Yong-Jie Qiao, Feng Li, Lv-Dan Zhang, Xin-Yuan Yu, Hao-Qiang Zhang, Wen-Bin Yang, Xiao-Yang Song, Rui-Ling Xu, Sheng-Hu Zhou
Yong-Jie Qiao, Xin-Yuan Yu, Hao-Qiang Zhang, Wen-Bin Yang, Xiao-Yang Song, Rui-Ling Xu,Sheng-Hu Zhou, Department of Joint Surgery, The 940th Hospital of Joint Logistic Support Force of Chinese People’s Liberation Army, Lanzhou 730050, Gansu Province, China
Feng Li, Department of Orthopedics, The 943rd Hospital of Joint Logistic Support Force of Chinese People’s Liberation Army, Wuwei 733000, Gansu Province, China
Lv-Dan Zhang, Department of Respiratory Medicine, The 940th Hospital of Joint Logistic Support Force of Chinese People’s Liberation Army, Lanzhou 730050, Gansu Province, China
Abstract BACKGROUND Periprosthetic joint infection (PJI) is a catastrophic complication that can occur following total knee arthroplasty (TKA). Currently, the treatment for PJI mainly includes the use of antibiotics alone, prosthetic debridement lavage, primary revision, secondary revision, joint fusion, amputation, etc.AIM To explore the clinical effect of two-stage revision surgery for the treatment of PJI after TKA.METHODS The clinical data of 27 patients (3 males and 24 females; age range, 47–80 years; mean age, 66.7 ± 8.0 years; 27 knees) with PJI treated with two-stage revision surgery in our hospital between January 1, 2010 and December 31, 2020 were analyzed retrospectively. The following outcomes were compared for changes between preoperative and last follow-up results: Erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), visual analogue scale (VAS) scores, Hospital for Special Surgery (HSS) scores, knee range of motion (ROM), and infection cure rates.RESULTS All 27 patients were followed up (range, 13–112 mo). The ESR (14.5 ± 6.3 mm/h) and CRP (0.6 ± 0.4 mg/dL) of the patients at the last follow-up were significantly lower than those at admission; the difference was statistically significant (P < 0.001). The postoperative VAS score (1.1 ± 0.7), HSS score (82.3 ± 7.1), and knee ROM (108.0° ± 19.7°) were significantly improved compared with those before the surgery; the difference was statistically significant (P < 0.001). Of the 27 patients, 26 were cured of the infection, whereas 1 case had an infection recurrence; the infection control rate was 96.3%.CONCLUSION Two-stage revision surgery can effectively relieve pain, control infection, and retain good joint function in the treatment of PJI after TKA.
Key Words: Total knee arthroplasty; Periprosthetic joint infection; Two-stage; Revision; Antibiotic therapy
INTRODUCTION
Periprosthetic joint infection (PJI) is a catastrophic complication after total knee arthroplasty (TKA), with an incidence of approximately 2% after primary TKA[1]. PJI can be classified as early (occurring within 3 mo after surgery), delayed (3–24 mo after surgery), and late (2 years after surgery)[2]. Currently, the treatment for PJI primarily includes the use of antibiotics alone, prosthetic debridement lavage, primary revision, secondary revision, joint fusion, amputation,etc.[3,4]. Tsukayamet al[5] grouped PJIs into four types and proposed corresponding treatment strategies: Type Ⅰ, no symptoms of infection but with positive intraoperative culture, mostly observed in preoperative diagnosis of aseptic loosening of the knee prosthesis and positive culture of the tissue specimen during revision surgery, which can be treated with intravenous antibiotics; type II, an early infection that occurs within 1 mo after surgery and can be treated by debridement to preserve the prosthesis; type III, an acute hematogenous infection that occurs suddenly in a well-functioning joint, which can also be treated, and the prosthesis is preserved; type IV, an advanced chronic infection that requires removal and revision of the prosthesis. PJI staging is the most widely used staging method and provides guidance on when to retain the prosthesis. Onestage revision leads to short hospitalization time, requires minimal cost, and has low impact on joint function[6]. However, its use is controversial because of the associated high recurrence rate of postoperative infection, and its effectiveness needs to be further explored[7]. Second-stage revision requires multiple surgeries and has the disadvantages of long hospital stay, increased costs, and impaired joint function, but it is effective and remains the gold standard of PJI treatment[8-10]. This study aimed to retrospectively analyze 27 patients with PJI who were treated with one-stage debridement, implant removal, antibiotic bone cement spacer exclusion, and two-stage revision and compare their preoperative and follow-up results.
MATERIALS AND METHODS
Inclusion and exclusion criteria
The inclusion criteria were as follows: Patients with PJI treated for the first time after TKA between January 1, 2010, and December 31, 2020; a diagnosis of PJI that conforms to the diagnosis standard set by of the International Consensus Group on Periprosthetic Joint Infection in 2014[11]; patients able to tolerate surgery; provision of informed consent for one-stage debridement, implant removal, antibiotic bone cement spacer exclusion, and two-stage revision; with complete follow-up data.
Patients with previous revision surgery due to infectious or non-infectious causes, those with termination of treatment using antibiotic bone cement spacer, those who were under anti-infection treatment for another infection site, and those lost to follow-up were excluded.
General information
We retrospectively analyzed the clinical data of 27 patients (3 males and 24 females; age range, 47–80 years; mean age, 66.7 ± 8.0 years; 27 knees) with PJI who were treated with phase I absences and phase II revisions from January 1, 2010, to December 31, 2020, at our hospital. There were 15 and 12 PJI cases in the right and left knees, respectively. There were 16 initial TKA cases recorded in our hospital and 11 cases from an outside hospital. The primary disease was osteoarthritis of the knee in 20 cases and rheumatoid arthritis in 7 cases. In all the cases, postoperative pathology was suggestive of acute/chronic septic inflammation. The surgery for all the cases was performed by the same team of surgeons.
Surgical methods
Surgery was performed under general anesthesia or combined lumbar epidural anesthesia, and the skin around the knee was cleaned thoroughly with a soft brush dipped in soap and water placed under the table. The surgical incision site was disinfected according to the infected area, the incision was made layer by layer along the original incision, the necrotic tissue and pus were cleared from outside to inside the infection site, any encountered sinus was completely removed, the joint capsule was opened to reveal the prosthesis, and the joint capsule, membranous tissue on the surface of the prosthesis, prosthesis, and bone cement were removed. At least three points of the interface granulation tissue and any other abnormal or septic tissue were sampled for bacterial culture and rapid frozen pathological and postoperative pathological examinations. The joint capsule, synovium, and diseased bone tissue were debrided thoroughly, and the surrounding tissue was completely excised. The bone cement was thoroughly cleaned after the prosthesis and pad were removed, and the remaining diseased tissue of the posterior joint capsule was completely excised again. The joint cavity was rinsed at least three times with hydrogen peroxide, dilute iodophor, and saline, with a liquid volume of more than 5000 mL, and the joint cavity was soaked with concentrated iodophor for at least 15 min and finally rinsed thoroughly with a large amount of saline using a pulse gun. The surgical gown, sterile gloves, and surgical instruments were changed for the next phase of the surgery. Depending on the size of the joint space after the prosthesis had been removed, an antibiotic cemented spacer of appropriate size was handmade (40 g of bone cement + 4 g of vancomycin, vancomycin-resistant, or specific pathogenic bacteria; antibiotics were added according to drug sensitivity results). Two groups of flushing and drainage tubes were left in place, and 4000 mL of saline/24 h of continuous drainage was administered after the surgery. Drainage fluid was collected and sent for culturing three times after 5–7 postoperative days, and the drainage tubes were removed after negative results were obtained.
For the reexamination of the erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and routine blood culture to monitor infection control regularly, exclusion for 3–6 mo is generally recommended, and three normal consecutive reexamination results are required for the second revision surgery to be performed. The bone and soft tissue are carefully explored, and three different parts of the soft tissue are sampled for rapid frozen pathological examination to assess the infection control. If the high magnification field was still greater than 10 neutrophils, thorough debridement and reinsertion of a new antibiotic bone cement placeholder is repeated. If the infection was completely controlled, the appropriate knee revision prosthesis was selected according to the degree of bone defect, bone quality, and stability of the collateral ligament, metal pad, and extension rod.
Postoperative management
For pain management, advanced, individualized, and multi-mode analgesia was used. For thrombosis prevention, 5000 IU of low molecular weight heparin calcium was injected subcutaneously once a day. For functional exercise, isometric and isotonic exercises of the quadriceps muscle, ankle pump exercises, and other functional exercise were performed as soon as possible after the administration of postoperative analgesia, and the exercise routine was gradually transitioned to active and passive functional exercises of the affected joints. For drainage, continuous knee cavity lavage was performed for 7–10 d after the first-stage spacer exclusion using 4000 mL of normal saline solution every day. Drainage fluid was tested by routine bacterial culture for 3 consecutive days from the 7thpostoperative day, and the flushing and drainage tubes were removed after all the results were negative. Based on the drainage condition, the drainage tube should be removed within 48 h after the two-stage revision.
Antibiotic application
The preoperative puncture fluid, intraoperative pus, necrotic tissue, and postoperative drainage fluid were all subjected to bacterial culture and drug sensitivity tests, and corresponding antibiotics were selected according to the drug sensitivity results. During the results waiting period or when the culture results are negative, empirical antibiotics should be administered for treatment, and broad-spectrum antibiotics should also be selected administered to treat most gram-negative and gram-positive bacterial infections. After first-stage exclusion, an adequate amount of sensitive antibiotics was administered intravenously for 2 wk (if the culture result was negative, intravenous vancomycin combined with third-generation cephalosporins or quinolones and other antibiotics was administered); oral sensitive antibiotics was also administered for 4 wk after the 2 wk (if the culture result was negative, oral rifampicin + ciprofloxacin were administered), and the decision to stop or extend the antibiotics (intravenous + oral sensitive antibiotics) < 6 wk of the drug course was based on a patient’s condition. The initial intravenous antibiotic regimen was continued after second-stage revision until the intraoperative culture results were clear or stopped if the results were negative; treatment was continued according to new PJI if there were 2 or more positive results.
Evaluation indicators
ESR, CRP, visual analogue scale (VAS) score, Hospital for Special Surgery (HSS) score, range of motion (ROM), and infection control rate were recorded before the surgery and at the last follow-up. Infection control was defined as the absence of infection recurrence and prosthesis loosening after revision and follow-up. ESR and CRP were used to evaluate infection control, and pain VAS score, HSS score, and ROM were used to evaluate symptom improvement and recovery of knee function. Two years after the surgery, radiographic images were reviewed to determine whether the prosthesis was loose.
Statistical analysis
SPSS version 23.0 (IBM, Chicago, IL, United States) was used to analyze the data. ESR, CRP, VAS score, HSS score, and ROM were all expressed as mean ± SD. Paired sample t test was used to compare the results obtained before surgery and at last follow-up, andP< 0.05 was considered to be statistically significant.
RESULTS
Analysis of evaluation indicators
All 27 patients were followed up for 13–112 mo (average, 59 ± 26 mo). Twenty-six patients were cured of the infection, and 1 patient had recurrence after 6 years of follow-up, with an infection control rate of 96.3%. The time between the initial joint replacement and the diagnosis of PJI ranged from 7 to 195 mo (mean, 41 ± 35 mo), with 9 cases (33.3%) of delayed PJI and 18 cases (66.7%) of advanced PJI. The duration of spacer exclusion was 2.8–6.3 mo (mean, 3.8 ± 0.8 mo). Positive bacterial culture results were obtained in 17 of the 27 patients (Table 1), with a positive rate of 63.0%, including 13 g-positive bacterial infection [8 cases ofStaphylococcus aureus, 2 cases of methicillin-resistantS. aureus(MRSA), 2 cases ofStaphylococcus epidermidis, and 1 case ofStreptococcus griseus], 3 g-negative bacterial infection (2 cases ofEnterobacter cloacae, 1 case ofPseudomonas aeruginosa), and 1 case of fungal infection (Candida). An articulating spacer was used in all 27 patients. All 27 patients with the following types of prosthesis underwent revision surgery: Surface knee prosthesis (3 cases), Legacy®(Zimmer Biomet, Warsaw, IN, United States) constrained condylar knee (LCCK) prosthesis (20 cases), and rotating hinge (RH) knee prosthesis (4 cases). The ESR (14.5 ± 6.3 mm/h) and CRP (0.6 ± 0.4 mg/dL) levels at the last follow-up were significantly (P< 0.001) lower than those obtained preoperatively (ESR, 57.1 ± 21.8 mm/h; CRP, 2.9 ± 2.1 mg/dL), and this difference was statistically significant (Table 2). The patients’ VAS score (1.1 ± 0.7), HSS score (82.3 ± 7.1), and knee ROM (108.0° ± 19.7°) at the last follow-up improved significantly (P< 0.001) compared with the preoperative scores (VAS, 4.0 ± 0.8; HSS score, 57.9 ± 9.4; knee ROM, 91.9° ± 26.9°) (Table 3).
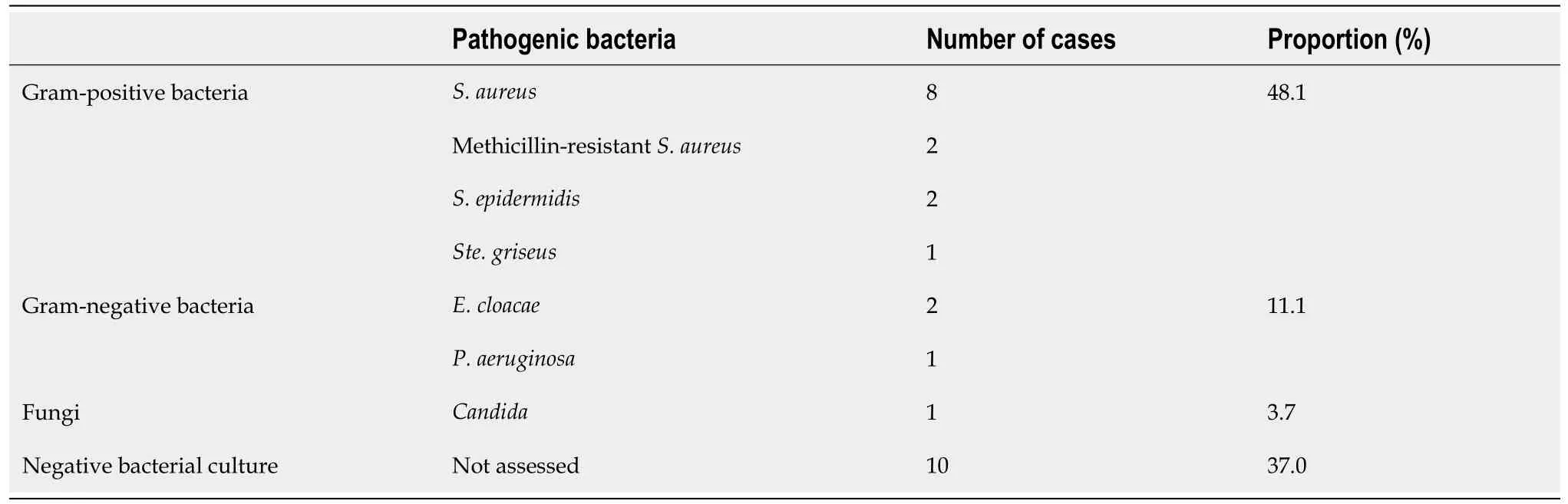
Table 1 Pathogenetic results of periprosthetic joint infection after total knee arthroplasty in 27 cases
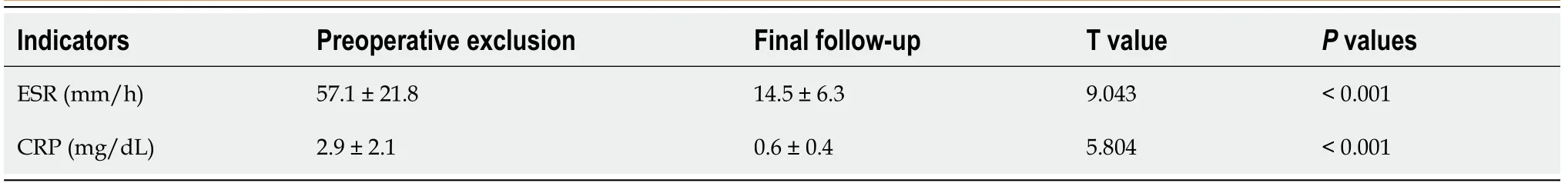
Table 2 Comparison of preoperative and final follow-up erythrocyte sedimentation rate and C-reactive protein results
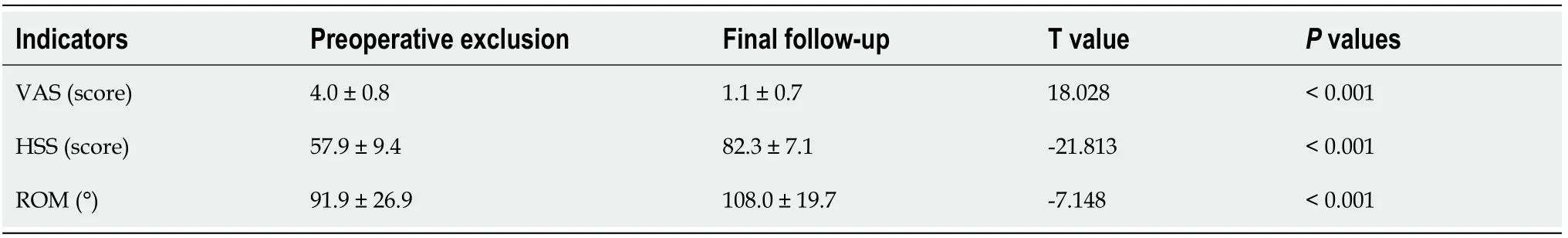
Table 3 Comparison of preoperative and final follow-up knee pain visual analogue scale scores, hospital for special surgery scores,and range of motion results
Typical case 1
The patient was a 78-year-old woman whose primary disease was left knee osteoarthritis (Kellgren-Lawrence stage VI). More than 4 years after the left TKA was performed in another hospital, her left knee joint became swollen and painful with limited movement for more than 6 mo, and there was sinus tract formation and secretion discharge for 2 mo (Figure 1). After admission, the bacterial culture of the knee joint puncture showed MRSA. Drug sensitivity test showed sensitivity to vancomycin and rifampin. After ensuring no contraindications to surgery, lumbar anesthesia was administered for onestage debridement, implant removal, and antibiotic bone cement spacer exclusion (Figure 2). Postoperative intravenous vancomycin (1 g, twice a day) was administered for 2 wk. After discharge, rifampicin capsule (0.45 g, once a day) and ciprofloxacin hydrochloride capsule (0.5 g, twice a day) were taken orally for 6 wk; the exclusion time was 4 mo. After three consecutive routine blood examinations, ESR and CRP were normal, and knee arthroplasty was performed in the second stage of the treatment (Figure 3).
Typical case 2
Case 2 was a 51-year-old woman with rheumatoid arthritis of the right knee, which occurred more than 6 years after right TKA (Figure 4). The patient’s chief complaints were right knee swelling and pain with limited movement for 6 mo. Negative bacterial culture results were obtained throughout the treatment, and pathological examination showed chronic purulent inflammation. After ensuring no contraindications to surgery, lumbar anesthesia was administered for stage debridement, implant removal, and antibiotic bone cement spacer exclusion. Postoperative intravenous vancomycin (1 g, twice a day) combined with cefoperazone sulbactam sodium (3 g, twice a day) was administered for 2 wk. After discharge from the hospital, the patient had to take oral rifampin (0.45 g, once a day) and ciprofloxacin (0.5 g, twice a day) for 6 wk, with an exclusion time of 4.8 mo. Three consecutive routine blood examinations revealed that the ESR and CRP were normal on all three instances. Knee arthroplasty was then performed in the second stage of the treatment.
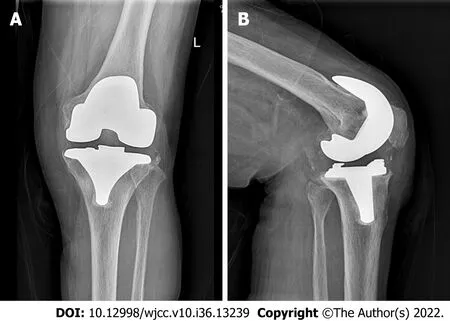
Figure 1 A 78-year-old female patient with periprosthetic joint infection after left knee arthroplasty. Radiographic image of the left knee joint showing good position of the prosthesis without significant loosening. A: Anteroposterior; B: Lateral.

Figure 2 A 78-year-old female patient after one-stage debridement, implant removal, and antibiotic bone cement spacer exclusion. A:Appearance of the infected skin around the prosthesis after left knee arthroplasty with sinus canal formation; B: Complete debridement after prosthesis removal; C:After the placement of antibiotic bone cement placeholders, the space is moderate; D and E: Radiographic images of the left knee after exclusion: Anteroposterior (D)and lateral (E); F: Pathology showing chronic suppurative inflammation.

Figure 3 Radiographic image of the left knee of a 78-year-old female patient after phase II revision. A and B: Radiographic images of the left knee after revision: Anteroposterior (A) and latera (B); C: Full-length orthotopic position of the lower limbs after revision; D and E: Radiographic images of the left knee 2 yr after revision: Anteroposterior (D) and lateral (E).

Figure 4 A 51-year-old female patient with periprosthetic joint infection after right knee arthroplasty. A and B: Radiographic images of the right knee arthroplasty: Anteroposterior (A) and lateral (B); C and D: Radiographic images of the right knee after exclusion: Anteroposterior (C) and lateral (D); E and F:Radiographic images of the right knee after revision surgery: Anteroposterior (E) and lateral (F); G and H: Radiographic images of the right knee 2 yr after revision:Anteroposterior (G) and lateral (H).
DISCUSSION
As one of the most serious complications of TKA, PJI is characterized by difficult treatment, long treatment period, high recurrence rate, and high disability rate. Different treatments have been reported in recent years. Prosthetic knee revision, including primary and secondary revision, is one of the basic treatment options for PJI. Currently, second-stage revision is the gold standard for PJI treatment[12], and the cure rate varies greatly among different joint centers. In the present study, we retrospectively analyzed 27 patients with PJI that was diagnosed and treated in our hospital. The infection control rate of the second-stage revision was 96.3%, and the success rate of treatment was significantly higher than that reported in previous studies[13,14].
According to the bacterial biofilm formation theory proposed by Costerton[15], bacteria adhere to the surface of prosthesis and secrete polysaccharide, fibrin, lipoprotein, and other substances to form a multi-membrane structure called biofilm. The bacterial biofilm forms irreversible changes in approximately 3 wk, and it can resist human immunity and the effects of antibiotics. Therefore, the application of antibiotics alone cannot completely eradicate the infection around the joint. The formation of biofilm is the main reason for the difficulty in the late treatment of PJI. Radical treatment of PJI requires removal of the entire prosthesis and intensive debridement to the point of complete exposure. Mechanical operation should be performed to remove the biofilm, which is very important for infection control and is the primary factor for successful surgical outcome[3,16,17]. Debridement should not be forceful, and soft tissue injury and bone defect around the joint should be minimized as much as possible. Soft tissue injury of the skin has a significant influence on wound healing in the first stage, and collateral ligament injury and bone defect increase the difficulty of second-stage revision. Correct application of antibiotics plays a crucial role in the prognosis of PJI. After identifying the pathogenic bacteria and determining drug sensitivity through bacterial culture, selecting a sufficient amount and appropriate course of sensitive antibiotics can improve outcomes. A previous study reported that the main pathogenic bacteria of PJI are gram-positive bacteria such asS. epidermidisandS. aureus, which are basically sensitive to vancomycin[18]. PJI with negative bacterial culture is called refractory PJI and is common in the clinic. In this study, the failure rate of bacterial culture was 37% (10/27), which is approximately equivalent to the rate (20%–50%) reported in the literature[19]. Negative bacterial cultures make the diagnosis of and antibiotic selection for PJI difficult. The main reason for the low pathogen detection rate may be that the patient has been empirically treated with antibiotics before the specimens were obtained[20]. Therefore, it is important to seek effective methods to improve the positive rate of bacterial culture. Emergence of metal-artifact-free magnetic resonance imaging technology, polymerase chain reaction technology, ultrasonic pyrolysis, mass spectrometry analysis, second-generation sequencing, and other technologies[4,21-23] has made identification of pathogens relatively easy. However, with the widespread application and even abuse of antibiotics, the incidence of drug-resistant bacteria, such as MRSA, is increasing, and the treatment is difficult and requires a prolonged cycle. Fungi detected in PJI are extremely rare, accounting for approximately 1%–2%. The diagnosis of fungal PJI is very difficult, and negative bacterial cultures do not rule out fungi as the cause of PJI; therefore, treatment is also extremely challenging[24].
The application of antibiotic bone cement spacer is an important step in second-stage revision. Spacers are classified as non-jointed (stationary) and jointed (mobile). Spacer, made with a ratio of 40 g bone cement to 4 g vancomycin, sustainably releases high concentrations of antibiotics locally to control infection. Individually made articular spacers can appropriately maintain the knee space and lateral collateral ligament tension, effectively prevent soft tissue contracture around the prosthesis, and maximally preserve knee function, which is convenient for the second-stage revision exposure of the surgical field and the recovery of postoperative joint function[25-27]. Studies have shown that 3Dprinted articular spacers can provide satisfactory ROM during the spacer exclusion period, prevent bone loss, and reduce the rate of infection and complications[28]. At present, there is no unified standard for the duration of the exclusion period. If the exclusion period is too long, the overall treatment time is prolonged and treatment cost is increased, which is not conducive to knee joint function. Spacer poses the risk of wear, dislocation, and fracture; the infection might not clear within an extremely short exclusion period, and there is a risk of infection recurrence. Our hospital recommends an interval of 3–6 mo between the first and second surgeries, and the knee joint should be normal during the open period. If the patient's general condition is stable, the incision is adequately healed, without symptoms of infection (such as swelling, heat, and pain), and three consecutive routine blood examination results of CRP and ESR are normal, the second revision can be performed. If signs of infection are identified during the surgery, the revision should be abandoned, and debridement and exclusion should be performed again.
Correct selection of revision prosthesis is the key to the success of the second phase of knee revision[29]. Ensuring prosthesis stability and maintaining joint stability are the basic principles for the selection of revision prosthesis. Because of bone defects, injury or loss of collateral ligaments, and other reasons, a special prosthesis system is often required for the second phase of knee revision. The ultimate goal of second-stage revision is to eradicate infection and rebuild a painless, functional, and stable knee. On the premise of achieving soft tissue balance and optimal joint stability, knee prosthesis with less limitation should be selected as much as possible. In the case of good bone structure and mild bone defect, the use of a prosthesis with less limitation can lead to effective load sharing in surrounding soft tissues, reduce prosthesis wear and loosening, and improve the success rate of revision[30]. When the bone structure is poor, the bone defect is obvious, and the stability of the prosthesis is poor. The stress on the contact surface of the prosthesis can be dispersed maximally to the pulp cavity using the extender rod and spacer to increase the stability of the prosthesis. In the case of collateral ligament insufficiency, the LCCK prosthesis not only provides anterior-posterior stability but also controls the balance between varus and varus, partially compensating for the collateral ligament function. RH prosthesis should be used in cases of severe lateral collateral ligament dysfunction combined with severe bone defects or complete loss of stability of the knee joint. RH prosthesis has good internal stability and does not require balancing of soft tissues. A large prosthesis module can replace bone defects, and a long handle can disperse the interface stress of the prosthesis.
This study has some limitations. This is a retrospective study with a relatively small sample size. It is not a multicenter study with a large sample or a randomized controlled trial. Some patients had negative bacterial cultures, and antibiotic use was mainly empirical. The reliability and accuracy of the study should be further confirmed in future studies with large samples.
CONCLUSION
The two-stage revision surgery approach, which includes the first stage of thorough debridement, removal of prosthesis, antibiotic bone cement placeholder exclusion for 3–6 mo, three normal consecutive routine blood examination results for ESR and CRP, selection of a suitable prosthesis for the second-stage revision, and the use of a sufficient amount of a full course of sensitive antibiotics, is a reliable method for the treatment of PJI after TKA. This approach can effectively relieve pain, control infection, and preserve good joint function.
ARTICLE HIGHLIGHTS
Research background
Periprosthetic joint infection (PJI) is a catastrophic complication after total knee arthroplasty (TKA).
Research motivation
This study aimed to retrospectively analyze 27 patients with PJI who were treated with one-stage debridement, implant removal, antibiotic bone cement spacer exclusion, and two-stage revision and compare their preoperative and follow-up results.
Research objectives
This study aimed to explore the clinical effect of one-stage debridement, implant removal, antibiotic bone cement spacer exclusion, and two-stage revision in the treatment of PJI after TKA.
Research methods
Of 27 patients with PJI treated with two-stage revision surgery were analyzed retrospectively. The following outcomes were compared for changes between preoperative and last follow-up results: Erythrocyte sedimentation rate, C-reactive protein, visual analogue scale scores, Hospital for Special Surgery scores, knee range of motion, and infection cure rates.
Research results
Of the 27 patients, 26 were cured of the infection, whereas 1 case had an infection recurrence; the infection control rate was 96.3%.
Research conclusions
Two-stage revision surgery can effectively relieve pain, control infection, and retain good joint function in the treatment of PJI after TKA.
Research perspectives
Whether the PJI can be cured using the one-stage debridement, implant removal, antibiotic bone cement spacer exclusion, and two-stage revision.
FOOTNOTES
Author contributions:Qiao YJ, Li F and Zhang LD contributed equally to this work; Qiao YJ, Li F and Zhang LD designed the study, collected data, performed the statistical analysis, and wrote the manuscript; Zhang HQ and Yu XY assisted with data collection; Yang WB drafted the manuscript; Zhang HQ and Song XY helped with data interpretation and critically reviewed the manuscript; Zhou SH conceived of the study, helped with data interpretation, and critically reviewed the manuscript; All the authors read and approved the final manuscript.
Institutional review board statement:Formal institutional approval was not deemed necessary since anonymised data routinely collected in our centre for clinical practice purposes were used.
Informed consent statement:All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:Participants gave informed consent for data sharing.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Yong-Jie Qiao 0000-0001-7335-9020; Feng Li 0000-0002-0763-014X; Wen-Bin Yang 0000-0002-6680-4998;Sheng-Hu Zhou 0000-0002-4539-319X.
S-Editor:Fan JR
L-Editor:A
P-Editor:Fan JR
 World Journal of Clinical Cases2022年36期
World Journal of Clinical Cases2022年36期
- World Journal of Clinical Cases的其它文章
- Liver injury in COVID-19: Holds ferritinophagy-mediated ferroptosis accountable
- Amebic liver abscess by Entamoeba histolytica
- Living with liver disease in the era of COVID-19-the impact of the epidemic and the threat to high-risk populations
- Cortical bone trajectory screws in the treatment of lumbar degenerative disc disease in patients with osteoporosis
- Probiotics for preventing gestational diabetes in overweight or obese pregnant women: A review
- Effectiveness of microwave endometrial ablation combined with hysteroscopic transcervical resection in treating submucous uterine myomas
