Hoffa's fracture in a five-year-old child diagnosed and treated with the assistance of arthroscopy: A case report
Zhi-Hao Chen, Hai-Fan Wang, Hao-Yu Wang, Fei Li, Xue-Feng Bai, Jian-Long Ni, Zhi-Bin Shi
Zhi-Hao Chen, Hai-Fan Wang, Hao-Yu Wang, Fei Li, Jian-Long Ni, Zhi-Bin Shi, The First Department of Orthopaedics, The Second Affiliated Hospital of Xi’an Jiaotong University,Xi’an Jiaotong University, Xi'an 710004, Shaanxi Province, China
Xue-Feng Bai, Department of Orthopaedics, Xi’an Daxing Hospital, Xi'an 710016, Shaanxi Province, China
Abstract BACKGROUND Hoffa's fracture is a coronal-oriented fracture of the femoral condyle. It is rarely observed in pediatric patients that isolated coronal fracture of the medial femoral condyle accompanies an intact lateral femoral condyle. Only a few cases involving Hoffa's fracture of the medial femoral condyle have been reported in patients with undeveloped skeletons. Such a fracture cannot be observed by routine imaging examinations, thus resulting in possible misdiagnosis and further treatment challenges.CASE SUMMARY A 5-year-old boy with Hoffa's fracture of the medial femoral condyle suffered from right knee pain and severe swelling after being hit by a heavy object. The patient was misdiagnosed and initially treated in a local primary healthcare center. No improvement in his right knee’s extension was observed following conservative treatment for 2 wk. The patient was transferred to our hospital, rediagnosed using arthroscopy, and underwent open reduction and internal fixation. The therapeutic outcome was satisfactory with the screws removed 7 mo after fixation. At the final follow-up of 40 mo, the range of motion in the knee had recovered. There was no varus-valgus instability.CONCLUSION Hoffa's fracture is rarely seen in children aged 5 years, let alone in the medial condyle, and can easily be misdiagnosed due to limited physical and imaging examinations. Suspected Hoffa's fracture in preschool children should be confirmed based on arthroscopic findings. Open reduction and internal fixation should be performed to protect the articular surface and prevent long-term complications.
Key Words: Hoffa's fracture; Pediatrics; Medial femoral condyle; Missed diagnosis; Arthroscopy; Open reduction-internal fixation; Case report
INTRODUCTION
Hoffa's fracture, named after Albert Hoffa in 1904 following his detailed research on this disease[1], is an unusual fracture type on the coronal plane of the femoral condyle. Hoffa's fractures of the lateral femoral condyle are commonly seen, while Hoffa's fractures of the medial femoral condyle are rare, especially in individuals with undeveloped skeletons. The latest case was a 16-year-old girl with Hoffa's fracture of the medial femoral condyle reported by Jianget al[2] in 2022. This type of fracture is an intraarticular fracture and is clinically treated under the same principles as a typical intra-articular fracture. But this type of injury is often misdiagnosed due to a lack of clinical suspicion and radiographic examinations. In this report, we present the case of a 5-year-old boy with unusual type of injury misdiagnosed in a local hospital. Arthroscopy was performed to confirm the medial Hoffa's fracture. Later, open reduction and internal fixation were successfully applied to the patient for treatment.
CASE PRESENTATION
Chief complaints
A 5-year-old boy was transferred to the Department of Orthopedics in our hospital due to right knee pain and swelling, and an inability to bear weight and extend the right knee.
History of present illness
The patient had right knee pain and an inability to extend the knee following 2 weeks of conservative treatment.
History of past illness
The boy had no history of severe diseases, surgery or long-term medication.
Personal and family history
The patient’s family had no related diseases.
Physical examination
His right knee was swollen, skin was intact with tenderness on palpation, and limited mobility. No distal neurovascular deficits were observed. He was alert, articulate, and a reliable reporter. No other weakness, stiffness, or edema was found.
Laboratory examinations
Results of laboratory examinations were unremarkable.
Imaging examinations
X-Ray showed a stable fracture in the medial femoral condyle with no displacement (Figure 1). A local orthopedist suggested conservative treatment. Computed tomography (CT) is considered efficient in the diagnosis of adult Hoffa's fracture. However, in this case, the thick cartilage of the distal femoral epiphyseal area made it difficult to evaluate the fracture[1,3,4]. The area of high signal on magnetic resonance imaging (MRI) also indicated no severe displacement (Figure 2).
FURTHER DIAGNOSTIC WORK-UP
Arthroscopy was performed to confirm the diagnosis. Different from the findings on the imaging examinations, obvious fracture displacement of the cartilage was found (Figure 3).
FINAL DIAGNOSIS
Hoffa's fracture of the medial femoral condyle.
TREATMENT
Arthroscopic exploration and diagnosis were performed at the beginning of the operation. The presence of steps and micromovement at the fracture ends could be seen during arthroscopy. However, due to instability of the bone mass caused by the now old injury (more than 2 wk), it was difficult to achieve a satisfactory reductionviaarthroscopy. Therefore, open reduction was scheduled (Figure 4). Two 3.0 mm partially-threaded cancellous screws placed perpendicular to the fracture line were used to reduce the fracture. To avoid epiphyseal injury, a screw of appropriate length was placed through the metaphysis. Countersunk screws were also placed through the articular cartilage.
OUTCOME AND FOLLOW-UP
Following open reduction and internal fixation, the patient wore a knee brace with 30° of knee flexion for approximately 2 wk. Afterwards, gradually begin to work on the range of motion of the knee. The patient was strictly instructed to avoid any weight-bearing bending until the sixth week, in order to minimize the shear force on his coronation. Partial weight-bearing began after the sixth week, then progressing to full weight-bearing (FWB) by the tenth week. At the six-month follow-up, he could walk without support. The knee range of motion was 5° to 100° (Figure 5). No angular deformity or limblength discrepancy was observed. X-ray showed that the fracture healed well and there was no sign of femoral condyle collapse (Figure 6). The screws were removed after 7 mo. At the final follow-up of 40 mo, the KSS score was 100. The patient had full range of motion, with no varus-valgus instability (Figure 7).

Figure 1 X-ray before surgery shows a stable fracture in the medial femoral condyle with no displacement. A: Anterior-posterior view of X-ray;B: Lateral view of X-ray.

Figure 2 Magnetic resonance imaging before surgery indicated no severe displacement. A: Sagittal slice of lateral condyle of femur; B: Most lateral slice of femoral intercondylar notch; C: Most medial slice of femoral intercondylar notch; D: Sagittal slice of medial condyle of femur.

Figure 3 Arthroscopy showed obvious fracture displacement of the cartilage.

Figure 4 The operation was completed using the medial parapatellar approach.
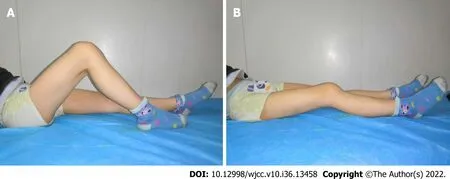
Figure 5 Six months after surgery, the range of motion of the knee joint reached 5°-100°. A: Maximum flexion position; B: Maximum extension position.
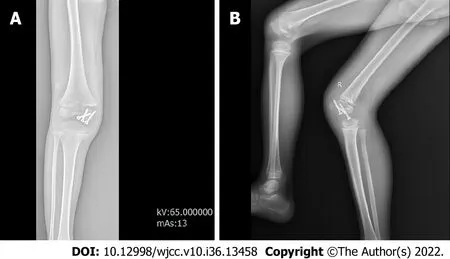
Figure 6 Plain radiographs showed a well-healed fracture with no evidence of collapse of the femoral condyle. A: Anterior-posterior view of Xray; B: Lateral view of X-ray.
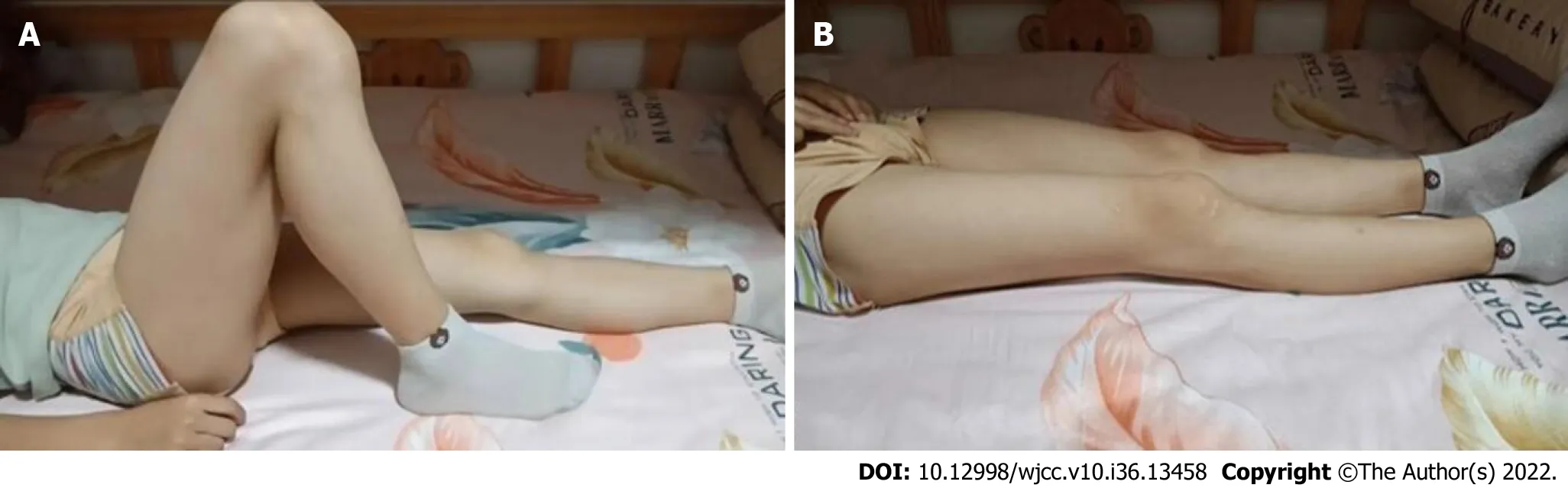
Figure 7 At the final follow-up of 40 months, the patient had full range of motion. A: Maximum flexion position; B: Maximum extension position
DISCUSSION
Coronal plane fracture of the femoral condyle was named after Hoffa following his detailed research on this fracture in 1904[3]. Letenneuret al[5] classified this fracture into three different types. Accordingly, our patient developed a Type III fracture. This rare injury can also be classified into a medial, lateral and conjoint Hoffa's fracture based on the location of the fracture[6]. According to a review of the literature on Hoffa’s fracture in the pediatric population (Table 1), 16 cases of Hoffa’s fracture in pediatric patients were reported. Only 5 were located on the medial femoral condyle. Baliet al[7] first described an isolated Hoffa's fracture of the medial condyle in a patient with an undeveloped skeleton. Ranjanet al[6] described a Hoffa’s fracture of the medial condyle in a 6-year-old girl. To date, only four cases of Hoffa’s fracture of the medial condyle in pediatric patients has been reported. We aimed to report the fifth case in a 5-year-old patient, the youngest ever diagnosed.
Hoffa’s fractures are mostly triggered by high-energy damage[8,9], and are more commonly seen in young adults. This injury is mainly caused by axial shear force affecting the posterior part of the femoral condyle when the knee is flexed[6]. Due to the anatomical features of the ectropion angle at the distal femur, when high-energy violence acts on the distal femur, it often acts firstly on the lateral condyle. As a result, lateral condyle fractures are more common than medial condyle fractures. Commonly, the cause of Hoffa's fractures in adults is vehicle accidents[7] while in pediatric Hoffa's fracture are usually caused by trivial injury or sports injury[10]. In this case, the injury was caused by a heavy object falling on the right knee. Since only a few cases have been reported, little is known about Hoffa's fractures in children, and McDonoughet al[11] reported the first case of a non-healing Hoffa's fracture in an eightyear-old boy. According to our research (Table 1), X-ray is the most effective diagnostic tool for confirming pediatric Hoffa’s fracture, followed by CT[12-14]. However, as the fracture is barely visible on routine anteroposterior radiographs, misdiagnosis often occurs even in the lateral view. The fracture can be obscured by the intact anterior condyle in the anterior and posterior projections, if it is minimally displaced[15-17]. Therefore, it is wiser to carry out the gold standard investigation, which is CT[18]. However, in pediatric patients, the fracture line can be easily ignored, even on CT and MRI due to thick cartilage. In young patients, the diagnosis of Hoffa’s fracture is often omitted based on past clinical experience. Three cases of misdiagnosed Hoffa’s fracture in eight-year-old and two twelve-year-old boys were identified in previous literature, which were fixed with cannulated screws and successfully treated[11,16,19]. In this study, we report another case of nonunion of Hoffa’s fracture in the medial condyle in a five-year-old boy who was initially misdiagnosed as having a stable fracture with no displacement. The patient was finally diagnosed with Hoffa’s fracture by arthroscopy. Therefore, it is noteworthy that arthroscopy is critical in the diagnosis of pediatric Hoffa’s fracture with inconclusive radiographs[10]. In our case, a CT scan was not performed on the injured knee due to difficulty in evaluating the fracture, thick cartilage of the distal femoral epiphysis and the patient’s immature skeleton[1,3,4]. Avoiding CT exams can also prevent greater radiation exposure during CT scans than Xrays[20].
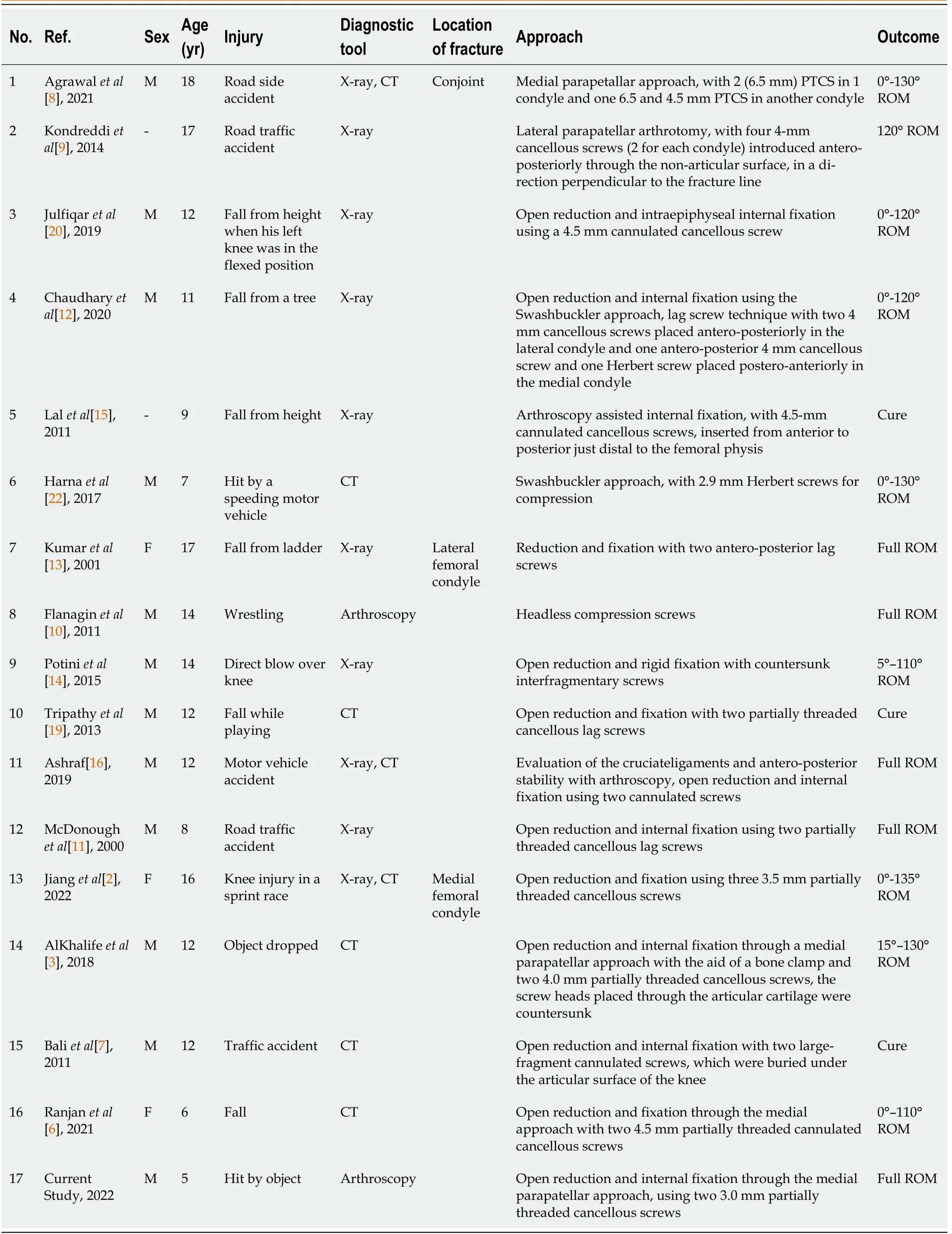
Table 1 Review of the literature on Hoffa’s fracture in the pediatric population
Conservative treatment of these fractures is unsatisfactory as the reduction in fracture fragments is difficult to achieve and to maintain by closure. This may lead to multiple complications such as avascular necrosis, nonunion, and malunion[4,15,21]. Therefore, as the ideal treatment[19], surgical stabilization and internal fixation are required to achieve a satisfactory clinical outcome. There is also controversy regarding the surgical approaches for pediatric Hoffa’s fracture. The approaches described in previous literature include the lateral, medial and Swashbuckler approach (Table 1). It is generally accepted that surgical stabilization is necessary for a satisfactory clinical outcome after the treatment of Hoffa’s fracture. The reason for this is that, closure reduction and cast/traction techniques are difficult to achieve and sustain the reduction of fracture fragments without soft tissue attachment. Therefore, this kind of injury is also prone to vascular necrosis and bone nonunion, which should be prevented by stable anatomical compression reduction and internal fixation. This can only be achieved by open/arthroscopic approaches[15]. In our case, we performed open reduction and internal fixation with the assistance of arthroscopy using a medial parapatellar approach. The outcome was satisfactory. The advantages of the guidance of arthroscopy include avoidance of soft tissue, decreased blood loss, and intraarticular visualization. Acute Hoffa’s fracture with minimal communition and large fragments can also get benefit from arthroscopic fixation[21,22].
CONCLUSION
We report Hoffa’s fracture of the medial condyle in a 5-year-old child, the youngest patient ever reported, who was diagnosed and treated with the assistance of arthroscopy. We maintain that this rare fracture can be misdiagnosed easily. Healthcare practitioners should note of this when dealing with children’s knee fractures. It is better to diagnose this fracture by arthroscopy in patients with skeletal immaturity. Treatment of this fracture with open reduction and internal fixation can prevent further long-term complications. However, arthroscopy-guided reduction and internal fixation may be a good option for patients who have a fresh fracture.
FOOTNOTES
Author contributions:Shi ZB provided this case and provided the relevant fund; Chen ZH and Wang HF drafted the majority of the manuscript; Wang HY, Li F, Bai XF and Ni JL collected all the materials; All authors have read and approved the final version.
Informed consent statement:Informed written consent was obtained from the patient.
Conflict-of-interest statement:All the authors declare that they have no conflict of interest.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Zhi-Hao Chen 0000-0002-7499-7507; Fei Li 0000-0002-7282-1938; Zhi-Bin Shi 0000-0002-4488-080X.
S-Editor:Liu JH
L-Editor:A
P-Editor:Liu JH
 World Journal of Clinical Cases2022年36期
World Journal of Clinical Cases2022年36期
- World Journal of Clinical Cases的其它文章
- Liver injury in COVID-19: Holds ferritinophagy-mediated ferroptosis accountable
- Amebic liver abscess by Entamoeba histolytica
- Living with liver disease in the era of COVID-19-the impact of the epidemic and the threat to high-risk populations
- Cortical bone trajectory screws in the treatment of lumbar degenerative disc disease in patients with osteoporosis
- Probiotics for preventing gestational diabetes in overweight or obese pregnant women: A review
- Effectiveness of microwave endometrial ablation combined with hysteroscopic transcervical resection in treating submucous uterine myomas
