Development of dilated cardiomyopathy with a long latent period followed by viral fulminant myocarditis: A case report
Seung Do Lee, Hyo Jin Lee, Hye Ree Kim, Min Gyu Kang, Kyehwan Kim, Jeong Rang Park
Seung Do Lee, Hyo Jin Lee, Hye Ree Kim, Min Gyu Kang, Kyehwan Kim, Jeong Rang Park,Division of Cardiology, Department of Internal Medicine, Gyeongsang National University School of Medicine and Gyeongsang National University Hospital, Jinju 52727, South Korea
Abstract BACKGROUND The clinical course of acute myocarditis ranges from the occurrence of a few symptoms to the development of fatal fulminant myocarditis. Specifically, fulminant myocarditis causes clinical deterioration very rapidly and aggressively. The long-term prognosis of myocarditis is varied, and it fully recovers without leaving any special complications. However, even after recovery, heart failure may occur and eventually progress to dilated cardiomyopathy (DCM), which causes serious left ventricular dysfunction. In the case of follow-up observation, no clear guidelines have been established.CASE SUMMARY We report the case of a 21-year-old woman who presented with dyspnea. She became hemodynamically unstable and showed sustained fatal arrhythmias with decreased heart function. She was clinically diagnosed with fulminant myocarditis based on her echocardiogram and cardiac magnetic resonance results. After 2 d, she was readmitted to the emergency department under cardiopulmonary resuscitation and received mechanical ventilation and extracorporeal membrane oxygenation. An implantable cardioverter defibrillator was inserted for secondary prevention. She recovered and was discharged. Prior to being hospitalized for sudden cardiac function decline and arrhythmia, she had been well for 7 years without any complications. She was finally diagnosed with dilated cardiomyopathy.CONCLUSION DCM may develop unexpectedly in patients who have been cured of acute fulminant myocarditis and have been stable with a long period of remission. Therefore, they should be carefully and regularly observed clinically throughout long-term follow-up.
Key Words: Myocarditis; Fulminant; Dilated cardiomyopathy; Outcome; Remission; Case report
INTRODUCTION
Myocarditis, an inflammation of the myocardium, is also defined as inflammatory cardiomyopathy characterized by worsening cardiac dysfunction and cardiac remodeling in terms of the size, shape, and structure of the heart[1]. Etiologies of acute myocarditis include various infections, autoimmune diseases, hypersensitivity reactions, and toxic reactions to drugs and toxins[1]. Clinical presentations of myocarditis vary from asymptomatic or with mild symptoms of chest pain, dyspnea, or palpitations to high-risk cardiac conditions with severe heart failure (HF), refractory arrhythmias, cardiogenic shock, and sudden cardiac death[2].
Regarding the severity and prognosis of myocarditis, most patients successfully recover, and the clinical course is mostly self-limited. However, in a study, nearly 30% of individuals reportedly developed dilated cardiomyopathy (DCM)[3]. Furthermore, prompt and aggressive treatment can help achieve complete recovery in patients who develop a fulminant presentation with severe left ventricular (LV) dysfunction[4]. Although studies have found that patients with myocarditis have poor long-term clinical outcomes[5-7], the outcomes and follow-up strategies after full recovery require further investigation.
Herein, we present a case of delayed development of DCM after a long remission period of fulminant myocarditis.
CASE PRESENTATION
Chief complaints
A 21-year-old woman who presented with dyspnea, tachycardia, and hypotension was transferred to our emergency department.
History of present illness
She was admitted to the local hospital for 2 d for upper abdominal discomfort and constipation.
History of past illness
She had a history of cesarean delivery a year before.
Personal and family history
She had no history of family history of any heart disease.
Physical examination
Her initial vital signs were as follows: Blood pressure of 137/67 mmHg, pulse rate of 184 beats per min, respiration of 40 breaths per minute, and a body temperature of 36.7 ℃. Other general examinations were not remarkable. Atrial fibrillation was detected, and the rate still increased even after the administration of digitalis. Her systolic blood pressure suddenly dropped, so she received electric defibrillation at 100 J, and her hemodynamic status was stabilized with a sinus heart rhythm.
Laboratory examinations
Remarkable laboratory findings were highly elevated levels of liver enzymes,i.e., aspartate aminotransferase of 3381 U/L (reference, < 37 U/L) and alanine aminotransferase of 1197 U/L (reference, < 41 U/L); extremely increased B-type natriuretic peptide level of 2233 pg/mL (reference range, 0-100 pg/mL); mild hypokalemia, with serum potassium concentration of 3.2 mmol/L (reference range, 3.3-5.1 mmol/L); white blood cell count of 11710 × 103/mm3; and C-reactive protein of 10.7 mg/L. Other than that, no abnormal findings, including cardiac enzymes, were found.
Imaging examinations
Her initial chest X-ray imaging showed remarkable cardiomegaly and bilateral pulmonary edema (Figure 1A). The initial transthoracic echocardiography (TTE) demonstrated dilated left atrium and LV and severe LV systolic dysfunction with an ejection fraction (EF) of 24% (Figure 2A; Supplementary Video 1). Mild mitral regurgitation and a small amount of pericardial effusion were found. On day 7 of hospitalization, cardiac magnetic resonance (CMR) imaging revealed endocardial edematous change and delayed gadolinium enhancement from the interventricular septum to the inferior wall of the LV (Figure 3). The myocardial perfusion of contrast was normal on CMR. Liver ultrasonography to rule out severe hepatic illness revealed only mild-to-moderate fatty liver.
FURTHER DIAGNOSTIC WORK-UP
She was diagnosed with acute myocarditis based on her acute clinical presentation and CMR findings. Increased liver enzymes improved dramatically with diuretic therapy and were thought to be the result of hepatic congestion following HF. After clinical stabilization, she was discharged and outpatient follow-up was arranged. However, she was readmitted at night of the same day that cardiopulmonary resuscitation was performed. On arrival, endotracheal intubation was performed, and repetitive defibrillation continued throughout the day. Severe arrhythmias, including ventricular fibrillation, ventricular tachycardia, and supraventricular tachycardia, recurred with hypotension. Subsequently, amiodarone and dobutamine were infused, and extracorporeal membrane oxygenation (ECMO) was initiated for circulatory support. As a result, her vital sign stabilized, and fatal arrhythmia was not observed. ECMO was discontinued, and an implantable cardioverter defibrillator (ICD) was inserted for secondary prevention.
On the second visit to the emergency department, the levels of cardiac enzymes were increased: Creatinine kinase-MB, 35.4 ng/mL (reference, < 5 ng/mL) and troponin-I, 2.67 ng/mL (reference range, 0-0.04 ng/mL). High neutralizing antibody titers to Coxsackie B1 virus (titer 1:64) were confirmed, and autoantibodies were negative. Although endomyocardial biopsy was not performed, she was clinically diagnosed with fulminant myocarditis based on TTE and CMR findings on clinical presentation. For HF, beta blockers, angiotensin receptor blockers, and diuretics were prescribed. TTE on day 21 revealed improved EF up to 40%.
One year later, the cardiomegaly detected by chest X-ray imaging was improved, and her follow-up LVEF recovered to normal range (Figures 1B and 2B; Supplementary Video 2). In the 7-year follow-up outpatient care, her condition and ICD without medications were regularly checked up. During the follow-up, she did not present any symptoms or signs, and there was only one event of inappropriate shock as a response to sinus tachycardia.
On the 8thyear, paroxysmal atrial fibrillation and rapid ventricular response were detected by ICD recording, and the LVEF decreased to 42%, which means that she had a relapse of HF (Figures 1C and 2C; Supplementary Video 3). There was no definite evidence of aggravating factors regarding her disease such as medication, alcohol, infection, and even emotional stress. She presented dry cough, ankle edema, and chest discomfort gradually. Guideline-based medications were started again, and her condition symptomatically improved.
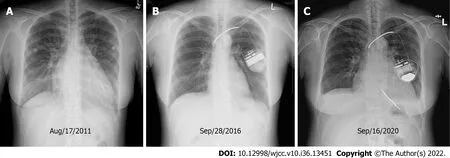
Figure 1 Serial chest X-ray images. A: Cardiomegaly and pulmonary edema were observed at the initial presentation; B: Cardiac silhouette of the following image was normalized; C: Overt cardiomegaly and pleural effusion developed, and recurrent dilated cardiomyopathy was finally diagnosed.
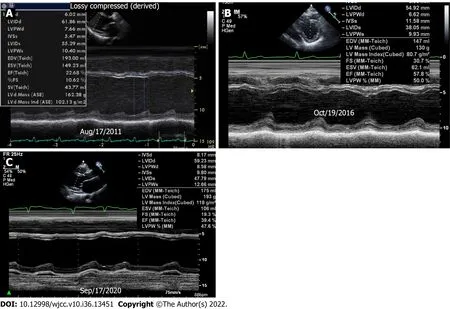
Figure 2 Transthoracic echocardiography. A: Baseline echocardiography showed dilated left ventricular (LV) dimension and severely decreased LV ejection fraction (EF); B: Preserved LVEF at one year follow-up; C: The last M-mode image showed dilated LV and low LVEF again. Movies of the serial change of 4-chamber views showed the same findings.
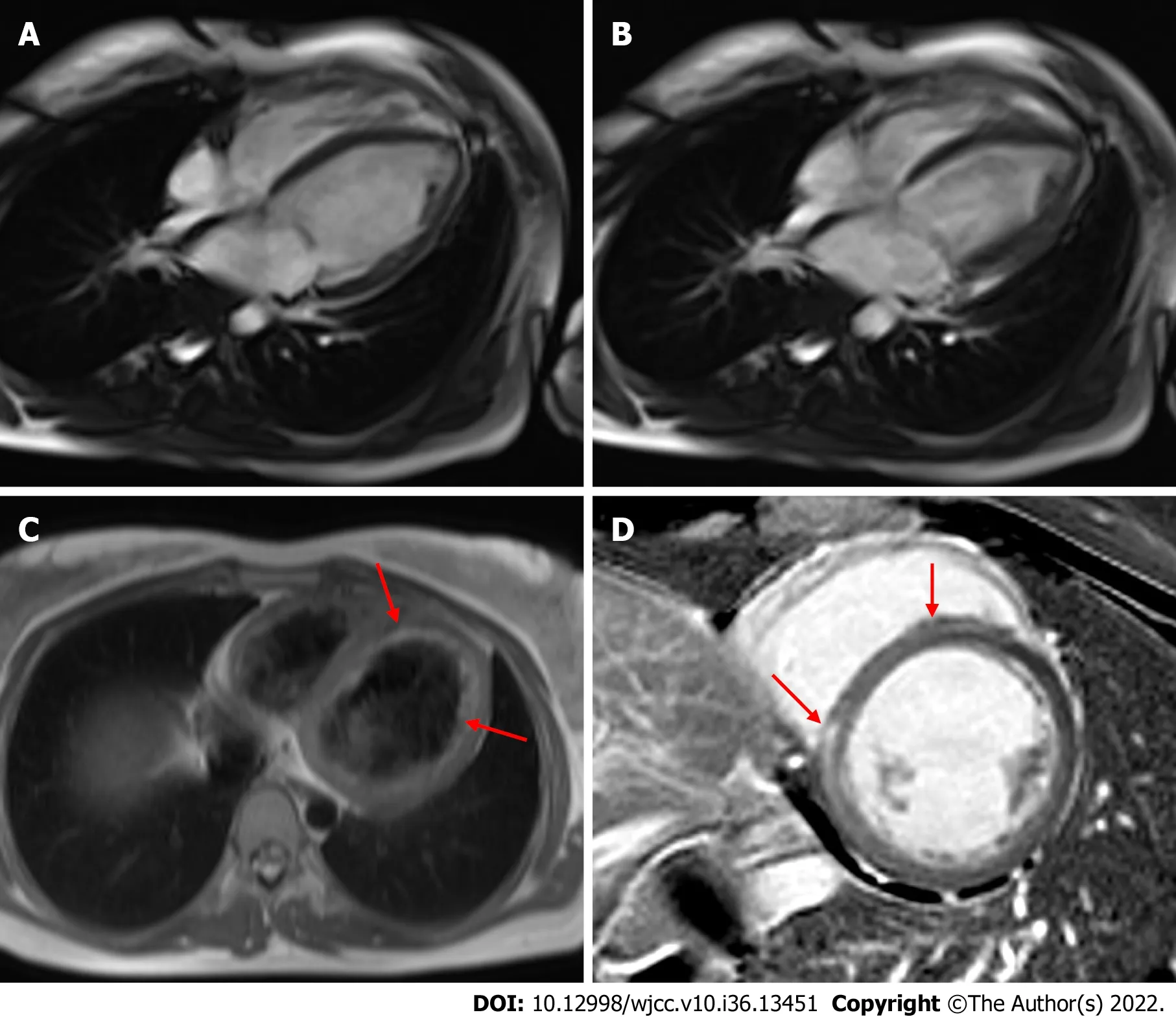
Figure 3 Cardiac magnetic resonance. A and B: Decreased left ventricular systolic function was observed (A: Diastole and B: Systole); C: A T2-weighted image shows diffuse endocardial edema (arrow); D: A T1-delayed image revealed late gadolinium enhancement in the mid-layer of the interventricular septum(arrow).
FINAL DIAGNOSIS
Initially, the patient was clinically diagnosed with fulminant myocarditis based on TTE and CMR findings on clinical presentation. The patient was finally diagnosed with DCM with a long remission period after viral fulminant myocarditis.
TREATMENT
She was given an angiotensin receptor blocker, a vitamin K antagonist, and digitalis as conventional treatment for DCM and atrial fibrillation.
OUTCOME AND FOLLOW-UP
The most recent imaging performed on March 2021 showed a slight improvement in LVEF (47%). She is currently not experiencing any clinical adverse events.
DISCUSSION
Fulminant myocarditis is a severe inflammatory myocardial disease often induced by cardiotropic viruses such as parvovirus, human herpes virus-6, coxsackie virus, human immunodeficiency virus, and cytomegalovirus[5]. Despite different clinical courses and outcomes, up to 30% of patients with acute myocarditis progressed to DCM, which is clinically defined by LV dilatation and systolic dysfunction[3]. The long-term poor clinical outcomes of patients with myocarditis have been reported[5,6], Escheret al[7] reported that about 50% of patients who suffered from acute myocarditis developed diastolic HF with preserved EF in a 6-year long-term follow-up period. However, it is unknown when DCM develops following the resolution of fulminant myocarditis.
In this case, we believed the patient had recovered completely from fulminant myocarditis, and she had been well with normal LVEF and normal diastolic function for 7 years. The paroxysmal atrial fibrillation event was the first sign of recurrent HF. It took 6 mo from the event of atrial fibrillation on the ICD to the onset of symptomatic HF. Studies and cases of recurrent myocarditis have been reported, with different intervals and varying causes[8,9]. However, we believe that our case is consistent with the study of Escheret al[7] in that the patient developed a long-latency relapse of HF because her symptoms and signs aggravated gradually. Recently, inflammatory cardiomyopathy, including DCM following acute myocarditis, has been recognized. Latent myocarditis caused by persistent virus and chronic inflammation is the major pathology of inflammatory cardiomyopathy, and it is commonly reported as a chronic and progressive impairment[10,11]. In another aspect, Spotnitz and Lesch[12] hypothesized the idiopathic dilated cardiomyopathy could be a late complication of healed viral myocarditis. Ghanizadaet al[5] demonstrated a higher risk of HF hospitalization and all-cause mortality among patients with myocarditis, even in patients without cardiovascular events and those on HF medications within the first year of discharge, compared to matched controls.
As DCM has been demonstrated to be one of the most common hereditary cardiomyopathies, genetic analysis of mutations for DCM became essential to determine the pathogenesis of the disease[13]. Our patient did not participate in the genetic test for cardiomyopathies because she had no family history related to cardiovascular disease and her medical history of myocarditis was apparent. However, further DCM genetic evaluation would be helpful to rule out any genetic cause for the development of DCM.
To the best of our knowledge, there has been no reported case of DCM developing after such a long latent period while maintaining normal LV function after a full recovery from viral fulminant myocarditis. To date, the long-term follow-up strategy after restoration of fulminant myocarditis has not been established. Moreover, the TRED-HF trial demonstrated a relapse of HF among patients who stopped pharmacological treatment after their LV function was restored[14]. Therefore, we suggest that continuous and regular follow-up and individualized pharmacologic treatment would be required in patients recovering from acute myocarditis. This precaution also should be taken in the case of COVID-19 myocarditis, which has been issued for a severe cardiovascular complication, as well as in some cases of COVID-19 mRNA vaccine-associated myocarditis.
CONCLUSION
We presented one clinical experience that even though patients who are thought to be fully recovered from acute fulminant myocarditis and seemed to be stable for a long-time follow-up period, may develop DCM unexpectedly and they should be clinically monitored at outpatient clinic carefully and regularly with a long period of follow-up.
FOOTNOTES
Author contributions:Park JR was the patient’s cardiologist, reviewed the literature, and contributed to the critical revision of the manuscript; Lee SD reviewed the literature, interpreted the clinical findings, and contributed to the manuscript’s drafting; Kang MG, Kim K, Lee HJ, and Kim HR contributed to the manuscript drafting; all authors have read and approved the final manuscript.
Informed consent statement:Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement:The authors declare that they have no conflict of interest.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:South Korea
ORCID number:Jeong Rang Park 0000-0001-5234-1251.
S-Editor:Chen YL
L-Editor:A
P-Editor:Chen YL
 World Journal of Clinical Cases2022年36期
World Journal of Clinical Cases2022年36期
- World Journal of Clinical Cases的其它文章
- Liver injury in COVID-19: Holds ferritinophagy-mediated ferroptosis accountable
- Amebic liver abscess by Entamoeba histolytica
- Living with liver disease in the era of COVID-19-the impact of the epidemic and the threat to high-risk populations
- Cortical bone trajectory screws in the treatment of lumbar degenerative disc disease in patients with osteoporosis
- Probiotics for preventing gestational diabetes in overweight or obese pregnant women: A review
- Effectiveness of microwave endometrial ablation combined with hysteroscopic transcervical resection in treating submucous uterine myomas
