Recurrence of intratendinous ganglion due to incomplete excision of satellite lesion in the extensor digitorum brevis tendon: A case report
Jeong Jin Park, Hyun Gyu Seok, Hongfei Yan, Chul Hyun Park
Jeong Jin Park, Hyun Gyu Seok, Hongfei Yan, Department of Orthopaedic Surgery, Yeungnam University Hospital, Daegu, Korea, Daegu 42415, South Korea
Chul Hyun Park, Department of Orthopaedic Surgery, College of Medicine, Yeungnam University, Daegu 42415, South Korea
Abstract BACKGROUND Intratendious ganglions are rare lesions, especially on the foot and ankle. Although several studies have presented the intratendinous ganglion of the foot and ankle, there are only few reported cases, and no cases of recurrence or secondary surgery have been reported.CASE SUMMARY We present the case of a 32-year-old man with an intratendinous ganglion of the second extensor digitorum brevis (EDB) tendon that recurred after ganglion excision. Magnetic resonance imaging (MRI) performed before the first surgery was reviewed to analyze the causes of the recurrence. We confirmed that there was a lack of satellite detection. After recurrence, MRI revealed an extratendinous lesion, tenosynovitis, and intratendinous ganglion of the second EDB tendon. Since the second EDB tendon can compensate for the extrinsic muscle, en bloc resection was performed alone. In addition, meticulous excision and synovectomy were performed for extra-tendinous lesions and tenosynovitis, respectively. The patient returned to daily life without any functional problems or recurrence.CONCLUSION If removal of the affected tendon is not fatal, en bloc resection should first be considered to prevent incomplete excision and intraoperative leakage. When planning surgical excision, it is necessary to evaluate the presence of satellite lesions along the course of the affected tendon.
Key Words: Intratendinous ganglion; Recurrence; Surgical excision; En bloc resection; Case report
INTRODUCTION
Ganglions are common benign tumor-like lesions caused by mucoid degeneration of connective tissues, including the joint capsule, tendon sheath, and tendon[1-4]. They were classified according to their sites of origin. Among these, the intratendinous ganglion, which occurs in the tendon substance, is the rarest[2,4,5]. Most intratendinous ganglions reported so far have been found in the extensor tendons of the wrist or hand[2,6-8]. An intratendinous ganglion on the foot or ankle is an even rarer disease, with few reported cases[9,10]. The etiology of intratendinous ganglions remains unclear. One possibility, based on the fact that tenosynovitis or associated tendon tears are commonly found around ganglion cysts, is the recurrent injury to the tendon with subsequent cystic degeneration[1]. Congenital anomalies may be present in patients with no history of trauma or sprains in the affected areas[3]. Intratendinous ganglions cause soft tissue swelling as well as symptoms such as pain and neuropathy[11-14].
An intratendinous ganglion can be treated using one of several methods, including aspiration, surgical excision, anden blocresection of the entire affected tendon. Aspiration is a straightforward method; however, it has a high recurrence rate of approximately 50%-70%, which makes it less preferred as a treatment option[12,14]. Surgical treatment should be considered for patients with persistent pain, nerve compression, tendon dysfunction, or recurrence after more conservative treatments[11,15]. Surgical methods include excision of the ganglion anden blocresection, with or without an additional procedure[8-10]. Although surgical excision can preserve tendon function, a risk of recurrence remains due to intraoperative leakage and incomplete resection of the ganglion[3]. However,en blocresection of the affected tendon exerts a low risk of recurrence and can result in functional restrictions and deformities[10]. Therefore, additional procedures such as tenodesis and tendon transfer may be required[2,9,10]. The distinct advantages and disadvantages of each method make it clinically vital to decide which approach should be used for the primary treatment. In addition, for cases of recurrence, it is important to identify the cause and plan for secondary surgery.
To the best of our knowledge, there have been no reports on assessing the recurrence of intratendinous ganglions of the foot and ankle after excision and the results of secondary surgeries. We report a case of an intratendinous ganglion in the second extensor digitorum brevis (EDB) tendon that recurred after excision of the ganglion alone, with successful secondary treatment byen blocresection of the entire tendon.
CASE PRESENTATION
Chief complaints
A 32-year-old Korean man presented to the orthopaedic clinic with a complaint of a painful mass on the dorsum of the right foot for 3 wk.
History of present illness
Symptoms started 3 wk prior to presentation and gradually worsened.
History of past illness
The patient with a painful mass on the dorsum of the right foot was diagnosed with intratendinous ganglion in the second EDB tendon at a local hospital. Open excision of the ganglion with tendon repair was subsequently performed. Histological examination of the tissue confirmed the diagnosis of intratendinous ganglion. Approximately 3 mo after surgery, the mass lesion recurred, and the patient was admitted to our hospital.
Personal and family history
The patient had no relevant family medical history.
Physical examination
The patient had no history of trauma to the affected area. Physical examination revealed a surgical scar on the dorsum of the right forefoot between the second and third rays. A palpable mass approximately 5 cm × 4 cm in size was found around the scar and was accompanied by slight tenderness. The range of motion of his toes was unrestricted.
Laboratory examinations
The results of the routine blood and urine tests, blood biochemistry, and immune and infection indices were normal.
Imaging examinations
Plain radiographs showed a slight enlargement of the soft tissue and no bony abnormalities. Magnetic resonance imaging (MRI) revealed multiple lobulated cystic lesions within and above the second EDB tendon, identified by regions of high signal intensity on a fat-saturated T2-weighted image (Figure 1A) and low signal intensity on a T1-weighted image (Figure 1B). Extensive tenosynovitis was observed around the ganglion cyst (Figure 2).
FURTHER DIAGNOSTIC WORK-UP
We diagnosed this as recurrence after open excision of the intratendinous ganglion. MRI scans taken before the first surgery were reviewed to understand the cause of recurrence. A previous MRI scan showed no lesions, except for a cystic lesion inside the second EDB tendon, with no indications of tenosynovitis in fat-saturated T2-weighted sagittal (Figure 3A) and axial (Figure 3B) images. However, a lesion with high signal intensity was observed at the proximal portion of the second EDB tendon before attachment to the calcaneus (Figure 4).
FINAL DIAGNOSIS
We concluded that incomplete resection was performed, mainly because of the failure to detect the satellite lesion located in the proximal portion of the second EDB tendon. In addition, contamination was thought to have occurred following intraoperative leakage during open excision, which in turn caused extra-tendinous lesions and tenosynovitis.
TREATMENT
Considering the presence of multiple ganglion cysts in the entire tendon from the proximal to the distal end,en blocresection was planned to prevent a recurrence. As the EDB tendon can be compensated for by an extrinsic muscle, tendon transfer was not planned. Additionally, meticulous excision of the extratendinous ganglion and synovectomy were planned.
Under epidural anesthesia, the patient was placed in the prone position with a tourniquet applied to the ipsilateral thigh. The procedure was performed by extending a previous longitudinal incision. Extratendinous ganglions and tenosynovitis were observed in the extensor tendons (Figure 5). After the excision of the extra-tendinous ganglions, the second EDB tendon was found to have an enlarged spindle shape (Figure 6). Bulbous satellite lesions were observed in the proximal portion of the tendon (Figure 7A), and a colorless jelly-like content was found inside the cysts when incised (Figure 7B). Following the extension of the incision to the anterior process of the calcaneus, remnant tendon removal and electrocauterization were performed. (Figure 8). The second metatarsophalangeal joint capsule was then removed to prevent a recurrence.

Figure 1 Multiple lobulated cystic lesions within and above the second extensor digitorum brevis tendon. A: Fat-saturation T2-weighted image;B: Fat-saturation T1-weighted image.

Figure 2 Extensive tenosynovitis around the ganglion cysts.
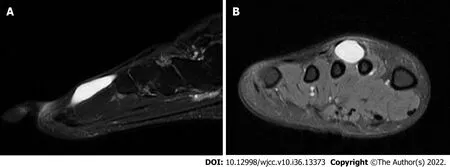
Figure 3 Intratendinous ganglion of the second extensor digitorum brevis tendon without extra-tendinous lesion and tenosynovitis on a fat-saturation T2-weighted image. A: Sagittal image; B: Axial image.

Figure 4 Satellite lesion at the proximal end of the second extensor digitorum brevis tendon before attaching to the calcaneus.

Figure 5 Extra-tendinous ganglion cysts and tenosynovitis over the extensor tendons.
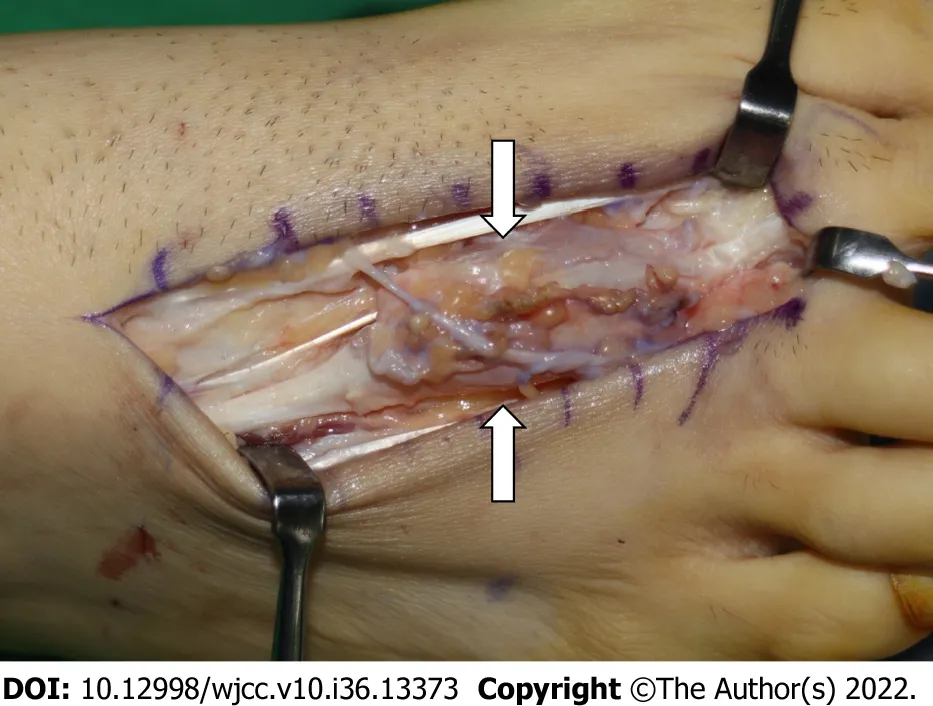
Figure 6 The second extensor digitorum brevis tendon with enlarged spindle shape.
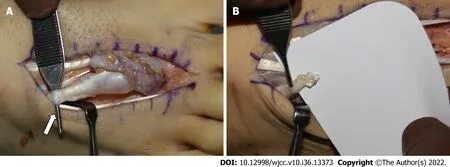
Figure 7 Satellite lesion of the second extensor digitorum brevis tendon. A: Bulbous satellite lesions in the proximal portion of the tendon; B: Colorless jelly-like content from the inside of the incised tendon.

Figure 8 Remnant tendon removal and electrocauterization were performed at the anterior process of the calcaneus.
OUTCOME AND FOLLOW-UP
Histological examination confirmed the diagnosis of intratendinous ganglion. The patient returned to his daily life without functional problems after surgery, and no recurrence of the lesions was found 18 mo after surgery.
DISCUSSION
An intratendinous ganglion is a rare lesion that originates within the tendon substance and causes soft tissue swelling[13,16]. It can cause persistent pain, functional restriction, and neurovascular compression[12,14]. Spontaneous tendon rupture is reportedly a high-risk factor[4,9,16]. Surgical treatment is considered only in patients with these symptoms[11,15]. Surgical treatments for intratendinous ganglions may involve only excision of the ganglion oren bloc resection.En blocresection is superior in preventing recurrence[10]; however, removal of the whole tendon results in functional loss of the affected tendon and may require additional procedures[10,15]. Therefore, when deciding on the optimal surgical approach, it is important to assess whether functional loss of the affected tendon may be fatal.
We reviewed previous cases of intratendinous ganglions that occurred in the lower extremities. Shimozonoet al[15] and Endoet al[17] only performed excisions of the ganglions because none of the cases had any soft tissue to compensate for the muscle strength of the FHL tendon; good clinical results were obtained without recurrence. Kimet al[3] also performed an excision of the ganglion to preserve semimembranosus tendon function; however, they noted a recurrence that was thought to be due to incomplete excision. Konoet al[10] performeden blocresection without additional procedures on the intratendinous ganglion of the second EDB tendon because the extrinsic muscle compensates for functional loss. The patient showed good progress, without functional loss or ganglion recurrence.
In our case, the patient underwent ganglion excision as the first surgery in a local hospital. The medical professionals treating him seemed to have thought that complete excision of the ganglion was possible because of the absence of a satellite lesion. However, when the previous MRI scan was reviewed, small cystic lesions with a high signal intensity on fat-saturated T2-weighted images were observed near the proximal end of the second EDB tendon. We believe that inability to detect satellite lesions is an important cause of recurrence. When clinical examination was conducted at our hospital after recurrence, the symptoms and lump size were more aggravated than those before, and MRI confirmed that these were accompanied by extra-tendinous ganglion cysts and tenosynovitis.
The recurrence rate after excision of the ganglion of the lower extremities has been reported to be approximately 10%[18,19]. Studies have not been conducted on the recurrence rate following surgical excision of intratendinous ganglions; however, it is expected to be much higher than 10% owing to the difficulty of complete removal of the ganglion[7,20,21]. In addition, considering the current case of extra-tendinous lesions and severe tenosynovitis after recurrence, repeated surgery requires not only expansion of the skin incision range but also removal of the massive soft tissue, which can lead to poor clinical results. If the removal of the affected tendon does not cause a functional deficit,en blocresection could be an ideal treatment method to avoid intraoperative leakage and incomplete resections that lead to recurrence. However, excision of only the ganglion should be considered first in cases of fatal functional deficiency and difficulty in performing additional procedures. To prevent incomplete excision, careful evaluation of MRI scans is essential to detect the presence of satellite lesions along the course of the affected tendon. Removal of all satellite lesions should be carefully planned to avoid the risk of another surgery. When complete removal is difficult, surgical treatment should be planned after evaluating the advantages and disadvantages of each approach.
CONCLUSION
To the best of our knowledge, no other case of an intratendinous ganglion recurrence despite open excision of the foot and ankle has been reported in the literature. Complete excision failure was accompanied by the recurrence of the intratendinous ganglion, extra-tendinous lesions, and tenosynovitis. If removal of the affected tendon is not accompanied by fatal functional restrictions,en blocresection should first be considered to prevent incomplete excision and intraoperative leakage. Finally, when planning a surgical excision, it is necessary to carefully evaluate the presence of satellite lesions along the course of the tendon.
FOOTNOTES
Author contributions:Park JJ and Park CH contributed to manuscript writing and editing, and data collection; Park JJ, Seok HG, and Yan HF contributed to data analysis; Park CH contributed to conceptualization and supervision; all authors have read and approved the final manuscript.
Informed consent statement:Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement:The authors declare no conflict of interest for this article.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:South Korea
ORCID number:Chul Hyun Park 0000-0002-3101-8655.
S-Editor:Ma YJ
L-Editor:Wang TQ
P-Editor:Ma YJ
 World Journal of Clinical Cases2022年36期
World Journal of Clinical Cases2022年36期
- World Journal of Clinical Cases的其它文章
- Liver injury in COVID-19: Holds ferritinophagy-mediated ferroptosis accountable
- Amebic liver abscess by Entamoeba histolytica
- Living with liver disease in the era of COVID-19-the impact of the epidemic and the threat to high-risk populations
- Cortical bone trajectory screws in the treatment of lumbar degenerative disc disease in patients with osteoporosis
- Probiotics for preventing gestational diabetes in overweight or obese pregnant women: A review
- Effectiveness of microwave endometrial ablation combined with hysteroscopic transcervical resection in treating submucous uterine myomas
