Acute moderate to severe ulcerative colitis treated by traditional Chinese medicine: A case report
Bin Wu
Bin Wu, Department of Traditional Chinese Medicine, The Third Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou 310005, Zhejiang Province, China
Abstract BACKGROUND Ulcerative colitis (UC), also known as chronic nonspecific UC, is an inflammatory bowel disease characterized by diffuse colonic mucosal inflammation. The incidence and prevalence of UC have risen markedly, and the disease seriously affects the quality of life of patients and imposes a great burden on the world health care infrastructure and economy.CASE SUMMARY Case I describes a 34-year-old female who came to see a doctor because of repeated abdominal pain, diarrhoea and purulent blood for 2 mo. This patient had UC with an initial onset, an active stage and a wide range of lesions. After the poor effect of sulfasalazine and mesalazine, the patient's condition gradually deteriorated, her abdominal pain and bloody stools continued, and anemia occurred. She began treatment with the Chinese medicine Guizhi Dahuang decoction, which was taken orally twice a day, 200 mL each time. After 6 mo of treatment, abdominal pain, diarrhoea, bloody stool and other symptoms disappeared. No abnormality was found by repeat electronic enteroscopye, and the anemia was corrected. The patient's condition did not recur after nearly 4 years of follow-up.CONCLUSION A series of symptoms in this UC patient significantly improved with the administration of traditional Chinese medicine.
Key Words: Traditional Chinese medicine; Ulcerative colitis; Complementary and alternative therapy; Gastroenterology; Clinical efficacy; Case report
INTRODUCTION
Ulcerative colitis (UC) is a continuous inflammatory intestinal disease characterized by abdominal pain, diarrhoea, mucinous bloody stool and other clinical manifestations, (often accompanied by extraintestinal manifestations at sites such as the bone, eye, skin, liver and gall bladder), mainly with damage to the mucosa and submucosa of the colon. It gradually spreads to the whole colon and may injure the ileocaecal portion. Genetic, immune, intestinal mucosal barrier function, environmental, psychological and other factors are considered to be involved in the pathogenesis of the disease. Which is difficult to cure, easily to recurring, clustered and regional. Studies have shown that more than 20% of patients with UC will develop inflammatory colon cancer, with a mortality rate of 50% within 30 years. The drugs used in the clinical treatment of UC mainly include aminosalicylic acid, sulfasalazine and corticosteroids, immunosuppressants and monoclonal antibodies. However, long-term or high-dose use of these drugs may lead to more serious adverse reactions, such as abdominal pain, kidney damage, hepatotoxicity and blood diseases[1,2].
The treatment of UC by traditional Chinese medicine (TCM) includes nondrug intervention and drug interventions. The nondrug intervention measures in the treatment of UC are mainly acupuncture intervention measures, including acupuncture, moxibustion, and acupuncture combined with moxibustion. The treatment of UC by TCM involves multiple signal transduction pathways, which show advantages in many aspects, such as reducing inflammation, regulating intestinal immune function, regulating intestinal flora, and repairing the intestinal mucosa, with few adverse reactions and good safety. This study provides a new method and option for the treatment of UC. The present patient had UC with an initial onset, an active stage and a wide range of lesions. Her medical history was not very long. The diagnosis by Western medicine was clear, and specialized treatment was carried out. However, the curative effect was not ideal. The patient's condition gradually deteriorated, abdominal pain and blood in the stool did not stop, anaemia gradually appeared, and she was transferred to Chinese medicine for treatment. It has been reported that Guizhi Dahuang decoction can be applied to treat various kinds of abdominal pain. Guizhi Dahuang decoction was applied to the patient as guided by the theory of TCM syndrome treatment. After 6 mo of treatment, the symptoms of abdominal pain, diarrhoea and bloody stool disappeared, and the anaemia was corrected. Importantly, the patient's condition did not recur after nearly 4 years of follow-up.
CASE PRESENTATION
Chief complaints
A 34-year-old female patient visited our hospital on March 13, 2018, with manifestations of abdominal pain and bloody mucopurulent diarrhoea for 2 mo.
History of present illness
Two months prior, the patient had experienced abdominal distension without obvious inducement; paroxysmal dull pain in the whole abdomen that was aggravated at night; bloody and, thin stool; approximately 3-4 times/day; reduced pain after defecation; chills; and fever, with a maximum temperature of 38 °C. On January 9, 2018, the patient attended the local hospital for a colonoscopy, which suggested UC (Figure 1). On January 22, 2018, the patient was hospitalized in the Department of Gastroenterology of the local hospital for paroxysmal abdominal pain, mainly on the left side, with bloody, sparse stool, approximately 5-6 times/day. She began to be treated with: Mesalazine sustained release granules combined with mesalazine (suppositories). After 1 wk, she improved and was discharged, thereafter continuing outpatient treatment for 5 wk. However, the patient's condition did not improve further. She produced sparse stool 1-2 times/day, and coffee-like stool, abdominal pain and abdominal distension were noted during defecation, accompanied by chills, night sweats, fatigue, poor appetite, and anaemia. Consequently, she came to the outpatient department of our hospital on March 13, 2018, to seek TCM treatment.
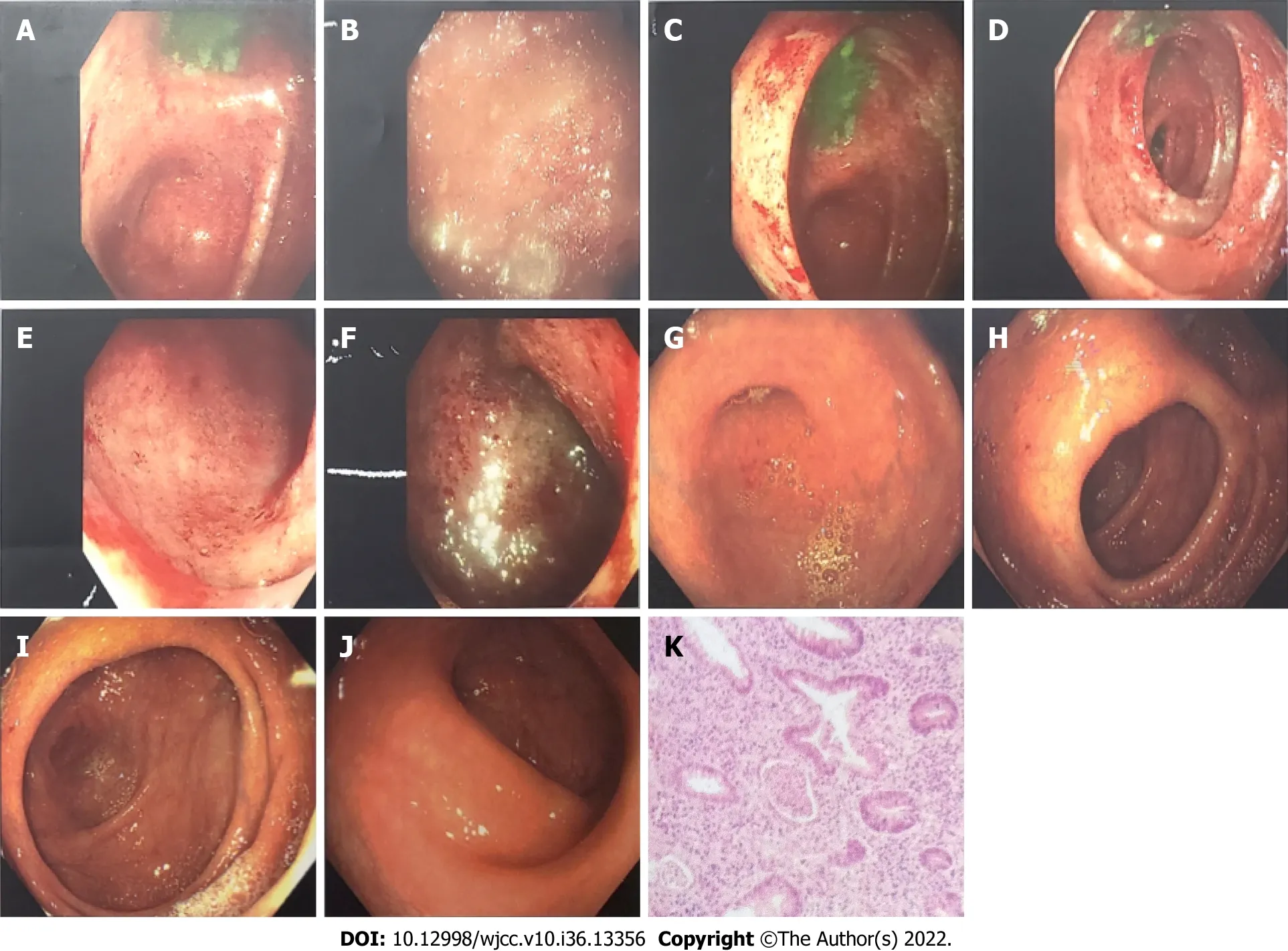
Figure 1 Comparison of colonoscopy results before and after treatment. A-F: Before treatment (January 19, 2018): The mucosa of the whole colon and rectum was congested and edematous, showing patchy hemorrhagic foci, with purulent moss on the surface and partial erosion, of which the right colon and rectum were the most serious; G-J: After treatment (September 9, 2018): There was no hyperemia or swelling around the appendix, clear hyperemia or edema of the mucosa of the blind base and ascending colon, white mucus on the surface, erosion or bleeding, and no erosion or bleeding of the mucosa of the liver flexure,transverse colon, splenic flexure, descending colon and sigmoid colon, ulcers or new organisms were observed. The rectal mucosa was free of erosion, bleeding and new organisms; K: Pathological diagnosis: (Large intestine) mucosa acute and chronic inflammation with crypt abscess formation, consistent with ulcerative colorectal inflammation.
History of past illness
The patient had no previous medical history.
Physical examination
The patient’s temperature was 37.0 °C, the heart rate was 78 beats/min, the respiratory rate was 18 breaths/min, and the blood pressure was 122/78 mmHg.
Laboratory examinations
Laboratory tests showed inflammation (73.4 mg/dL of C-reactive protein) and anaemia (9.7 g/dL of haemoglobin) at the time of visit. See Table 1 for further relevant results.
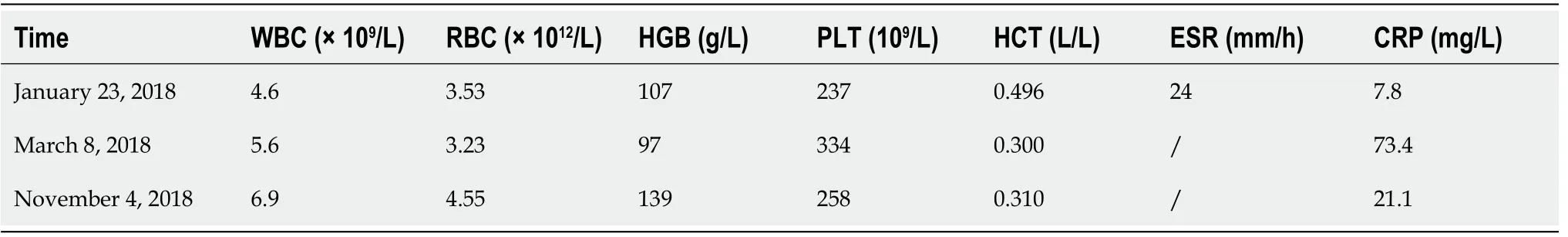
Table 1 Laboratory tests
Imaging examinations
Colonoscopy results showed that the mucosa of the whole colon and rectum was congested and oedemtous, showing patchy haemorrhagic foci, with purulent moss on the surface and partial erosion; the right colon and rectum were the most seriously affected (Figure 1). Pathological diagnosis: Acute and chronic inflammation of the large intestinal mucosa with crypt abscess formation, consistent with ulcerative colorectal inflammation (Figure 1).
FINAL DIAGNOSIS
The final diagnosis was UC.
TREATMENT
Medical records are shown in Figure 2.
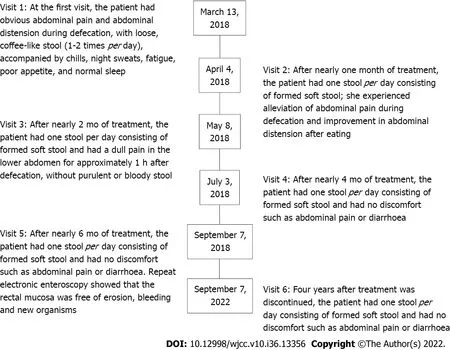
Figure 2 Description of the medical records.
Guizhi Dahuang decoction was selected as the main prescription, which was administered through the whole treatment process. The main drug composition and dosage were Guizhi 9 g, fried white peony 18 g, liquorice 9 g, ginger 9 g, jujube 9 g, and rhubarb 3 g. The above prescription was a daily dosage, with approximately 600 mL of water added and approximately 300 mL of decoction taken orally twice. During the treatment period, appropriate flavouring was given according to different accompanying symptoms and signs of the patients. The dosage of medicine was prescribed for 7 d each time, and the total number of outpatient visits was 22. The whole treatment process lasted nearly 6 mo. During this period, some adjustments were made according to the specific situation of the patient at each follow-up visit. However, the drug composition of Guizhi Dahuang decoction was always maintained through the whole treatment.
During the treatment, the patient was encouraged to reduce the intake of spicy and stimulating food.
OUTCOME AND FOLLOW-UP
The patient was treated with TCM for approximately 6 mo. On September 7, 2018, reexamination of electronic colonoscopy showed that the mucosa of the colon liver flexure, transverse colon, splenic flexure, descending colon and sigmoid colon was free of erosion, bleeding, ulcers and new organisms. The rectal mucosa was also free of erosion, bleeding and new organisms.
Follow-up was carried out 2 mo after the treatment. The patient was generally in good condition, without abdominal pain, diarrhoea or purulent bloody stool. See Table 1 for laboratory inspection and Table 2 for clinical evaluation.
The patient was followed up again 4 years after the treatment. She was generally in good condition, without abdominal pain, diarrhoea, pus or bloody stool. See Table 2 for the clinical evaluation.
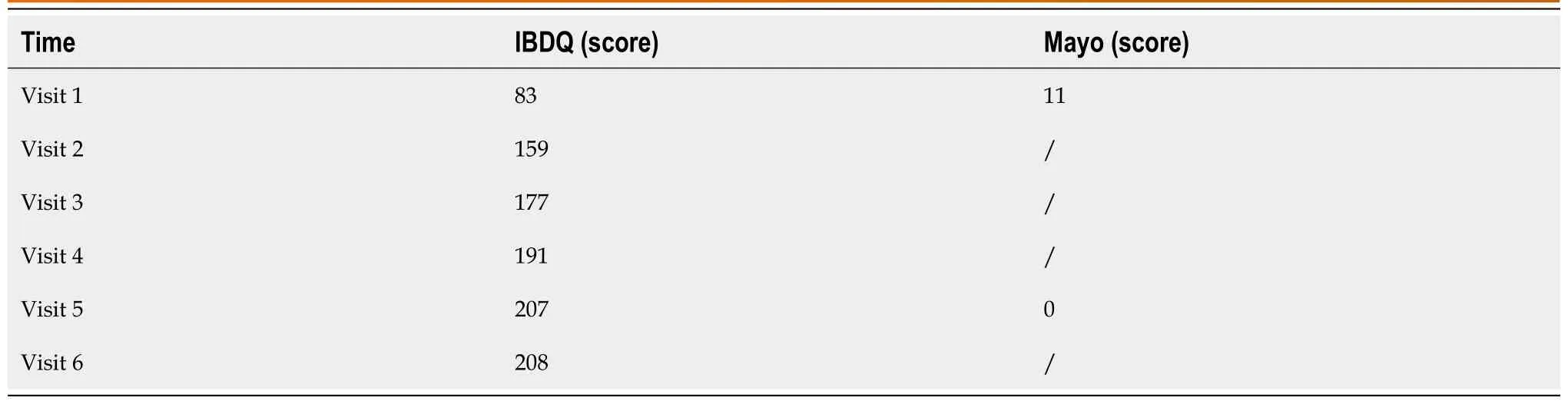
Table 2 Disease condition assessment
DISCUSSION
UC is a continuous inflammatory intestinal disease characterized by abdominal pain, diarrhoea, mucinous bloody stool and other clinical manifestations, often accompanied by extraintestinal manifestations at sites such as the bone, eye, skin, liver and gall bladder, mainly damaging the mucosa and submucosa of the colon. It gradually spreads to the whole colon and may injure the ileocaecal portion[3-5]. Genetic, immune, intestinal mucosal barrier function, environmental, psychological and other factors are considered to be involced in the pathogenesis of the disease[6-8]. UC is difficult to cure, easily to recurring, clustered and regional. Studies have shown that more than 20% of UC patients will develop inflammatory colon cancer, with a mortality rate of 50% within 30 years[9,10].
UC belongs to the category of "dysentery" and "intestinal bleeding" in TCM[11]. The treatment of UC by TCM includes nondrug intervention measures and drug intervention measures. Nondrug intervention measures in the treatment of UC mainly include acupuncture, moxibustion, and acupuncture combined with moxibustion. The drug intervention measures mainly include oral Chinese herbal medicine administration, enemas or oral Chinese herbal medicine combined with enemas. The mechanism of Chinese herbal medicine for the treatment of UC involves multiple signal transduction pathways, showing advantages in many aspects, such as reducing inflammation, regulating intestinal immune function, regulating intestinal flora, and repairing the intestinal mucosa, with few adverse reactions and good safety. It provides a new method and outlook for the treatment of UC[12-14]. Guizhi Dahuang decoction is derived from the treatise on febrile diseases written by Zhang Zhongjing in the Eastern Han Dynasty. According to the theoretical guidance of that book, Guizhi Dahuang decoction can be applied to patients with symptoms of weakness accompanied by abdominal fullness, abdominal pain and diarrhoea. Guizhi Dahuang decoction is composed of Guizhi decoction and rhubarb, and increases the amount of Paeonia in the prescription. There are many studies on Guizhi decoction. Modern pharmacological studies have shown that Guizhi decoction has regulating effects on body temperature, sweat gland secretion, blood pressure, immune function and gastrointestinal movement and has anti-inflammatory, antibacterial, antiviral, hypoglycaemic and cardiovascular protective effects[15]. Total glucosides of paeony (TGP) is the main component of the largest amount of paeony in the formula. More than 90% of the active substances in TGP are paeoniflorin[16]. It has been proposed that TGP and paeoniflorin may exert their immune effects in UC by reducing the accumulation of indole-3-lactic acid in the colon of mice with enteritis and restoring the imbalance of intestinal microbiota in mice with UC[17].The pharmacological effects of rhubarb include diarrhoea, antibacterial, anti-inflammatory,
and antitumor actions; improved renal function; cholagogic, liver-protecting, diuretic, and anticoagulant activities; scavenging of oxygen free radicals; immune regulation; and other functions[18]. As the main component of rhubarb, rhein can significantly alleviate dextran sulfate sodium induced chronic colitis by reducing the level of uric acid and regulating intestinal microbiota[19]. Guizhi Dahuang decoction is used to treat various kinds of abdominal pain, such as non ulcer dyspepsia and irritable bowel syndrome[20]. Although the components of Guizhi Dahuang decoction are complex, and its mechanism of action may involve multiple components and targets, so the pharmacology of a single TCM is not enough to explain the specific mechanism of Guizhi Dahuang decoction in the treatment of UC. However, the above findings combined with previous relevant literature reports lead the author to consider Guizhi Dahuang decoction as playing a role in UC treatment by reducing the inflammatory response, regulating intestinal flora imbalance, and other mechanisms.
This case involved a patient with UC exhibiting with an initial onset, an active stage and a wide range of lesions. After 2 mo of conventional Western medicine treatment, the effect was not ideal, and the condition showed a tendency toward gradual worsening. Abdominal pain and bloody stools were persistent, and there was also secondary aneamia. After 6 mo of the conventional treatment, the patient began to apply Guizhi Dahuang decoction. After 6 mo of further treatment, the abdominal pain, diarrhoea, bloody stools and other symptoms of the patient disappeared. Analysis by electronic colonoscopy showed that there were no obvious abnormalities, and the anaemia was also corrected.
UC has a long course and easily recurs. Therefore, long-term medication is needed to control the disease. The drugs used in the clinical treatment of UC mainly include aminosalicylic acid, sulfasalazine and corticosteroids, immunosuppressants and monoclonal antibodies. However, long-term or high-dose use of these drugs may lead to more serious adverse reactions, such as abdominal pain, kidney damage, hepatotoxicity and blood diseases. After 6 mo of TCM treatment, the patient did not have any adverse reactions. After 4 years of follow-up, it was confirmed that she did not have any symptoms of abdominal pain, diarrhoea or bloody stools and that her general condition was good. Compared with treatment by Western medicine, the advantages of TCM, such as safety and stable efficacy, were once again demonstrated[21-23].
The success of this patient's treatment suggests to us the following: (1) Although the theoretical system of TCM emphasizing personalized treatment is ancient, it can still solve clinical problems in the new era; and (2) Guizhi Dahuang decoction has the potential to treat UC. In addition, relevant studies in the early stage have shown that TCM treatment measures have positive effects in improving the antioxidation capacity of colon tissue, improving the intestinal flora of patients with UC, regulating the bodyily and intestinal immune function, inhibiting the infiltration of inflammatory cells, promoting the health of intestinal function, and alleviating the clinical symptoms of patients with UC; however, the long-term effects are still uncertain[24,25]. This case seems to suggest that the long-term efficacy of Chinese medicine in treating UC may be better than expected.
However, it is difficult to apply universal significance to a single case. The mechanism of Guizhi Dahuang decoction in treating acute UC is not clear. It is hoped that the mechanism of Guizhi Dahuang decoction in the treatment of UC can be explored in the future through randomized, double-blind, longterm, multicenter research and the application of new pharmacological technology to bring more effective, safer and more economical treatment options to patients with UC.
CONCLUSION
A series of symptoms in this UC patient significantly improved following Guizhi Dahuang decoction treatment.
ACKNOWLEDGEMENTS
We thank the patient in this case for her informed consent for using some images for publication of this report.
FOOTNOTES
Author contributions:Wu B is the only author.
Supported byZhejiang Provincial Natural Science Foundation of China, No. LQ20H270010.
Informed consent statement:Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Bin Wu 0000-0002-8404-0741.
S-Editor:Fan JR
L-Editor:A
P-Editor:Fan JR
 World Journal of Clinical Cases2022年36期
World Journal of Clinical Cases2022年36期
- World Journal of Clinical Cases的其它文章
- Liver injury in COVID-19: Holds ferritinophagy-mediated ferroptosis accountable
- Amebic liver abscess by Entamoeba histolytica
- Living with liver disease in the era of COVID-19-the impact of the epidemic and the threat to high-risk populations
- Cortical bone trajectory screws in the treatment of lumbar degenerative disc disease in patients with osteoporosis
- Probiotics for preventing gestational diabetes in overweight or obese pregnant women: A review
- Effectiveness of microwave endometrial ablation combined with hysteroscopic transcervical resection in treating submucous uterine myomas
