Effect of acupuncture-like transcutaneous electrical nerve stimulation on labor pain in nulliparous women: a randomized controlled trial
Zahra MEHRI, Farnoosh MOAFI, Ahad ALIZADEH, Mohammad HABIBI, Fatemeh RANJKESH
1 Student Research Committee, Qazvin University of Medical Sciences, Qazvin 34199-15315, Iran
2 School of Nursing and Midwifery, Qazvin University of Medical Sciences, Qazvin 34199-15315, Iran
3 Metabolic Diseases Research Center, Research Institute for Prevention of Non-communicable Diseases, Qazvin University of Medical Sciences, Qazvin 34199-15315, Iran
4 Irannian Scientific Acupuncture, Tehran 34199-15315, Iran
5 Children Growth Research Center, Research Institute for Prevention of Non-communicable Diseases, Qazvin University of Medical Sciences, Qazvin 34199-15315, Iran
Abstract
Keywords: Transcutaneous Electrical Nerve Stimulation; Acupoint Therapy; Pain; Analgesia; Labor Pain; Pain Measurement;Visual Analog Scale
Labor pain is a unique phenomenon that results from a natural physiological process and is influenced by physical, psychological, and cultural factors, and healthcare systems and providers[1]. The severity of labor pain is one of the factors affecting women’s experience in the process of delivery, which is associated with their satisfaction[2]. Poor labor management can cause chronic pain, depression, and posttraumatic stress in postpartum women[3], and the fear of subsequent childbirth may increase the rate of cesarean section[4]. Therefore,labor pain management is one of the main concerns in women during childbirth[5]. Pharmaceutical methods such as epidural anesthesia and opioids are very effective for labor pain. However, they may cause adverse effects such as instrumental labor and cesarean section due to fetal distress, hypotension, and urinary retention[6]. In contrast, non-pharmacological methods are associated with greater compliance in women and less manipulation[7].
Acupressure is one of the effective nonpharmacological methods for labor pain management[8].The points are on the channels called “meridian”.According to traditional Chinese medicine, there are 12 meridians in the human body in which Qi (vital energy)flows. If an obstacle blocks this flow, it will disrupt energy balance and cause diseases. Acupressure maintains a healthy level by balancing and coordinating the two opposing energies, Yin and Yang[9]. Recently, many studies have been conducted through stimulating points to manage labor pain. Hegu (LI4) and Sanyinjiao (SP6) are points that have been examined extensively in the labor process[10-11]. These points have effects on the intensity of pain, length of delivery, cesarean section, oxytocin usage, women’s satisfaction, and early onset of breastfeeding without side effects[12-14]. Shenmen (HT7)and Neimadian (Extra) are also effective for pain and anxiety management[15-17].
Various methods have been used to stimulate points.Electro-acupressure is one of the non-pharmacological methods and can be used for labor pain management without complications[18-19]. Therefore, researchers have found a way that specifically increases the effectiveness of this method in labor pain management by transcutaneous electrical nerve stimulation (TENS)[20-22].On the one hand, labor pain management is important,and complications of pain relief methods should be taken into consideration. On the other hand, there are limited data on acupuncture-like TENS (ACUTENS), and most studies have been conducted during the first stage of labor using one or two points. Thus, this study was designed to determine the effect of ACUTENS at Hegu(LI4), Shenmen (HT7), Sanyinjiao (SP6), and Neimadian(Extra) in treating labor pain in nulliparous women.
1 Clinical Materials
1.1 Ethical considerations
The Ethics Committee of Qazvin University of Medical Sciences approved the study (Ethics Code No.IR.QUMS.REC.1396.479).
Before the study, the purpose of the study was explained to all the participants, informed consent was obtained, and they were assured that their information would be kept confidential and they could withdraw at any time.
1.2 Inclusion and exclusion criteria
This randomized clinical trial was conducted at Razi Hospital in Qazvin, Iran between January and July 2018(IRCT20171203037731N1).
The inclusion criteria included nulliparous women with 37-42 weeks of gestation, single pregnancy at low risk, and cervical dilation of 3-4 cm.
Those with a birth weight of more than 4 000 g(according to the ultrasound), vaginal hemorrhage in labor, a history of chronic conditions such as diabetes,kidney diseases, cardiovascular diseases, chronic hypertension, drug abuse, cigarette and alcohol use, and skin lesions at the points were excluded from the study.
1.3 Sampling and randomization
The sample size was estimated to be 65 participants in each group based on the previous study[16]using PASS software (http://www.ibmh.msk.su/PASS/), (effect size of 0.5,α=0.05 and 90% study power). With a 10%dropout rate, the final sample was 72 participants in each group.
Sampling was done in two stages. In the first stage, the participants were selected from prenatal health-care centers using convenience sampling. Then, a random allocation of the participants into two groups of intervention and control was carried out by the block randomization method with four blocks. For the purpose of block randomization, the assignment sequence was generated using an online random sequence generator before the beginning of the study. Given that the two groups were studied, four blocks were used, and a letter was assigned to one group (A: intervention group and B:control group). Thirty-six random blocks were selected for randomization.
1.4 Statistical analysis
Data analysis was carried out using the R software(version 4.0.2). Descriptive analysis was used to calculate the mean (x) and standard deviation (s) for continuous variables and the proportions for the categorical variables. The Shapiro-Wilk test was used to examine the normality of the variables. Chi-square test ort-test was used to evaluate the performance of random allocation at the baseline. Natural logarithm was used to reduce the variance of the VAS score and transform it into normal distribution. The VAS scores in the two groups over different stages of delivery were compared using twoway repeated measurement analysis of variance(ANOVA).P<0.05 was considered significant.
2 Interventions
2.1 Control group
The control group received routine care in the delivery room.
2.2 Intervention group
The intervention group received ACUTENS in addition to the same routine care in the delivery room as the control group.
Points: Hegu (LI4), Shenmen (HT7), Sanyinjiao (SP6),and Neimadian [Extra, located on the medial side of the lower leg, 7 Cun (proportional unit of the body) above the medial malleolus and about 0.5 Cun from the posterior edge of the tibia]. Please see Figure 1.

Figure 1. Designations of the points used for acupuncture-like transcutaneous electrical nerve stimulation
Methods:Considering the use of ACUTENS in this study, it was necessary to choose two points. Childbirth is a long process, so to prevent tolerance, we used four practical acupuncture points, including Sanyinjiao (SP6)and Neimadian (Extra) on the lower leg and Hegu (LI4)and Shenmen (HT7) on the hand to reduce pain. At the beginning of the active phase of labor with cervical dilation of 4 cm, the portable TENS machine was placed at Sanyinjiao (SP6) and Neimadian (Extra) unilaterally(the right side), and the stimulation started at a low frequency of 2-4 Hz. The intensity was gradually increased to the point of tolerance or the threshold of pain. Frequency 2-4 Hz with endorphin secretion causes mild analgesia. This stimulation continued until cervical dilation reached 8 cm. At the dilation of 8 cm (the beginning of the pelvic stage of labor), due to the increase in the intensity and frequency of pain and to prevent tolerance, the device pads were connected to Hegu (LI4) and Shenmen (HT7) alternatively. The frequency of the device was adjusted to 100 Hz. Then,the intensity was allowed to increase gradually to the maximum degree of tolerance. To this stimulation, in addition to the secretion of endorphins, serotonin is also secreted, bringing about significant analgesia.
Strong stimulations continued until the end of delivery and episiotomy, and then the device was gradually withdrawn[17].
3 Observation of Efficacy
3.1 Observation items
Two tools were used. The first one was a checklist consisting of questions about demographic data (age,marital status, education level, and job), pregnancy(gestational age, abortion, infertility, membrane status,and fetal weight estimate), and delivery (episiotomy,Apgar score, infant weight, infant sex, duration of the first and second stages of labor, and vaginal hemorrhage).
The outcome was measured using the visual analog scale (VAS) at baseline and then at 4, 6, 8, and 10 cm of cervical dilation, the second stage of labor, during episiotomy, and the first hour after the delivery. The 10-centimeter spectrum ranges from zero (which shows free of pain) to 10 (which demonstrates an extreme intensity of pain). It assesses the participant’s pain intensity. The relative change in pain intensity was calculated as follows. The relative change of pain intensity = (VAS score at the baseline - VAS score at each stage) ÷ VAS score at the baseline × 100%.
3.2 Results
3.2.1 General data
A total of 144 women who were referred to Razi Hospital were enrolled in the study. Due to the loss of samples during the study, the final dataset comprised 130 individuals (64 cases in the intervention group and 66 cases in the control group), (Figure 2). Demographic characteristics were similar in women between the intervention group and the control group due to randomization (P>0.05), (Table 1).
3.2.2 VAS score
Results of multivariate tests of repeated measures ANOVA showed that the interaction between time and group was statistically significant (Wilks’ Lambda=0.345,P<0.001). The univariate test also showed that this interaction effect was statistically significant (Partial Eta Squared=0.345,P<0.001), (Table 2).
The VAS scores of the intervention group were significantly lower than those of the control group in the first and second stages of labor, at episiotomy, and one hour after the delivery (P<0.001), (Table 3).
In the first stage of labor during progressing cervical dilation from 6 cm to full dilatation, the results showed a significant difference in the pain intensity at the beginning of the intervention (P<0.001). In the second stage of labor, the intensity of pain was also significantly lower than that in the control group (P<0.001). In addition, the intensities of the pain at episiotomy and one hour after the delivery were significantly lower than those in the control group (P<0.001), (Figure 3). The pain intensity of the intervention group decreased from the beginning of labor to 37.8% at the end of the first stage compared with that before intervention (Figure 4). In the control group, the severity of pain in the first stage increased by 61.6% compared with the beginning. After the delivery and one hour later, there were decreases in the pain intensity in both groups. However, the decreases in the intervention group were significantly greater (P<0.001).

Figure 2. Flow chart of the study

Table 1. Demographic and reproductive characteristics of the two groups

Table 2. Multivariate and univariate analyses of the VAS score in the two groups

Table 3. Comparison of the VAS score in the two groups

Figure 3. Trend of the pain intensity in the two groups
4 Discussion
We found that ACUTENS at Hegu (LI4), Shenmen(HT7), Sanyinjiao (SP6), and Neimadian (Extra) reduced the experience of pain intensity in the nulliparous women during the active phase of labor compared with the control group. According to the results, the process of labor pain management started half an hour after the onset of the intervention and continued until the end of labor. The intensity of pain in the control group increased with the progress of the active phase of labor, which was statistically significant (P<0.001). In line with the present study, some studies have shown that acupressure application is effective in relieving pain in the first stage of labor[10,23-25].
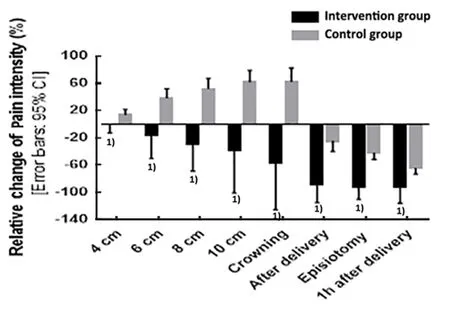
Figure 4. Relative change of the pain intensity based on the pre-intervention pain in the two groups
Contrary to the result of the present study, two studies have shown no significant difference in reducing the severity of labor pain between the two groups[26-27]. The results of the above studies were not consistent with the present study, which could be related to the type of treatment and the number of points, and the duration of stimulation. In this study, in addition to pressing the four points on the hand and foot, a specific tool, the ACUTENS,was used to overcome the development of tolerance to the stimulation of the points, and continued throughout the first stage of labor. The severity of stimulation was customized by the subjects. The protocol was also unique, which could affect the intensity of pain in the first phase of labor.
In Chinese terms, pain is always the result of a shortage or increase in Qi in the vital channels. Therefore,warming, massage, and pressure can lead to a better flow of Qi and pain relief. Better circulation of Qi from acupressure and tonicity of the uterus later in our life cause tonic contractions and prevent intermittent contractions from causing post-traumatic pain[26]. On the other hand, reducing the level of anxiety may also reduce pain. Since anxiety is accompanied by an increase in the catecholamine level, which results in endorphin reduction, increasing pain and prolonging the labor[26,28].Another mechanism is the gate control theory, in which pressure stimulates large nerve fibers and reduces pain sensation by closing the pain gates. Points are the location of sensory receptors with thin filaments (A-delta and C strings), which are located in the muscles and can be activated by needle stimulation, pressure, or electrical stimulation to the peripheral nerves of the skin and sensory receptors[20].
In the present study, the mean pain intensity in the second stage of labor, during episiotomy, and one hour after delivery in the intervention group showed a significant decrease compared with the control group. In line with the present study, a study found that acupressure for 10 min at Hegu (LI4) on the hand and Yongquan (KI 1) on the foot decreased the pain intensity significantly in the second stage of delivery in the intervention group[24]. One study showed that the effect of Hegu (LI4) acupressure on the reduction of postpartum pain was significant[28]. DING L X,et al[14]examined the effect of acupuncture at Neimadian (Extra)on postoperative abdominal pain in China. The results of this study showed that acupuncture was effective as a non-pharmacological pain relief method.
Contrary to the result of the present study, a study found that Hegu (LI4) acupressure for 20 min in the first stage of labor had no effect on the severity of pain in the second stage of labor[10]. One study showed that manual stimulation for 2 min at Guanyuan (CV 4) and Qihai(CV 6) showed no change in the intensity of pain one and two hours after delivery compared with the control group[26]. The result of this study was not consistent with the present study due to the differences in the way of intervention. In the present study, ACUTENS continued throughout episiotomy and the first hour of postpartum based on the subjects’ desire. No similar study was found on the effect of this intervention at episiotomy and after delivery.
Moreover, there was no significant difference in the mean duration of the first and second stages of labor between the two groups. Also, there was no significant difference in the rate of delivery complications, including cesarean section, instrumental delivery, and postpartum hemorrhage[29].
The results of this study indicate that ACUTENS at Hegu (LI4), Shenmen (HT7), Sanyinjiao (SP6), and Neimadian (Extra) can reduce the intensity of pain in different stages of labor in nulliparous women. Therefore,ACUTENS can be used as a non-pharmacological pain relief method for labor pain management. Pregnant women can also use this technique to adjust to labor pain in order to experience less severe pain but a more pleasurable experience of labor.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
There was no project-fund support for this study.
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 10 November 2020/Accepted: 27 May 2021
 Journal of Acupuncture and Tuina Science2022年5期
Journal of Acupuncture and Tuina Science2022年5期
- Journal of Acupuncture and Tuina Science的其它文章
- Efficacy of mild moxibustion combined with surgery for meniscal injury and its effect on TGF-β1 and PDGF levels in the fluid of knee joint
- Effects of acupuncture plus medication on hippocampus SIRT1 and FOXO3a expression, MDA content, and SOD activity of rats with Alzheimer disease
- Improvement effect of acupuncture on locomotor function in Parkinson disease via regulating gut microbiota and inhibiting inflammatory factor release
- Effects of Mo-Rubbing abdomen manipulation on glucose metabolism and inflammatory factors in rats with type 2 diabetes mellitus
- Observation on the therapeutic efficacy of Tuina plus “three-bridge” exercise for non-specific low back pain
- Influence of herbal cake-partitioned moxibustion on lumbar functions and inflammatory factors in patients with lumbar disc herniation due to kidney deficiency and blood stasis
