Recent advances of multimoda ultrasound in image-guided prostate-targeted biopsy
Keywords Prostate Targeted biopsy Ultrasound
ABSTRACT Prostate-targeted biopsy is usually the preferred method over systematic biopsy because it can effectively detect prostate cancer using only a few puncture cores with fewer complications.With the development of ultrasound,it has gained multimodal technological upgrades, such as the emergence of contrast-enhanced ultrasound, ultrasound elastography, and three-dimensional ultrasonography. Moreover, multimodal ultrasound has played an increasingly significant role in prostate-targeted biopsies.
Prostate cancer(PCa)is the second most frequently diagnosed cancer in men worldwide,with approximately 1.4 million new cases diagnosed each year.1As the current“gold standard”for confirming the diagnosis of PCa, prostate biopsy, including systematic biopsy and targeted biopsy,has been widely used in clinical practice since it was first introduced by Hodge et al.in the 1980s.2,3Significantly,a targeted biopsy is usually the preferred method over systematic biopsy because it can effectively detect PCa using only a few puncture cores with fewer complications.4Therefore, precise characterization of the target lesion and performing the targeted biopsy has long been a hot research issue.
Transrectal ultrasonography(TRUS),a universally available imaging modality, has been applied in prostate disease diagnosis because it is a convenient and non-invasive examination technique.5In recent years,multimodal technological upgrades have been developed, such as the emergence of contrast-enhanced ultrasound, ultrasound elastography,and three-dimensional ultrasonography. The diversity of imaging manifestations of PCa facilitates a wide range of applications of multimodal ultrasound techniques in prostate-targeted biopsies. For example,abnormal hypoechogenicity in gray-scale ultrasound, rich blood flow signals in color or power Doppler ultrasound, focal asymmetry hyperenhancement on contrast-enhanced ultrasound, and abnormal stiff regions on ultrasound elastography are all usually indicative of PCa, and could be characterized as lesions for targeted biopsy. Using multimodal ultrasound, the prostate can be thoroughly assessed to determine whether it is suspicious for PCa from the integral shape,inner echo,blood perfusion, and tissue stiffness. Ultrasound, especially three-dimensional ultrasonography, has also played an increasingly important role in real-time guidance of magnetic resonance imaging (MRI)-targeted biopsy. In this article, the application of multimodal ultrasound-guided prostate-targeted biopsy is summarized.
1. Two-dimensional transrectal ultrasonography (2D-TRUS)
Two-dimensional transrectal ultrasonography(2D-TRUS)is the most common ultrasound technique,including grayscale ultrasound and color or power Doppler ultrasound. Using gray-scale ultrasound, the prostate shape, capsule, and internal echo can be carefully observed, and asymmetrical focal hypoechogenicity is usually indicative of PCa. Additionally,color or power Doppler ultrasound can be used to test prostate blood flow signals.If there were any abnormal hypoechogenicity or blood flow signals, an image-guided targeted biopsy was performed (Fig. 1, A-C).Although 2D-TRUS has been routinely applied in prostate disease diagnosis because of its unique advantages of skillful operation and easy control, relatively low sensitivity in PCa localization limits its independent use in targeted biopsies.6Moreover, the low resolution of detailed anatomical structures has also resulted in a reduced positive biopsy rate.7Many researchers have recommended adding in some more puncture cores based on 2D-TRUS-targeted biopsy to improve the rate of PCa detection. However, some PCa lesions might still be missed even if a“saturation” biopsy approach to obtaining enough cores has been employed.8However, it is worth mentioning that 2D-TRUS has an important function in guiding MRI-targeted biopsies in real-time.
2. MRI-ultrasound fusion/cognitive targeted biopsy (MRI-TBx)
The value of multiparametric magnetic resonance imaging(mp-MRI)for identifying PCa lesions has been verified.9,10Many international guidelines have already recommended prebiopsy mp-MRI examinations because it has been proved that mp-MRI could improve the detection rate of PCa and reduce unnecessary biopsies by 25%.11The exceptional performance of mp-MRI in PCa detection further facilitated MRI-guided targeted biopsy as a possible option. However, some intrinsic shortcomings(e.g.,complex operations,specialized settings,low availability,and high cost)have restricted the widespread use of MRI-guided targeted biopsies.Therefore, to supplement the limitations of mp-MRI,2D-TRUS raises concern as a feasible alternative and is fused with MRI to guide targeted biopsy (Fig. 2). Moreover, considering the complicated and time-consuming process of image fusion, MRI-ultrasound cognitive targeted biopsy is gradually being used. However, its PCa detection rate largely depends on the experience of the operator, which has slight instability.12As MRI-ultrasound fusion/cognitive targeted biopsy(MRI-TBx) has been increasingly recognized in clinical practice,2D-TRUS has become an essential part of prostate biopsy. Despite the growing acknowledgment of mp-MRI, there are still some limitations,such as moderate specificity and variable negative predictive values of 63%–98%.11,13In addition, mp-MRI might miss or even characterize some PCa lesions as benign, with a ratio of approximately 58%.14Furthermore,the biopsy revealed PCa in 5%–15%of men with negative MRI findings.9,15Therefore, it is essential to combine MRI-TBx with multimodal ultrasound to more accurately diagnose PCa.
3. Contrast-enhanced transrectal ultrasonography (CE-TRUS)
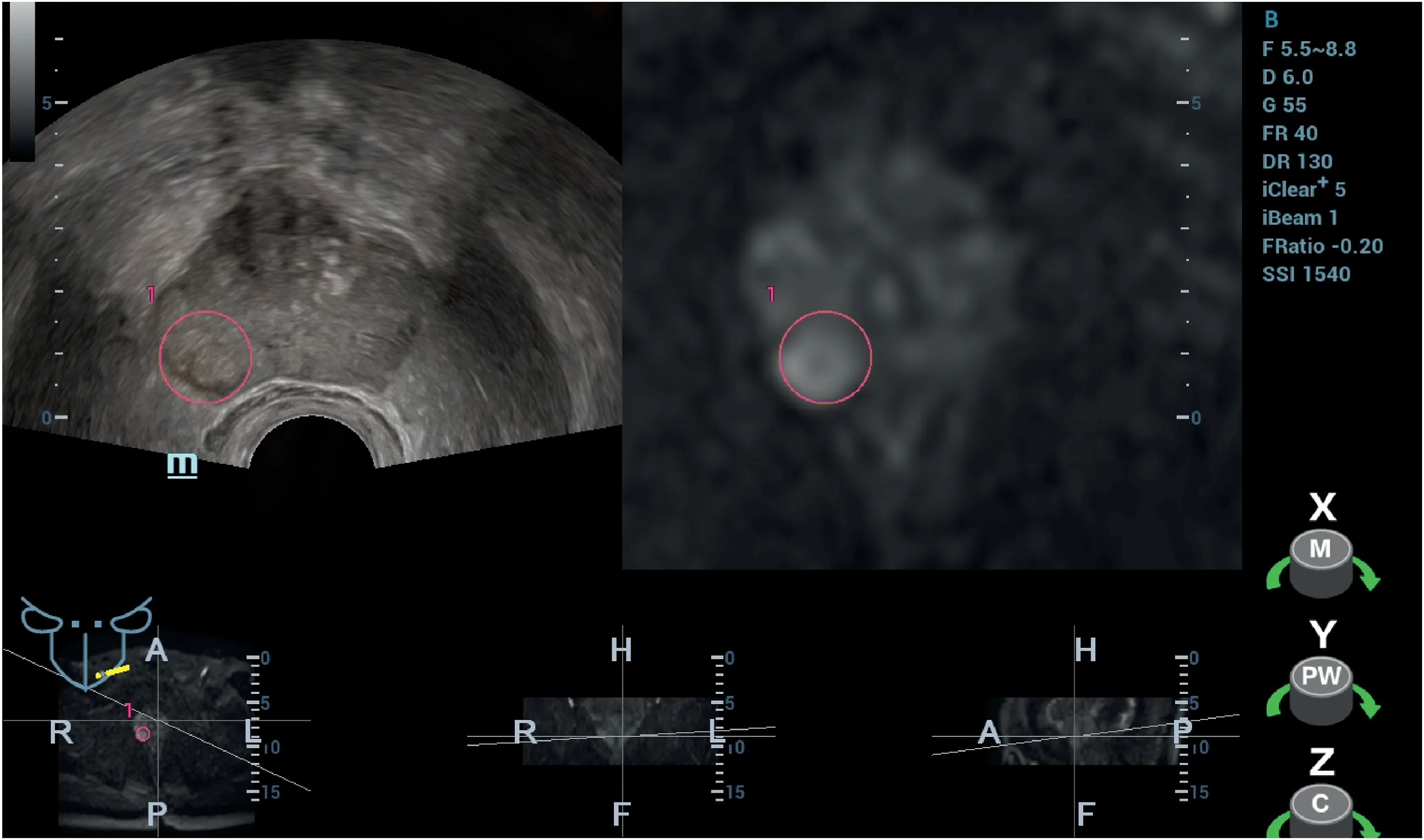
Fig. 2. MRI-ultrasound fusion targeted biopsy. A 62-year-old man with PSA 23.06 ng/ml, 4-core targeted biopsy followed by 12-core systematic biopsy were performed and histopathology detected PCa of Gleason 4+5.Two-dimensional transrectal ultrasonography(2D-TRUS)images fused with MRI in real time determine the suspicious lesion in ultrasound image according to MRI. The red circle represents the puncture target.
Contrast-enhanced transrectal ultrasonography (CE-TRUS) has been widely used in prostate disease diagnosis in recent years because it can dynamically display blood perfusion and vascularity, especially micronourishing vessels related to tumors that may not have sufficient native flow to be detected by conventional color or power Doppler ultrasound.16Focal asymmetry hyperenhancement during the early phase of prostate cancer by CE-TRUS is usually indicative of PCa and can be characterized as a lesion for targeted biopsy (Fig. 1, D). In addition, owing to the angiogenesis of PCa in the early stage, CE-TRUS may be extremely sensitive to lesion localization.Compared to 2D-TRUS,CE-TRUS is better in early detection of the blood flow in tumors and can improve the accuracy of ultrasound.17Therefore, CE-TRUS is widely applicable to prostate-targeted biopsy. It was proven that the positive rate of CE-TRUS-targeted biopsy was higher than that of systematic biopsy,especially for PCa with a higher Gleason score.18Some studies have shown that the combination of CE-TRUS-targeted biopsy and systematic biopsy can improve the detection rate.19However, some drawbacks of CE-TRUS, including increased cost, inability to scan the whole prostate during one administration of the contrast agent, contrast agent allergy,and time consumption, should attract attention. Moreover, there are some limitations of CE-TRUS in detecting extensive tumors with relatively low Gleason scores.19
4. Transrectal shear wave elastography (SWE)
The proportion of extracellular matrix proteins associated with tumors would increase during PCa formation and is involved in the improvement of tissue stiffness in the PCa region.20Transrectal shear wave elastography(SWE) can be used to qualitatively and quantitatively analyze prostate tissue stiffness. The PCa region is generally stiffer than the surrounding normal tissue. Thus, abnormally stiffer regions in the prostate were characterized for targeted biopsy (Fig. 1, E). SWE could present a red-coded area suspicious of PCa with greater stiffness, which 2D-TRUS failed to identify. SWE could additionally characterize approximately 60%of the clinically significant PCa missed by MRI.The detection rate of PCa can be improved by 10%after combining SWE with MRI.21Compared to systematic biopsy, SWE-targeted biopsy could improve the detection rate of PCa. Moreover, SWE can effectively predict PCa extracapsular extension, although negative manifestations cannot entirely exclude extracapsular extension.22However, the instability and dependence of SWE on operators limit its potential for wide clinical use.23In addition,SWE is usually used to assess the stiffness of the outer glands, but it is difficult to accurately measure the stiffness of the inner glands.
5. Transrectal real-time strain elastography (TRSE)
Transrectal real-time strain elastography(TRSE)is another technique used to analyze tissue stiffness.Unlike SWE,TRSE must be performed by applying additional pressure on tissues and assessing stiffness based on the degree of tissue deformation.24Similarly, abnormal regions, especially asymmetrically stiffer regions detected by TRSE in the prostate,could be characterized by targeted biopsy (Fig. 1, F). Previous research has shown that TRSE-targeted biopsy could improve the detection rate of PCa by 18.3%–24.8%. By combining TRSE-targeted biopsy with systematic biopsy, the negative predictive value for high-risk PCa can be improved from 79%to 97%.25Moreover,the study conducted by Kamoi et al.proposed the“TRSE 5-point”method,taking 3-point as the cut-off value to differentiate the presence from the absence of PCa; the sensitivity,specificity,and accuracy were 68%,81%,and 76%,respectively.26Similar to SWE, TRSE can also accurately predict the extracapsular extension of PCa.However,TRSE has limitations in detecting small PCa lesions and may miss PCa with a low Gleason score.27In addition,TRSE has limitations in identifying suspicious lesions owing to its high dependence on operators.28
6. Three-dimensional transrectal ultrasonography (3D-TRUS)
Three-dimensional transrectal ultrasonography (3D-TRUS) has emerged as a novel imaging technique in prostate-targeted biopsy to provide a precise anatomic localization(Fig.3). The 3D-TRUS helps acquire 3D images and remediates the shortage of 2D-TRUS for measuring the volumes of lesions. Moreover, 3D-TRUS can cover large regions of interest, including peripheral blood vessels.29The 3D model of a real-time puncture route was reconstructed to record the position of the puncture needle and to perform a targeted biopsy more visually and accurately.30Therefore, 3D-TRUS is often a better choice for repeated biopsies and for identifying lesions, especially small target lesions.Compared with 2D-TRUS, 3D-TRUS with a higher localizing accuracy could improve the efficiency of MRI-ultrasound fusion/cognitive targeted biopsy and increase the rate of PCa detection.29,30However, a complex reconstruction operation is still a deficiency of 3D-TRUS,which awaits further improvement.

Fig. 3. Three-dimensional transrectal ultrasonography (3D-TRUS). (A) Coronal plane; (B) Sagittal plane; (C) Cross section; (D) Prostate 3D reconstruction.
In conclusion, with the development of multimodal ultrasound,various ultrasound techniques are widely used in prostate-targeted biopsies. Many studies have shown that multimodal ultrasound-targeted biopsy could effectively improve the rate of PCa detection. Although at present, MRI-targeted biopsy guided by 2D-TRUS is the mainstream technique in prostate-targeted biopsy, multimodal ultrasound is a reliable auxiliary technique to supplement the deficiency of MRI. It is essential to understand that multimodal ultrasound is not merely an auxiliary technique and is more likely to become the mainstream in targeted biopsy in near future as a positive prospect in clinical application. Although, the role of multimodal ultrasound in prostate-targeted biopsy still needs further exploration and confirmation.
Declaration of competing interest
No conflict of interest exists in the submission of this manuscript,and all authors have approved the manuscript for publication.
 Journal of Interventional Medicine2022年3期
Journal of Interventional Medicine2022年3期
- Journal of Interventional Medicine的其它文章
- A review of high-intensity focused ultrasound as a novel and non-invasive interventional radiology technique
- Ultrasound-guided microwave ablation for symptomatic adenomyosis: More areas of concern for more uniform and promising outcomes
- Balloon-occluded retrograde transvenous obliteration with lauromacrogol sclerosant foam for gastric varices
- A canine model of aortic arch aneurysm created with autologous pericardium
- Diagnosis of hepatic inflammatory pseudotumor by fine-needle biopsy
- Efficacy of contrast-enhanced ultrasound-guided percutaneous core needle biopsy in anterior mediastinal masses
