Impact of sarcopenia on tumor response and survival outcomes in patients with hepatocellular carcinoma treated by trans-arterial (chemo)-embolization
Gael Roth, Yann Teyssier,Maxime Benhamou, Melodie Abousalihac, Stefano Caruso, Christian Sengel, OlivierSeror,Julien Ghelfi, Arnaud Seigneurin, Nathalie Ganne-Carrie, Elia Gigante, Lorraine Blaise, Olivier Sutter,Thomas Decaens,Jean-Charles Nault
Abstract
Key Words: Hepatocellular carcinoma; Transarterial chemoembolization; Bland embolization; Sarcopenia;Skeletal muscle index
INTRODUCTION
Liver cancer is the second cause of cancer-related deaths worldwide[1], mostly represented by hepatocellular carcinoma (HCC). At the diagnosis, 70% of HCC patients have only access to palliative treatments, and among intermediate HCC, classified as Barcelona Clinic of Liver Cancer (BCLC)-B[2],transarterial chemoembolization (TACE) and transarterial embolization (TAE) are the best therapeutic options to offer[3-5]. Nonetheless, despite a good level of tumor response, around 50%-55% of patients receiving these treatments suffer from a high level of relapse[6]. It is well demonstrated that TACE presents the best results on patients with a good general status and a low level of liver insufficiency[7],but additional reliable predictive markers are needed to better define which patients will take full benefit of this procedure, and which ones present an increased risk of low efficacy and liver deterioration. At the diagnosis, more than 90% of HCC patients present with cirrhosis, a clinical condition often associated to malnutrition with sarcopenia. Indeed, sarcopenia, defined as the “progressive loss of muscle mass and strength with a risk of adverse outcomes such as disability, poor quality of life, and death”[8], is a consequence of chronic inflammation, hypercatabolism, and anorexia found in cirrhosis and advanced tumor stages. Sarcopenia has already been described as a poor prognostic factor in HCC patients undergoing surgical resection or treated by systemic therapies[9-12]. Further studies are needed to clarify the predictive value of sarcopenia in other HCC treatment settings, such as TAE or TACE.Indeed, several studies with small numbers of patients showed interesting results on the predictive value of sarcopenia regarding survival outcomes of patients treated by TACE but without clear impact on tumor response[13]. This study aimed to evaluate the predictive value of sarcopenia for tumor response and survival outcomes in a bicentric cohort of HCC patients treated by TACE or TAE.
MATERIALS AND METHODS
Patient selection
Patients were retrospectively included from December 1, 2007 to November 1, 2013 in Jean Verdier Hospital and from June 1, 2011 to December 1, 2014 in Grenoble-Alpes University Hospital. The inclusion criteria were as follow: Age > 18 years, HCC diagnosed by histology or non-invasive criteria[7], first treatment using TAE or TACE, and available pre- and post-therapeutic computed tomography(CT) scan. Transarterial procedures performed for acute bleeding of HCC were excluded.
Transarterial procedures
Patients were treated with transarterial therapy following standard local protocol[14]. Each indication of TACE or TAE was validated during multidisciplinary tumor board including a hepatologist, an interventional radiologist, and a liver surgeon. In case of TACE, chemotherapy was either doxorubicin or idarubicin according to institutional standards of care, as previously described[15]. The choice of chemotherapy was left to the investigator’s discretion. Every TACE or TAE was performed by an expert interventional radiologist.
As recommended by European guidelines, TACE could be repeated 2 mo after the first treatment in case of partial response on postoperative scan and preserved liver function after rediscussion in multidisciplinary tumor board[7].
Ethical approval
Written consent was obtained for every patient before transarterial procedures and the study protocol respects the ethical guidelines of the 1975 Declaration of Helsinki (6threvision, 2008). Study ethics was also approved by the independent French ethic committee CERIM (Comité d’éthique de la recherche en imagerie médicale;No. CRM-2004-084).
Clinical and paraclinical data collection
Clinical and biological data were recorded before the treatment: Demographic data, body mass index,liver function, platelets, presence of cirrhosis, etiology of the underlying liver disease, alpha-fetoprotein(AFP) level, tumor size, number of nodules, tumor portal invasion, and esophageal varices at the last upper endoscopy.
After the first treatment, all patients were prospectively followed until death or the last recorded visit until June 30, 2018.
Anthropometric measurements
Anthropometric measurements were assessed on the pre-therapeutic CT scan and the first follow-up CT scan realized 1-3 mo after the transarterial treatment by two radiologists (OSu and YT) using the software Image J®. Skeletal muscle and psoas muscle area were measured on a cross-sectional CT image at the level of the 3rdlumbar vertebra. Skeletal muscle index (SMI) was calculated using the total muscle area on the L3 CT slice divided by squared height as previously described[16]. Sarcopenia was defined by SMI < 50 cm2/m2in male and < 39 cm2/m2in female patients as defined by the North American expert statement on sarcopenia in liver transplantation[17]. Psoas muscle index (PMI) defined as the psoas muscle area on height ratio was also assessed as previously described[17].
The following data were recorded on imaging: Liver volume, spleen volume, presence of ascites at imaging, presence of para-umbilical vein, presence of esophageal varices, and presence of splenomegaly defined by a spleen’s cranio-caudal diameter superior to 12 cm.
Assessment of tumor response and survival outcomes
All imaging examinations were archived in a picture archiving and communication system and blindly read by two radiologists (OSu and YT). Clinical and paraclinical parameters were extracted from the patient’s electronic medical records.
Radiological response was assessed by two radiologists (OSu and YT) comparing the baseline imaging and the imaging available 1-3 mo after the first session of trans-arterial treatment as recommended[7]. Radiological response was classified into complete response, partial response, stable disease, and progressive disease as defined by the modified RECIST criteria[7].
Progression-free survival was defined as the time between the date of the first treatment and the date of death, radiological progression, or the last recorded visit. Patients were censured at the date of liver transplantation. Overall survival (OS) was defined as the time between the date of the first treatment and the date of death or the last recorded visit, with censoring at the date of liver transplantation in transplanted patients.
Statistical analysis
Categorical variables were compared using the Fisher exact test for two groups and Chi squared test for three groups and more. Continuous variables were compared using the Mann-Whitney test. Logistic regression was used to compare the association with radiological response and baseline variables.
Survival outcomes as OS and progression free survival (PFS) were computed using the Kaplan-Meier method, and the Log-rank test was used to compare survival rates. The association between baseline variable and OS and PFS was assessed in univariate analysis using the Cox model. Variables with aPvalue < 0.05 in the univariate analysis were computed in multivariate analysis using the Cox model.Statistical analyses were performed using Graph Pad (PRISM) and R software.
RESULTS
Description of the population
A total of 225 patients were included in the analysis, including 93 from Jean Verdier Hospital and 132 from Grenoble-Alpes University Hospital (Figure 1). Patients were mainly male (88.8%) with a median age of 65 (58-75) years old. The underlying liver diseases were mainly related to chronic alcohol intake(61%), hepatitis C (28%), and non-alcoholic steatohepatitis (29%) with 81.6% of patients classified as Child-Pugh A.
HCCs were classified as BCLC-A in 27.5%, BCLC-B in 55.5%, and BCLC-C due to segmental portal vein thrombosis in 16.8% of patients. One hundred and fifty-four (68.4%) of the patients were treated by TACE (127 with doxorubicin and 27 with idarubicin; including 87 by lipiodol TACE and 40 by TACE using drug eluting beads). Seventy-one (31.5%) patients were treated by TAE using lipiodol with gelatin sponge. Patients’ characteristics are detailed in Table 1.
Anthropometric and portal hypertension assessment at imaging
Anthropometric measurements including the value of total muscle area in L3 and psoas area in L3 are detailed in Table 1. Ascites was identified in 23.5% of the cases at imaging as well as splenomegaly in 57% of the cases, umbilical vein repermeabilization in 36.4%, and esophageal varices in 71.1%. About 57.7% (n= 130) of the patients had sarcopenia based on the SMI. The value of psoas area/squared height(cm2/m2) was significantly positively associated with body mass index (BMI), liver volume, albumin,alcohol intake, male, and non-alcoholic steatohepatitis (NASH), and negatively associated with age and hepatitis C virus (Figure 2A). Sarcopenia at imaging (defined by SMI < 50 cm2/m2in male and < 39 cm2/m2in female patients) was observed in 130 (57.7%) patients.
Sarcopenic patients were significantly older (67.5 years oldvs62.5 years old;P=0.0338), with a lower BMI (24.3vs28.7P< 0.0001) and a higher median serum AFP level (11.5 ng/mLvs7.7 ng/mL;P=0.0152) compared to non-sarcopenic patients at imaging (Table 1 and Figure 2B). Sarcopenia was also associated with a higher tumor burden (sum of the size of the 2 main tumors) and a lower BMI, ALAT level, and spleen volume, and was less frequent in alcohol-related cirrhosis and in NASH patients(Figure 2B). At the first radiological assessment, 28.7% of the patients with sarcopenia harbored an increase in Child-Pugh Class (A to B/C or B to C) compared to 24.53% of patients without sarcopenia (P= 0.6862, Fisher exact test). Patients’ baseline features as well as treatments following TACE or TAE,according to the presence or not of sarcopenia, are detailed in Table 1.
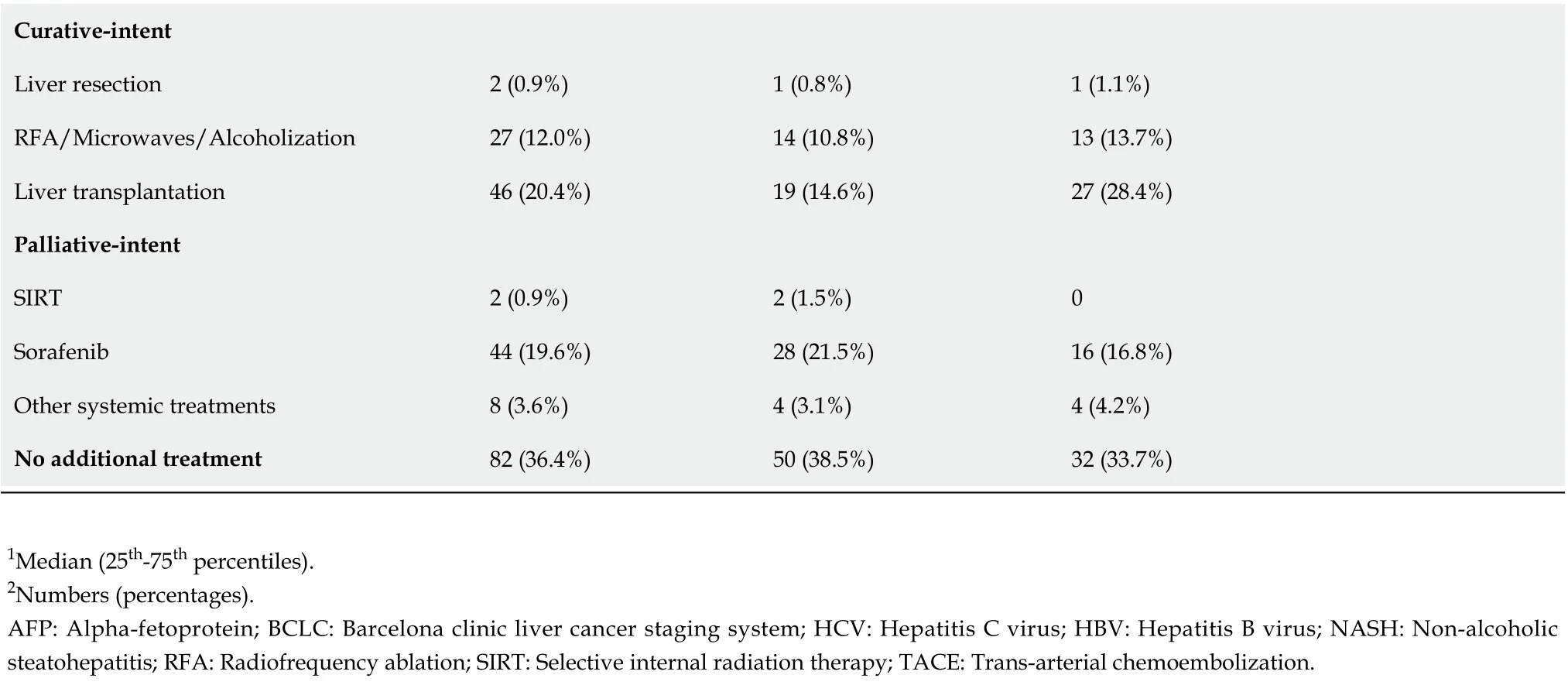
Relationship between sarcopenia and radiological response
At the first radiological evaluation after TACE or TAE, 23% (n= 52) of patients harbored a complete response, 39% a partial response (n= 88), 23% a stable disease (n= 52), and 15% (n= 33) a progressive disease based on mRECIST criteria. Presence of portal hypertension signs on endoscopy or imaging was not encountered as predictive markers of radiological response. Presence of sarcopenia had a significant impact on progression proportions after TACE (P= 0.0084, Chi square test Figure 3A). Whereas objective tumor response (complete and partial radiological response) was not statistically different in sarcopenic (64%) compared to non-sarcopenic patients (67%,P=0.66, Fisher exact test), a higher rate of progressive disease was observed in patients with sarcopenia compared to patients without (19%vs8%,P=0.0236, Fisher exact Test, Figure 3B). In univariate analysis, sarcopenia [odds ratio (OR): 2.59; 95%CI:1.16-6.40,P= 0.0274], serum AFP level (OR: 1.00029; 95%CI: 1.00008-1.0006,P= 0.0226), and BCLC-C stage (OR: 2.22; 95%CI: 1.25-4.05;P= 0.00758) were related to progressive disease at imaging. In multivariate analysis, only BCLC-C stage (OR: 1.98; 95%CI: 1.038-3.88,P= 0.0416) remained independently associated with a higher rate of progressive disease.
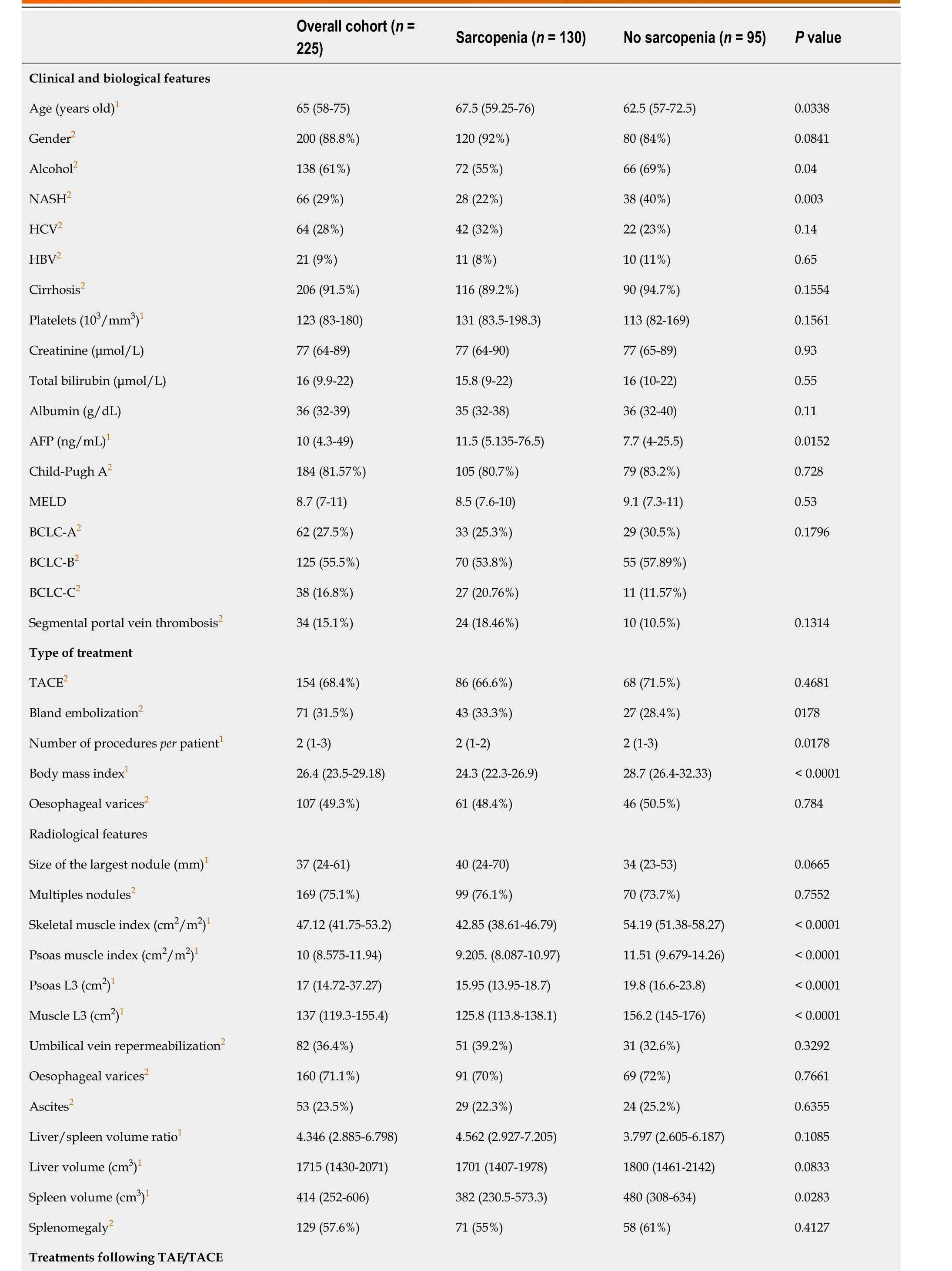
Table 1 Description of population features according to presence of sarcopenia or not
Curative-intent Liver resection 2 (0.9%)1 (0.8%)1 (1.1%)RFA/Microwaves/Alcoholization 27 (12.0%)14 (10.8%)13 (13.7%)Liver transplantation 46 (20.4%)19 (14.6%)27 (28.4%)Palliative-intent SIRT 2 (0.9%)2 (1.5%)0 Sorafenib 44 (19.6%)28 (21.5%)16 (16.8%)Other systemic treatments 8 (3.6%)4 (3.1%)4 (4.2%)No additional treatment 82 (36.4%)50 (38.5%)32 (33.7%)1Median (25th-75th percentiles).2Numbers (percentages).AFP: Alpha-fetoprotein; BCLC: Barcelona clinic liver cancer staging system; HCV: Hepatitis C virus; HBV: Hepatitis B virus; NASH: Non-alcoholic steatohepatitis; RFA: Radiofrequency ablation; SIRT: Selective internal radiation therapy; TACE: Trans-arterial chemoembolization.
Relationship between sarcopenia before TACE and survival
The median progression-free survival was 9.4 mo. Patients with sarcopenia had a lower median PFS compared to patients without (8.3 movs13.2 mo,P= 0.0035, log rank test, Figure 4A). In univariate analysis, sarcopenia, tumor portal vein thrombosis, size of the largest nodule, serum AFP level, and platelet level were significantly associated with a lower PFS (Table 2). In multivariate analysis,sarcopenia [hazard ratio (HR): 1.62; 95%CI: 1.15-2.28], tumor portal vein thrombosis (HR: 1.77; 95%CI:1.11-2.83), size of the largest nodule (HR: 1.008; 95%CI: 1.002-1.013), and platelet level (HR: 1.002; 95%CI:1.002; 95%CI: 1.0001-1.005) remained independently associated with a lower PFS (Table 2).
The median OS was 24.3 mo. OS was shorter in patients with sarcopenia compared to patients without (19.4 movs35.5 mo,P= 0.0149, log rank test, Figure 4B). Sarcopenia, ascites at imaging, size of the largest nodule, serum AFP level, Child-Pugh score, and BMI were associated with OS at univariate analysis (Table 3). In multivariate analysis, sarcopenia (HR: 1.68; 95%CI: 1.04-2.72), AFP level (HR:1.0001; 95%CI: 1.00001-1.002), and size of the largest nodule (HR: 1.007, 95%CI: 1.0015-1.013) were independently associated with a higher risk of death (Table 3).

Table 2 Univariate and multivariate Cox analyses of baseline variables associated with progression-free survival
Evolution of sarcopenia after TACE and its impact on OS
Post-TACE SMI was assessed by CT scan at the first radiological assessment in 218 patients in order to assess the evolution of sarcopenia after treatment. Among the patients without sarcopenia at baseline,71 were still non-sarcopenic, and 22 became sarcopenic. Among the 22 patients who became sarcopenic,19 had a progressive disease at the first radiological assessment.
Patients with post-TACE sarcopenia presented a shorter median OS (n= 147, 18.15 mo) compared with non-sarcopenic patients (n= 71, 35.7 mo,P= 0.0019) (Figure 4C).

Table 3 Univariate and multivariate Cox analyses of baseline variables associated with overall survival
In non-sarcopenic patients at baseline, emergence of a post-TACE sarcopenia was associated with a significant shorter median OS of 17 mo when compared with already sarcopenic patients before TACE(19.3 mo) and patients who stayed non-sarcopenic along TACE procedure (36.43 mo,P= 0.0004)(Figure 4D).

Figure 2 Correlation of biological and clinical features with sarcopenia. A: Association of clinical, biological, and radiological features with skeletal muscle index expressed as a continuous variable; B: Association of clinical, biological, and radiological features with the presence or not of sarcopenia. Comparison of a continuous variable in two or more than two groups was performed using Wilcoxon signed-rank test or Kruskal-Wallis test, respectively. Qualitative data were compared using the Fisher’s exact test. Correlation analysis between continuous variables was performed using Spearman's rank-order correlation. All tests were two-tailed and a P-value < 0.05 was considered significant. BMI: Body mass index; HCV: Hepatitis C virus; NASH: Non-alcoholic steatohepatitis; SMI: Skeletal muscle index.
DISCUSSION
This study is the largest multicentric cohort study exploring the impact of sarcopenia on tumor response and survival outcomes in patients with HCC treated by TACE or TAE. Sarcopenia represents a major challenge in chronic diseases and especially in the treatment of cancers in which the general status is classically altered, and aggressive treatments with poor tolerance profiles are frequent. Sarcopenia in cirrhosis has already been described as impacting survival, confirming the need of a global approach with a close nutritional support of these patients. Sarcopenia measures were assessed on the open-access software Image J®, which has been proved as equivalently efficient as other commercial programs,meaning that radiological assessment of sarcopenia is accessible to every center[18]. The use of SMI was preferred to methods only based on the measurement of PMI or the transverse psoas muscle thickness.Even though the two latter are simple to assess and showed interesting results in term of survival in HCC patients treated by TACE in previous studies, SMI seems to offer a more robust and complete measurement of the muscle mass in cirrhotic patients. Besides, PMI may identify fewer patients at risk of an increased mortality and presents a higher inter-observer variability. To finish, SMI is easy to use and recommended by the North American Expert Opinion Statement on Sarcopenia in Liver Transplantation[17,19,20]. In this study, measures were performed by only one radiologistpercenter,which limits bias induced by potential interobserver variability. This also constitutes a limit as interobserver variability should be studied to improve result exportability and better evaluate their reproducibility.
Figure 3 Radiological response according to presence of sarcopenia. A: Complete response vs partial response vs stable disease vs progressive disease assessed using the mRECIST criteria after the first session of treatment; B: Complete and partial response and stable disease vs progressive disease assessed using the mRECIST criteria after the first session of treatment. Statistical analysis was performed using the chi square test. CR: Complete response; PR:Partial response; SD: Stable disease; PD: Progressive disease; TACE: Trans-arterial chemoembolization.

Figure 4 Survival according to presence of sarcopenia before and after trans-arterial chemoembolization. A and B: Progression free survival (A)and overall survival (OS) (B) according to the presence or not of sarcopenia before trans-arterial chemoembolization (TACE); C: OS according to presence or not of sarcopenia after TACE; D: OS according to the presence or not of sarcopenia before TACE, and appearance of sarcopenia after TACE designated as post-TACE sarcopenia. Results were computed using the Kaplan-Meier method and compared by the log rank test. The patients at risk are represented under the x-axis.
In this study, a high prevalence of sarcopenia (57%) in patients with HCC treated by transarterial treatment was observed despite the predominance of Child-Pugh A patients and intermediate stage tumors (BCLC-B). This is consistent with a recent HCC cohort study exploring the impact of sarcopenia on survival in patients treated by hepatectomy where 54% of patients were sarcopenic, as well as published data in liver transplantation[17]. Even if patients with sarcopenia have a lower BMI than patients without, most of patients with sarcopenia harbored a normal BMI (median value of 24).Moreover, with the increase of overweight and obesity which represents 15%-20% of the worldwide population[21], BMI is even less sensitive to detect malnutrition in patients with chronic diseases and especially liver diseases. These elements suggest that sarcopenia measured by performant radiological methods reflect more precisely the nutritional state and the protein catabolism of these patients.Nonetheless, other markers that could impact the outcomes after trans-arterial (chemo)embolization such as patient’s daily activities and diet are not collected in this study due to its retrospective character.As well, this study lacked of other frailty parameters such as grip strength or walking speed. It constitutes another limit that cannot be addressed due to the retrospective character of the study.
One of the main strengths of this study is the radiological reviewing of radiological response using mRECIST criteria. This analysis revealed that sarcopenia was associated with a higher risk of progressive disease after trans-arterial treatment but without any difference on objective tumor response. Nevertheless, in multivariate analysis, only BCLC-C (segmental portal thrombosis) was independently associated with progressive disease. Sarcopenia was also associated with a shorter PFS together with tumor size in multivariate analysis. These data suggest that a subgroup of patients with advanced tumor stage and sarcopenia have a more aggressive disease which is more prone to resist to trans-arterial treatments. Indeed, sarcopenia may reflect the consequences of an intense hypercatabolism due to a particularly aggressive disease. In these patients, transarterial treatment may be deleterious in addition to be less effective as it could lead to liver failure and decrease the possibility of using systemic treatments after progression. Besides, the increased rate of radiological response obtained with the recent combination atezolizumab-bevacizumab forces us to better select the optimal treatment for patients between TACE and systemic treatments[22]. However, as sarcopenia has also been associated with poorer survival outcomes in patients under systemic therapies[10], it remains to be studied if sarcopenic patients with a high tumor burden benefit more from systemic treatments than trans-arterial procedures. In any case, sarcopenia needs to be detected as early as possible to initiate a medical intervention using nutritional support and physical activity to reverse sarcopenia and potentially improve survival. Indeed, muscle restoration before starting these treatments showed interesting results in terms of survival[10,23], and this type of intervention should be tested in a randomized controlled trial as up to 60% of patients treated by TACE harbored sarcopenia.
Sarcopenia was also associated with a shorter OS independently of tumor burden, suggesting that undernutrition and loss of muscle are key prognostic factors in patients with HCC treated by TACE or TAE. As sarcopenia is easily assessable using a CT scan in clinical practice, it could be useful to stratify patients in clinical trials. This study showed that sarcopenia assessed at the first radiological evaluation after TACE was also associated with a shorter OS, underlying the robustness of this association.Moreover, a subset of patients rapidly developed sarcopenia at the first radiological assessment which was particularly associated with a poor OS. Almost all these patients presented a progressive disease at the first evaluation, suggesting that they harbored an aggressive tumoral disease potentially responsible for the fast development of sarcopenia.
CONCLUSION
In conclusion, sarcopenia is associated with a higher rate of tumor progression and shorter survival in patients with HCC treated by TACE or TAE. Moreover, sarcopenia is an easy-to-assess radiological biomarker of poor prognosis that should be measured in order to better estimate prognosis and test a targeted intervention mixing nutritional support and physical activity.
ARTICLE HIGHLIGHTS


Research objectives
This study aimed to evaluate the prognostic value of sarcopenia in patients with HCC treated by transarterial (chemo)-embolization based on baseline computed tomography (CT) findings and study its impact on objective tumor response and survival outcomes.
Research methods
Sarcopenia is easy to assess on CT by measuring the skeletal muscle index. A skeletal muscle index(SMI) < 50 cm2/m2in male and < 39 cm2/m2in female patients corresponding to sarcopenia was observed in 57.7% of the patients.
Research results
Based on SMI analysis measured on baseline imaging, sarcopenia was observed in 57.7% of the patients.After full review of radiological response using mRECIST criteria, sarcopenia was associated with a higher rate of progressive disease. It was also associated with a decrease overall survival even after adjustment with usual risk factors of death.
Research conclusions
Sarcopenia is an easy-to-assess radiological biomarker of poor prognosis that should be measured in order to better assess prognosis of HCC patients.
Research perspectives
Sarcopenia should be systematically detected at baseline, and induce a targeted intervention mixing nutritional support and physical activity. Further studies are needed to assess the benefit of these strategies in HCC patients.
FOOTNOTES
Author contributions:Roth G, Teyssier Y, Decaens T, and Nault JC equivalently contributed to this work; Roth G,Decaens T, and Nault JC contributed to the conceptualization; Roth G and Nault JC contributed to the methodology;Roth G, Teyssier Y, Benhamou M, Abousalihac M, Sengel C, Seror O, Ghelfi J, Ganne-Carrié N, Gigante E, Blaise L,Sutter O, Decaens T, and Nault JC contributed to the investigation; Roth G, Benhamou M, Teyssier Y, Abousalihac M,and Nault JC contributed to the formal analysis; Roth G, Nault JC, Seigneurin A, and Caruso S contributed to the data curation; Nault JC, Seigneurin A, and Caruso S contributed to the statistical analysis; Roth G, Teyssier Y,Benhamou M, Caruso S, Seigneurin A, Abousalihac M, Sengel C, Seror O, Ghelfi J, Ganne-Carrié N, Gigante E, Blaise L, Sutter O, Decaens T, and Nault JC contributed to the validation; Decaens T and Nault JC contributed to the resources; Roth G and Nault JC wrote the original draft; Roth G, Teyssier Y, Benhamou M, Seigneurin A, Abousalihac M, Sengel C, Seror O, Ghelfi J, Ganne-Carrié N, Gigante E, Blaise L, Sutter O, Decaens T, and Nault JC reviewed and edited the manuscript; Roth G, Decaens T, and Nault JC contributed to the supervision; all authors have read and approved the manuscript.
Institutional review board statement:The study was conducted according to the guidelines of the Declaration of Helsinki. Study ethics was approved by the independent French ethic committee CERIM (Comité d’éthique de la recherche en imagerie médicale) (approval date May 252020; No. CRM-2004-084).
Informed consent statement:Patients gave their written consent before TACE procedures as in routine care practice.No specific consent statement was required regarding the retrospective analysis of data as they were anonymously used.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:No additional data are available.
STROBE statement:The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:France
ORCID number:Gael Roth 0000-0001-5822-4320; Yann Teyssier 0000-0002-9785-8729; Maxime Benhamou 0000-0002-8590-5161; Mélodie Abousalihac 0000-0002-0661-1684; Stefano Caruso 0000-0002-6319-3642; Christian Sengel 0000-0001-9004-256X; Olivier Seror 0000-0001-6680-8991; Julien Ghelfi 0000-0002-9039-6488; Arnaud Seigneurin 0000-0002-2168-1672;Nathalie Ganne-Carrie 0000-0002-7351-5027; Elia Gigante 0000-0002-5455-2308; Lorraine Blaise 0000-0001-5344-1625;Olivier Sutter 0000-0002-2802-9652; Thomas Decaens 0000-0003-0928-0048; Jean-Charles Nault 0000-0002-4875-9353.
S-Editor:Fan JR
L-Editor:Wang TQ
P-Editor:Cai YX
 World Journal of Gastroenterology2022年36期
World Journal of Gastroenterology2022年36期
- World Journal of Gastroenterology的其它文章
- Nonalcoholic steatohepatitis and hepatocellular carcinoma: Beyond the boundaries of the liver
- Early extrahepatic recurrence as a pivotal factor for survival after hepatocellular carcinoma resection: A 15-year observational study
- SARS-CoV-2 and the pancreas: What do we know about acute pancreatitis in COVID-19 positive patients?
- Esophageal magnetic compression anastomosis in dogs
- Liver-specific drug delivery platforms: Applications for the treatment of alcohol-associated liver disease
- P2X7 receptor as the regulator of T-cell function in intestinal barrier disruption
