Esophageal magnetic compression anastomosis in dogs
Xiang-Hua Xu, Yi Lv, Shi-Qi Liu, Xiao-Hai Cui, Rui-Yang Suo
Abstract
Key Words: Magnetic; Anastomosis; Esophagus; Reconstruction; Hand sewn; Dog
INTRODUCTION
Esophageal atresia (EA) is a serious and fatal gastrointestinal developmental malformation in the neonatal period. It has a worldwide prevalence of 2.4 to 3.8 per 10000 newborns[1-4]. Because of the development of surgical and good neonatal intensive care, the survival is about 90% in those born with EA with severe associated anomalies and is even higher in those born with EA alone[5]. However, the postoperative complications of traditional hand-sewn anastomosis are numerous, and the therapeutic effect is not good. The primary complications during the postoperative period are leakage (incidence 15%-20%), stenosis of the anastomosis (30%-40%), gastroesophageal reflux (40%-65%), esophageal dysmotility, fistula recurrence, scoliosis, deformities of the thoracic wall and respiratory disorders[6-8].After surgery, children suffer from various complications, which seriously affect their development and quality of life.
Magnetic compression anastomosis (MCA) is a novel suture-free reconstruction of the digestive tract.Since Kanshinet al[9] reported using a magnetic device to anastomose gastroduodenal and cecojejunal in dogs in 1978, there have been many reports of this technique using animal experiments and regarding its clinical applications. At present, clinically, it has been used in gastrointestinal anastomosis[10,11],jejunal anastomosis[12,13], cholangioenteric anastomosis[14-16] and so on. Fourteen patients underwent MCA for gastrointestinal anastomosis, and the technical success of MCA was achieved in 100% of the cases. Two patients underwent anastomotic restenosis, and 1 patient had an anastomotic perforation due to balloon dilatation to prevent restenosis. Fifteen patients underwent MCA for jejunal anastomosis,of which five patients had severe systemic disease and underwent complex open urinary reconstruction procedures. The device was successfully placed and effectively formed a side-to-side, functional end-toend jejunal anastomosis. Forty-seven patients underwent MCA for cholangioenteric anastomosis.Thirty-eight patients had a malignant primary disease, while nine had benign disease. With a median follow-up of 547.5 d (range 223-1042 d), no patients had biliary fistula, while two developed anastomotic stricture at 4 mo and 14 mo after surgery. Magnetic materials have noncontact suction characteristics that will greatly simplify the process of gastrointestinal anastomosis, especially in the case of gastrointestinal stenosis or atresia. Recently, Kamadaet al[10] reported that MCA without general anesthesia is a valuable alternative to surgery for gastrointestinal obstruction. Some patients with biliary obstruction are not eligible for conventional endoscopic procedures or are unsuitable for surgery. The MCA technique is an available method for performing choledochocholedochostomy and choledochoenterostomy interventionally[16]. The mean age of the patients in these two reports was above 60 years. Therefore, MCA technology can be designed as a minimally invasive technique and is tolerated by elderly patients.
Because of the many complications of traditional operations and the ability to obtain minimally invasive surgery by MCA, MCA could be a superior method to treat congenital EA. There have been several clinical reports on esophageal reconstruction using MCA[17-19]. Muenstereret al[17] reported that they used esophageal MCA for staged EA repair in 3 patients (Gross type A, B, and C) at high risk for conventional surgical repair. Surgeries were all successful, and there were no perioperative complications. Liuet al[18] reported that two patients who had severe stricture after simultaneous EA and duodenal obstruction repair underwent magnetic compression stricturoplasty. Magnetic compression stricturoplasty successfully established the patency of the esophagus in these two patients with refractory EA stricture. These two cases required multiple additional procedures, but durable esophageal patency with absence of dysphagia was achieved at 15 or 10 mo after magnetic compression stricturoplasty. Dormanet al[19] reported a case in which EA was repaired with a proximal fistula using endoscopic MCA after staged lengthening. Magnetic coupling occurred at 4 d, and after magnet removal at 13 d, an esophagram demonstrated a 10 French channel without leakage. A series of studies on MCA technology have been carried out in our laboratory. The technology has been used in choledochojejunostomy, rectovaginal fistula repair, laparoscopic pancreatoduodenectomy (LPD) and liver transplantation. Twenty-six mongrel dogs underwent choledochojejunostomy magnamosis with different magnetic pressure magnets. The surgical procedures were all successful[20]. There was a comparative study with 12 pigs for rectovaginal fistula repair. Eight animals were in the MCA group,and four animals were in the hand-sewn group. The rectovaginal fistula site was smooth, and healing was complete. This technology was used in one case clinically and achieved success[21]. Seven patients received MCA technology in LPD. LPD was successfully completed in all seven patients, of which seven underwent laparoscopic magnetic compression choledochojejunostomy and two received laparoscopic magnetic compression pancreatojejunostomy. No leakages were observed after the operation. After a median follow-up period of 11 mo (range 4-18 mo), there was no incidence of anastomotic stricture[22].We also used MCA to reconstruct vessels in liver transplantation. In pig liver transplantation, we used MCA to reconstruct the suprahepatic vena cava, infrahepatic vena cava and portal vein. They were all successful, and the pig lived for over one month[23]. Currently, we want to use MCA technology to treat EA, but there is a paucity of published research data and animal studies. Therefore, the purpose of this study was to study the difference between MCA and hand-sewn anastomosis of the esophagus in dogs.
MATERIALS AND METHODS
Animals
The protocol of the animal study was reviewed and approved by the committee for Ethics of Animal Experiments of Xi’an Jiaotong University (No. XJTULAC2020-1441). Thirty-six mongrel dogs (male = 18,female = 18) with body weights of 10-15 kg were provided by the Laboratory Animal Center of Xi’an Jiaotong University. Dogs were acclimatized to laboratory conditions (23 °C, ad libitum access to food and water) for 2 wk prior to experimentation. In this study, we selected mongrel dogs because the esophagus in the neck is long enough for reconstruction. This purpose is to avoid performing surgery in the thoracic cavity and to improve the survival rate.
Study design
Thirty-six dogs were randomized into either the MCA group or the hand-sewn group,n= 18 per group,with the same male to female ratio. The dogs in the MCA group were subjected to end-to-end esophageal anastomosis with the magnetic device, while those in the hand-sewn group underwent hand-sewn anastomosis with 4-0 absorbable multifilament Vicryl. We used interrupted single-layer sutures. In both groups, there was no surgical left in place. Postoperative complications and weight were observed. The anastomosis time, gross appearance and pathology of the anastomoses were evaluated at one month, three months and six months after the operation.
Magnetic anastomosis device
The magnetic anastomosis device used in the study possessed a parent magnetic ring (PMR) and daughter magnetic ring (DMR), which were made of rare earth neodymium iron boron (NdFeB, N40)and plated with nickel from Northwest Institute for Nonferrous Metal Research, Xi’an, China. A special drainage tube was placed between the PMR and DMR, and both the PMR and DMR had outer diameters of 20 mm, inner diameters of 14 mm, and thicknesses of 2 mm. The magnetic force between the PMR and DMR is 30 Newton at zero distance with a magnetic density of 8000 GS.

Figure 1 Surgical procedures of magnetic compress esophagus anastomosis. A: Transecting the esophagus at the diseased region; B: Placing the parent magnetic ring (PMR) and daughter magnetic ring (DMR) on the upper and lower ends of esophagus; C: The PMR and DMR attract each other and create the anastomosis, and the esophagus reconstruction is complete, the dispositive allows food passage; D: The magnetic devices fall off the esophagus into the stomach,and the esophagus lumen is completely open.

Figure 2 The magnetic device and the appearance on X-ray, the esophageal anastomosis of magnetic compression anastomosis and hand-sewn suture. A: The magnetic device, composed of two magnetic rings and one special catheter; B: The magnetic ring position on X-ray postoperatively,and the anastomosis face is smooth; C: Using the magnetic compression anastomosis technology to finish the esophageal anastomosis; D: The anastomosis by hand-sewn suture.
Surgical procedures
The dogs were first anesthetized with an intraperitoneal injection of 30 mg/kg pentobarbital sodium solution. The dogs were anesthetized and then placed in the right lateral position on a temperaturecontrolled operating table with their cervical region shaved and sterilized. The experimental process is shown in Figure 1. A 5 cm incision was made along the anterior edge of the sternocleidomastoid muscle in the neck. Then, the muscle was separated layer by layer, and a 3 cm long portion of the esophagus was found. Next, the esophagus was transected.
In the MCA group, the PMR and DMR were placed in the upper and lower esophagus, respectively,after transecting the esophagus (Figure 1A). The magnetic anastomosis device was shown in Figure 2A.The upper and lower ends of the esophageal anastomosis were sutured with 4-0 silk thread and tightened to the position of the special drainage tube. Under the action of attraction, the magnetic rings at both ends are attracted to each other automatically and press the anastomotic tissue together, and the esophageal anastomosis is then completed (Figure 2C). When the anastomotic tissue is necrotic and falls off, the magnetic device is discharged into the stomach with the digesta and is discharged out of the body. In the control group, the operation was the same as that in the study group, except that end-toend anastomosis was performed with 4-0 absorbable sutures (Figure 2D).
Postoperative care
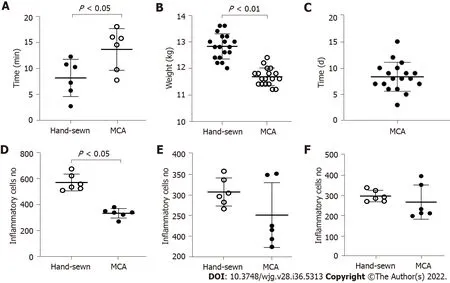
Figure 3 The analysis about anastomosis time, weight changes, the time of the magnetic device fell and the number of inflammatory cells between two groups. A: The anastomosis time of the magnetic compression anastomosis group and hand-sewn group. There were 18 dogs in each group; B:The dogs were weighed at 1 mo, and every group contained 6 dogs. There was a significant difference between the two groups; C: The time when the magnetic device had fallen into the stomach of 18 dogs; D-F: The number of inflammatory cells respectively at 1 mo, 3 mo and 6 mo. MCA: Magnetic compression anastomosis.
An X-ray (Perlove Medical Equipment incorporated company, Nanjing, China) was performed on the dogs in the study group to confirm the target location and precise mating of the magnetic compression rings (Figure 2B). X-ray was performed every day before the magnets fell off the esophagus. Postoperatively, every dog was kept in a cage. After the surgery, the dogs in the two groups were fasted for two days and then started on enteral nutrition. However, in the hand-sewn group, dogs generally showed poor appetite and even refused to eat. They started enteral nutrition at 4 d, 5 d, or even longer. During this period, we can only keep them alive with parenteral nutrition. The dogs in the MCA group started enteral nutrition earlier than those in the hand-sewn group. All dogs in both groups were given cefazolin sodium intramuscularly for 3 d postoperatively to prevent infection. Intramuscular injection(0.5 g) was administered twice a day. After a week, dogs were given enteral nutrition, a liquid diet, a semiliquid diet, and a normal diet according to their recovery. Six dogs were randomly selected in each group at 1 mo, 3 mo and 6 mo after the operation. They were weighed and intravenously injected with an overdose of anesthetic.
Specimen collection and histological analysis
All anastomosis segments with a sufficient length were harvested. The anastomotic stoma was found and severed 2 cm above and below the anastomosis. The gross information was observed, and all samples were immersed in 10% buffered formalin overnight. The samples were embedded in paraffin after fixation. Four-micrometer-thick sections were cut at the anastomosis site. Sections were stained with hematoxylin and eosin and Masson’s trichrome dye. Then, we observed the changes in the tissue and cells under a light microscope.
Statistical analysis
Data were analyzed using GraphPad Prism v8 software (GraphPad, La Jolla, CA, United States).Quantitative data are expressed as the mean ± SD, and differences between the two groups were analyzed with the independent samplesttest. The anastomosis time and weight data conformed to a normal distribution and homogeneity of variance. Statistical significance was set atP< 0.05.
RESULTS
Procedural parameters
Anastomosis was successfully created in all dogs. The anastomosis time of the MCA group was shorter than that of the hand-sewn group (7.5 ± 1.0vs12.5 ± 1.8,P< 0.01) (Figure 3A). X-ray examinations showed that the esophagi were all unobstructed and that the contrast agent could pass through the anastomosis in the MCA group. All dogs survived. There was one dog in the hand-sewn group and one dog in the MCA group with stenosis after the operation. These were found when we obtained anastomotic stoma tissue. We observed one dog in the hand-sewn group who suddenly refused to eat,and the incision skin was red, swollen and purulent 8 d after the operation. We performed surgical exploration and performed a second esophageal reconstruction.

Figure 4 Gross appearance of the anastomosis in magnetic compression anastomosis and hand-sewn group. A: The tissue of magnetic compression anastomosis (MCA) group is thin at 1 mo, but the mucous membrane is intact; B: Anastomotic tissue of the MCA group at 3 mo; C: At 6 mo, the tissue becomes smooth and flat in the MCA group. There is little difference from normal tissue; D: The tissue of the hand-sewn anastomotic stoma is incomplete, and the mucous membrane has a small pinhole at 1 mo, which was caused by the suture needle. Red arrow indicates; E: Anastomotic tissue of the hand-sewn group at 3 mo;F: Anastomotic tissue of the hand-sewn group at 6 mo.
Expulsion time of the magnetic compression rings and weight changes
We observed how long the magnetic rings took to fall off into the stomach. The mean time was 8.3 ± 2.7 d (range 3-15 d) (Figure 3C). The weights of dogs in the MCA group (13.87 ± 0.63 kg) and the hand-sewn group (13.98 ± 0.80 kg) were similar at the beginning of the experiment. The difference in weight between the two groups was not statistically significant. However, the weights decreased more in the hand-sewn group than in the MCA group 1 mo after the operation. The mean weight of the MCA group was 12.73 ± 0.80 kg, while the mean weight of the hand-sewn group was 11.63 ± 0.71 kg,P< 0.05. At 3 mo and 6 mo after the operation, the dog weights were similar between the two groups (13.75 ± 0.84 kgvs14.03 ± 0.82 kg, 14.93 ± 0.80 kgvs15.44 ± 0.47 kg).
Gross appearance of the anastomosis
The esophagi grew well, and there were no ulcerations or fistulas. The mucosa layers were intact.However, the anastomotic stomas were slightly thinner than the peripheral tissue at 1 mo. We could see that the muscle layer tissues were not completely covered. In the hand-sewn anastomosis group, the suture plots were still visible 1 mo after the operation (Figure 4D). With the passage of time, the submucosa and muscle layers were gradually covered, and the anastomoses became increasingly smooth and flat. However, at 1 mo, 3 mo and 6 mo, the anastomoses of the MCA group were smoother than those of the hand-sewn group.
Histological appearance of the anastomosis

Figure 5 Hematoxylin and eosin dye of the anastomotic tissue in magnetic compression anastomosis and hand-sewn group. Each image consists of two parts, one with a 2 × objective view and the other with a 40 × objective view. A: The anastomotic tissue of the magnetic compression anastomosis(MCA) group at 1 mo. The mucous membrane was intact, but the muscularis was separated; B: The anastomotic tissue of the hand-sewn group at 1 mo. There were more inflammatory cells in the tissue of the hand-sewn group than that of the MCA group; C: The anastomotic tissue of the MCA group at 3 mo. The muscularis became continuous; D: The anastomotic tissue of the hand-sewn group at 3 mo; E: The anastomotic tissue of the MCA group at 6 mo; F: The anastomotic tissue of the hand-sewn group at 6 mo.
Light microscopy showed that the anastomotic mucosa of the MCA group had grown well during the first month after surgery, while the submucosal and muscular layers were still fractured (Figure 5A).Three months after the operation, the submucosal and muscular layers had completely covered the anastomoses, and the anastomotic tissue was similar to the normal esophageal tissue under light microscopy (Figure 5C). In the hand-sewn group, the mucosa was continuous one month after surgery,but the submucosa and muscle layers were still broken, similar to the findings in the MCA group at one month (Figure 5B). At 3 mo postoperatively, the anastomotic site was covered by the submucosa and muscularis (Figure 5D). The number of inflammatory cells in the hand-sewn group was greater than that in the MCA group at 1 mo (Figures 5A and B). We counted the number of inflammatory cells in one high-power field (40 ×) in both groups (334 ± 37vs572 ± 65,P< 0.01). At 3 mo and 6 mo, the number of inflammatory cells was less than that at 1 mo. Between the two groups, the number of inflammatory cells was equal at 3 mo and 6 mo (Figures 5C-F). Masson staining showed that the number of collagen fibers in the hand-sewn group was greater than that in the MCA group. The blue fibers are collagen fibers (Figures 6A-F).
DISCUSSION
We studied the tissue status of the anastomotic esophagus after esophageal reconstruction by magnetic anastomosis technology and clarified the safety of MCA surgery. A comparative study was conducted between magnetic anastomosis and hand-sewn anastomosis for esophageal reconstruction to determine whether the effects of MCA were superior to those of the hand-sewn method.
By observing gross specimens and tissue sections at different time periods in the MCA and handsewn groups, we found that in both the MCA group and the hand-sewn anastomosis group, the anastomotic tissues were not completely healed at 1 mo after surgery. The mucosal surface of the two groups was smooth without ischemia or necrosis, while some submucosa and muscularis were still missing. After 3 mo, the anastomotic sites of the two groups had healed well, and the mucosal layer,submucosal layer and muscular layer were continuous. Liquid food is still the main diet in the early stage to reduce the stimulation of esophageal mucosa and prevent the occurrence of ulcers. Based on the results of the experiment, we suggest that MCA patients should consume a liquid diet or a semiliquid diet for at least one month.

Figure 6 Masson Thrichrome dye staining of the anastomotic tissue in magnetic compression anastomosis and hand-sewn group. Each image consists of two parts, one with a 2 × objective view and the other with a 40 × objective view. A: The anastomotic tissue of the magnetic compression anastomosis (MCA) group at 1 mo. The mucous membrane was intact, but the muscularis was separated at 1 mo, and the appearance was similar to that of hematoxylin and eosin staining; B: The anastomotic tissue of the hand-sewn group at 1 mo. There were more collagenous fibers than that in MCA group; C: The anastomotic tissue of the MCA group at 3 mo. The muscularis became continuous; D: The anastomotic tissue of the hand-sewn group at 3 mo; E: The anastomotic tissue of the MCA group at 6 mo; F: The anastomotic tissue of the hand-sewn group at 6 mo.
The tissue healing of the MCA group was faster and better than that of the hand-sewn group. Six months after the operation, the specimens of the MCA group were smoother than those in the handsewn group, and a slight amount of scar tissue was observed in the hand-sewn group. There are several reasons for this. Magnetic anastomosis technology applies the mutual attraction between magnetic rings to maintain a constant and balanced pressure on the tissues at the anastomosis, resulting in slow ischemic necrosis of the tissues between the magnetic rings and the growth and healing of the surrounding tissues. This is a slow process that allows time for esophageal compensation to grow.Hand-sewn sutures use Vicryl to quickly tighten the tissues at both ends of the esophagus. There is a certain tension at both ends of the esophagus, which may lead to shearing forces placed on the esophageal tissue from Vicryl. Second, Vicryl, as an absorbable thread, will exist in the tissue for a long time as a foreign body, which may cause infection and scar hyperplasia. The suture material could play an important role in the healing of esophageal anastomosis. Vicryl is an absorbable material, but the time of absorption is more than 1 mo. During this period, Vicryl may act as a foreign body, leading to foreign body granuloma or anastomosis edema. Braided sutures are more prone to infection than monofilament sutures. Vicryl is the braided suture and perhaps in this study Vicryl is not the best selection.
At six months postoperatively, the magnetic anastomosis group grew slightly better than the handsewn group. Before surgery, the weights of the dogs in both groups were the same. One month after surgery, the body weight of the hand-sewn group was significantly lower than that of the magnetic anastomosis group. Three months after surgery, the weights of the dogs were similar in both groups.This suggests that MCA may contribute to enhanced recovery after esophageal reconstruction. There are two reasons that may contribute to the enhanced recovery with MCA technology: (1) The magnetic device has a gap in the middle, through which the liquid can enter the stomach, while it will not contact the anastomotic tissue. It may relieve pain and reduce the incidence of infection; and (2) The shedding time of the magnetic device is shorter than the time of the suture being discharged or absorbed by the tissues. The absorbable time of Vicryl RapideR is approximately 40 d[24], while the magnetic device discharge time is approximately 8 d. We observed that the dogs in the MCA group could feed earlier than those in the hand-sewn group. The MCA group of dogs recovered faster and better than the dogs in the hand-sewn group.
During 6 mo of observation, there was 1 stenosis in the MCA group and 1 stenosis and 1 Leakage in the hand-sewn group. Because the sample size was small, there was no statistically significant difference between the two groups. The rate of stenosis and leakage of anastomosis using the traditional handsewn operation is high. This has seriously affected the postoperative growth of children. We hope that this novel MCA technology can improve EA. The complication rate needs to be verified by more animal experiments and clinical case reports.
One clinical report showed that anastomosis was achieved in an average of 6 d (range 3 to 7 d) in 5 patients (age 6 mo to 5.9 years) with severe recurrent postsurgical esophageal stenosis refractory to dilatation[25]. Another MCA was achieved on day 36[26]. Clinical reports have shown that the anastomosis time ranges from 3 d to 36 d[26-28]. It involves many factors, such as the age of the child,type of EA, size of the magnetic ring and field strength of the magnetic device. This will be our next experimental purpose. Based on a large amount of experimental and clinical data, a model was established to estimate various parameters of magnetic devices preoperatively.
There are also some limitations of the study. First, our surgery location was on the dog’s neck, not in the thoracic cavity. This is not consistent with the clinicopathology. The position of EA is generally flush with the bifurcation of the main bronchus and may have a tracheoesophageal fistula. Second, in this study, we did not consider the effect of different structural sutures on the anastomosis. Does monofilament have less effect on anastomotic healing than multifilament? Third, this is a model of esophageal anastomosis, and not of anastomosis in the setting of an atresia, there are several differences.
CONCLUSION
MCA is an effective and safe method for esophageal reconstruction in dogs. The anastomosis with MCA is faster than the hand-sewn anastomosis. Postoperatively, some aspects of the recovery of the MCA group were faster and better than those of the hand-sewn group. We provide some information useful for the future clinical application of the device in selected cases.
ARTICLE HIGHLIGHTS

ACKNOWLEDGEMENTS
The authors would like to acknowledge the Laboratory Animal Center of Xi’an Jiaotong University for skillful technical assistance.
FOOTNOTES
Author contributions:Xu XH, Liu SQ, Lv Y designed and coordinated the study; Xu XH, Liu SQ, Cui XH and Suo RY performed the experiments and acquired and analyzed the data; XH Xu and Lv Y wrote the manuscript; and all authors approved the final version of the article.
Supported bythe National Natural Science Foundation of China, No. 82170676; and Natural Science Foundation of Shaanxi Provincial Key Industries Innovation Chain (Cluster)-Social Development Project, No. 2020ZDLSF02-03.
Institutional animal care and use committee statement:All experimental protocols were approved by the Committee on the Ethics of Animal Experiments of Xi’an Jiaotong University (Permit Number: XJTULAC2020-1441).
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:No additional data are available.
ARRIVE guidelines statement:The authors read the ARRIVE guidelines, and the manuscript was prepared and revised according to the ARRIVE guidelines.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Xiang-Hua Xu 0000-0001-6144-3938; Yi Lv 0000-0003-3636-6664; Shi-Qi Liu 0000-0002-2274-7880; Xiao-Hai Cui 0000-0002-7856-7117; Rui-Yang Suo 0000-0003-3622-958X.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Wang JJ
 World Journal of Gastroenterology2022年36期
World Journal of Gastroenterology2022年36期
- World Journal of Gastroenterology的其它文章
- Nonalcoholic steatohepatitis and hepatocellular carcinoma: Beyond the boundaries of the liver
- Impact of sarcopenia on tumor response and survival outcomes in patients with hepatocellular carcinoma treated by trans-arterial (chemo)-embolization
- Early extrahepatic recurrence as a pivotal factor for survival after hepatocellular carcinoma resection: A 15-year observational study
- SARS-CoV-2 and the pancreas: What do we know about acute pancreatitis in COVID-19 positive patients?
- Liver-specific drug delivery platforms: Applications for the treatment of alcohol-associated liver disease
- P2X7 receptor as the regulator of T-cell function in intestinal barrier disruption
