Radiotherapy assisted with biomaterials to trigger antitumor immunity
Xiojun Yu, Hito M,∗, Guiying Xu, Zhung Liu
a Department of Thoracic Surgery, Dushu Lake Hospital Affiliated to Soochow University, Suzhou 215021, China
b Department of Cardiothoracic Surgery, Children,s Hospital of Soochow University, Suzhou 215021, China
c Institute of Functional Nano & Soft Materials (FUNSOM), Jiangsu Key Laboratory for Carbon-Based Functional Materials and Devices, Soochow University,Suzhou 215123, China
ABSTRACT As an extensively applied therapeutic approach to combat tumors, radiotherapy generates localized ionizing radiation to destruct tumor cells.Despite its importance in clinical oncology, radiotherapy would often cause significant organ toxicity, and its therapeutic effect is limited by tumor hypoxia.Moreover, although abscopal therapeutic effects have occasionally been observed, radiotherapy is still mostly employed as a local treatment method that could hardly control tumor metastases.In recent years, strategies involving biomaterials and nanomedicine have received increasingly high attention to enhance cancer radiotherapy.Beyond sensitizing tumors for radiotherapy via various mechanisms, many biomaterial systems with immune stimulating effects have also been introduced to boost the antitumor immunity post cancer radiotherapy.In this mini-review, we will summarize the progress of different biomaterials and nanomedicine systems in combination with radiotherapy to trigger antitumor immune responses and enhance the efficacy of immunotherapy, and discusses the perspectives and challenges of this research direction aimed at clinical translations.
Keywords:Biomaterials Radiotherapy Immunotherapy
1.Introduction
Depending on the source of radiation, radiotherapy is divided into internal radiation and external radiation, both of which could directly kill tumor cells locally by generating reactive oxygen species (ROS) [1–3].However, the therapeutic efficacy of radiotherapy is often limited by the lack of oxygen in the tumor microenvironment [4,5].Although radiotherapy in certain cases could induce systemic immunotherapeutic effects through immunogenic cell death (ICD) for treating tumors [6,7], such abscopal effects are usually insufficient and unpredictable.While local irradiation have been reported to eradicate treated tumor, the therapeutic efficacy for metastatic foci and untreated lesions is quite limited [8].Most importantly, the large area irradiation is usually avoided in clinic due to serious organ damages [2,9].Therefore, there is an urgent need to develop strategies to enhance the efficacies of radiotherapy, not only for local treatment, but also for abscopal therapeutic responses, while not causing additional side effects.
Cancer immunotherapy has achieved rapid development in recent years [10].Different from traditional treatment methods such as radiotherapy and chemotherapy to directly destruct tumor cells,immunotherapy tames and activates the host’s immune system to attack tumor cells.Immunotherapeutics inhibit tumor growthviavarious pathways, ranging from activating and augmenting effector mechanisms to blocking suppressive receptors.For instance, immune cell therapies such as chimeric antigen receptor(CAR) T cell therapy have demonstrated promising therapeutic outcome in treating certain types of leukemias and lymphomas.The immune checkpoint blockade (ICB) therapy based on antibodies against cytotoxic T lymphocyte associated protein 4 (CTLA-4), programmed death receptor 1 (PD-1) and its ligand (PD-L1) [11], has already been extensively used in the clinic for treatment for a wide range of tumors.Those breakthroughs represent a paradigm shift from conventional cancer treatments to novel therapeutic strategies.
Increased attention has been attracted on the combination of immunotherapy with radiotherapy.It has been reported that ionizing radiation may be able to induce ICD and lead to exposure of tumor antigens that may subsequently trigger immune responses against abscopal distant tumors.Recently, the combination of radiotherapy with ICB immunotherapy has been tested in clinical trials to treat head and neck cancer [12], lung cancer [13,14],etc.,presenting promising therapeutic outcomes such as prolonging the overall survival of patients.Nevertheless, the uncertainty of radiation induced antitumor immunity is a problem needs to be resolved.Based on that, researchers are focusing on strategies to further augment the radiation-induced immunity [15].
In recent years, various types of biomaterials and nanomedicine systems have been explored to enhance the efficacy of cancer radiotherapy [16,17].For instance, nanomaterials containing high-Z elements could be employed as radio-sensitizers by depositing more radiation energy within the tumor.Another strategy of enhancing local radiotherapy is to relieve tumor hypoxia using nanocatalysts to decompose tumor endogenous hydrogen peroxide, or introduce oxygen nano-shuttles to transport more oxygen into tumors [18].Beyond enhancing the performance of radiotherapy for local tumor treatment, another proposing approach is to boost the antitumor immunities utilizing nano-adjuvants or other immunestimulating agents [19], so as to achieve systemic antitumor immune responses post local radiotherapy.In this mini review, we will summarize recent advances in the design of radiotherapy combined with immunotherapy.
2.Immune responses post cancer radiotherapy
Clinically, radiotherapy is used for treatment of various cancer types [20].The immune system plays an important role in radiotherapy induced tumor inhibition [21,22].Studies have shown that to achieve the same therapeutic effect, more radiation doses are required in mouse tumor models with congenital immunodeficiency than mice with a sound immune system [23], which may be related to the release of tumor associated antigen and further activation of immune response after radiotherapy.On the other side, in some clinical reports, it was observed that after the elimination of residual tumors under direction exposure to irradiation, sometimes the tumors in the non-radiation areas would also shrink.This is considered to be the result of radiotherapy inducing systemic immune responses.
During radiation therapy, the radiation energy would destroy the structure of DNA [24,25], causing the apoptosis of tumor cells.The rupture of dead cells will release a large amount of tumorrelated antigento trigger immune responses against tumor cells[26,27], a process named as immunogenic death.This type of cell death is different from tumor necrosis, and can trigger antitumor immunity for a sustained period of time [28].In addition, there are other mechanisms related to radiation triggered ICD.For example,radiotherapy would damage mitochondria and endoplasmic reticulum [29], inducing the exposure of tumor DNA fragments, which could be recognized by an intracellular protein called cyclic GAMP synthetase (cGAS) to further activate the interferon gene stimulator (STING) pathway (Fig.1a).In the study of Denget al., ionizing radiation produced a type I interferon-dependent anti-tumor response through the STING pathway [30].DNA of dying irradiated cancer cells was found in the cytoplasm of dendritic cells, which is responsible for the activation of the cGAS-STING-type I-IFN pathway [31,32].Among the different innate sensory pathways that regulate tumor inflammation, studies have shown that STING-type I-IFN is necessary for radiation-induced inflammation and subsequent adaptive immune responses [32].In addition to the STING pathway, Apetohet al.proved that after radiotherapy, high mobility group box protein 1 (HMGB1) released by damaged cells serves as toll-like receptor 4 (TLR4) agonist to stimulate antigen presenting cells such as macrophages and dendritic cells [33].In addition,calreticulin, which serves as a phagocytic signal for macrophages[34–36], has also been found to be related to the immune effect induced by radiotherapy (Fig.1b).
Owing to the capability of radiotherapy to trigger ICD of tumor cells, the combination of radiotherapy with immunotherapy especially ICB therapies has been widely tested in the clinic [37–39].However, the overall efficacies of such combination therapy strategies remain to be further improved.One important limitation is the immunosuppressive tumor microenvironment that prevents the recognition of tumor antigens by antigen presenting cells within the tumor.Meanwhile, the hypoxic and acidic tumor microenvironment would also limit the infiltration of CD4+effective T cells and CD8+killer T cells into the tumor.Moreover, studies have also shown that radiotherapy could stimulate the differentiation of fibroblasts into cancer-related fibroblasts by increasing extracellular matrix deposition and collagen expression [40–42], which promotes tumor growth through releasing chemokines and/or direct cell-cell contact, thereby resulting in a more immunosuppressive tumor microenvironment (Fig.1c).
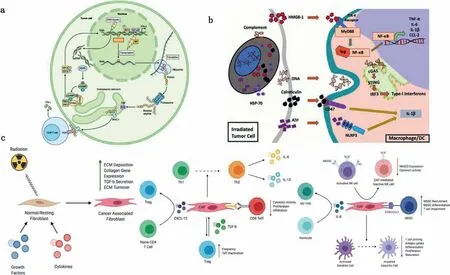
Fig.1.Immune responses induced by cancer radiotherapy.(a) Radiotherapy exposes immunogenic mutations for MHC-I presentation on the surface of cancer cells.Copied with permission [26].Copyright 2019, NRC Research Press.(b) Radiotherapy induces the release and activation of multiple different inflammatory mediators from injured cells including heat shock protein 70 (hsp70), HMGB1, cytosolic DNA, calreticulin, and adenosine triphosphate (ATP).Copied with permission [36].Copyright 2018, Frontiers Media S.A.(c) Mechanisms of radiation-induced transformation of resting fibroblasts to cancer-associated fibroblasts, resulting in immunosuppression.Reproduced with permission[40].Copyright 2021, John Wiley and Sons.
In summary, the immune responses induced by local irradiation alone have a relatively low positive rate for distant metastases, as evidenced by scarce reports of the spontaneous shrink of untreated tumor lesions [43–45].Even when radiotherapy is combined with ICB therapies, the immunosuppressive tumor microenvironment would still largely reduce the therapeutic responses of antitumor immunity [46].Therefore, there is an urgent need for a method that can enhance antitumor immune responses post radiotherapy treatment of local tumors, while limiting the unwanted side effects.
3.Biomaterials assisting external radiotherapy to trigger antitumor immunity
External radiotherapy used an exogenous machine to produce high-energy particle beams, including X-rays and gamma rays, to irradiate the tumor surface to achieve therapeutic effects.On one hand, direct irradiation of high-energy particle beam would destroy the DNA structure of tumor cells, leading to their abnormal functions and death.On the other hand, radiation could stimulate the generation of a large number of reactive oxygen species (ROS)inside cells to cause cell damages.External radiotherapy is short in duration and often requires multiple exposures.Although external beam radiotherapy could cause immunogenic death of tumor cells,the induced immunotherapy effect remains to be limited.To enhance the antitumor immune responses post external beam radiotherapy, Minet al.designed a variety of different antigen capture nanoparticles (AC-NPs) [47].In their study, polylactic acid-glycolic acid (PLGA) nanoparticles were used as the framework, and the nanoparticle surface properties were changed through different modification methods.Those AC-NPs are co-incubated with irradiated melanoma cells.Further comparison showed that maleimide-PEG (Mal AC-NP)-modified NPs had stronger antigen-binding ability, while PLGA NPs modified with methoxy-PEG (mPEG) showed the lowest antigen trapping ability.In mouse tumor models, after intravenous injection of those nanoparticles, the antitumor immunity post radiation of tumors was significantly improved with the presence of AC-NPs.When further combined with PD-1 blockade, the cure rate increased to 20%.Those mice rejected tumor rechallenge, demonstrating a durable antigen-specific immune memory.
It is known that oxygen molecules would be involved in the process of radiation-induced cell killing, by generating ROS under radiation or react with DNA radicals generated by radiation.The hypoxic tumor microenvironment is a potent barrier to the therapeutic responses of radiotherapy.Thus, many nanomedicine systems have been developed to enhance the efficacy of tumor radiotherapy by relieving tumor hypoxiaviadifferent strategies.In our previous work, we formulated a unique type of core-shell nanoparticles using PLGA core-shell nanoparticles to encapsulate catalase (Cat) inside the core.In the meanwhile, R837, a TLR7 receptor agonist, was loaded into the PGLA shell, forming PLGAR837@Cat nanoparticles [48].In this system, catalase could effectively alleviate the hypoxia of the tumor microenvironment and enhance the killing effect of radiotherapy.After the radiotherapy induced ICD of tumor cells, R837 acted as an immune adjuvant and triggered strong antitumor immune responses to inhibit tumor metastasis (Fig.2).Such therapeutic strategy could be further enhanced by combination with ICB therapy.Moreover, a potent immune memory to inhibit re-challenged tumors was also observed.
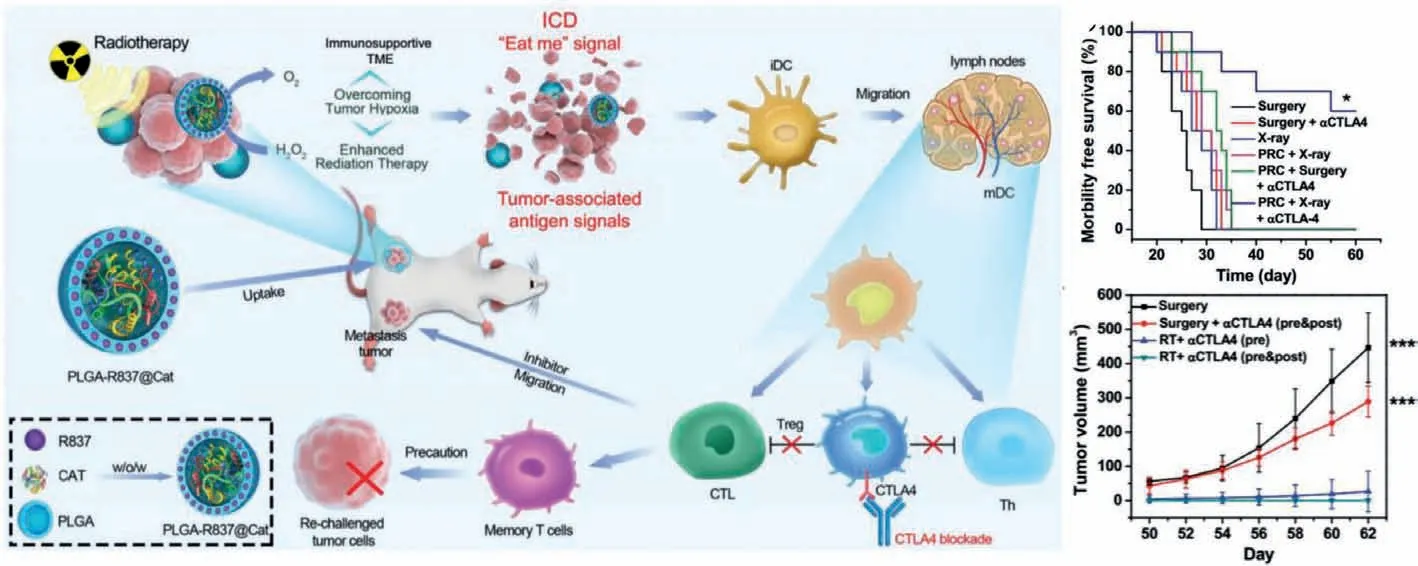
Fig.2.External beam irradiation induced immunotherapy assisted by PLGA-R837@Cat nanoparticles.PLGA-R837@Cat-based radiotherapy in combination with checkpointblockade could relieve tumor hypoxia and induce anticancer immune responses.Reproduced with permission [48].Copyright 2019, John Wiley and Sons.
The addition of metal elements to the multifunctional biomaterial structure can further sensitize radiotherapy.Huanget al.constructed nanoparticles using commonly used clinical elements gadolinium (Gd3+), 5′-guanosine monophosphate (5′-GMP)and hemin [49].In this system, Gd3+could increase the deposition of the radiation energy in the tumor site and produce more ROS, leading to tumor destruction under low doses of radiation.Meanwhile, Hemin was able to simulate the catalytic activity of peroxidase to further enhance the effect of radiotherapy.In addition to the oxidative damage of tumor cell membrane and structure caused by ROS, the destruction of lysosome would also release a variety of enzymes, resulting in cell autolysis.Moreover, the destruction of tumor cell organelles would release small fragments of tumor-associated antigens, which could activate the anti-tumor immune effect through a variety of pathways.In combination with PD-1 blockade, stronger anti-tumor immune responses were triggered to control tumor metastasis in a mouse tumor model (Fig.3).Nanoparticles with even more functions have also been designed to achieve combination therapy against tumors.Gaoet al.used selenium-containing multifunctional nanomaterials as a carrier to load chemotherapeutic drug doxorubicin.After systemic administration of those nanoparticles, external beam radiation therapy was further conducted on tumors of those mice [50].On one hand, radiotherapy would promote the release of doxorubicin and improve the effect of chemotherapy.On the other hand, radiation could also be used as an external switch to oxidize diselenide loaded in nanoparticles into selenic acid, which could enhance the function of NK cells.The combination of immunotherapy, chemotherapy and radiotherapy was realized using those multifunctional nanoparticles to achieve greatly improved antitumor therapeutic effect (Fig.4).
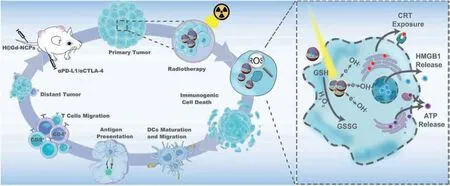
Fig.3.The mechanism of H@Gd-NCPs for radiosensitization via amplifying intracellular oxidative stress to potentiate checkpoint blockade immunotherapies.Copied with permission [49].Copyright 2020, John Wiley and Sons.
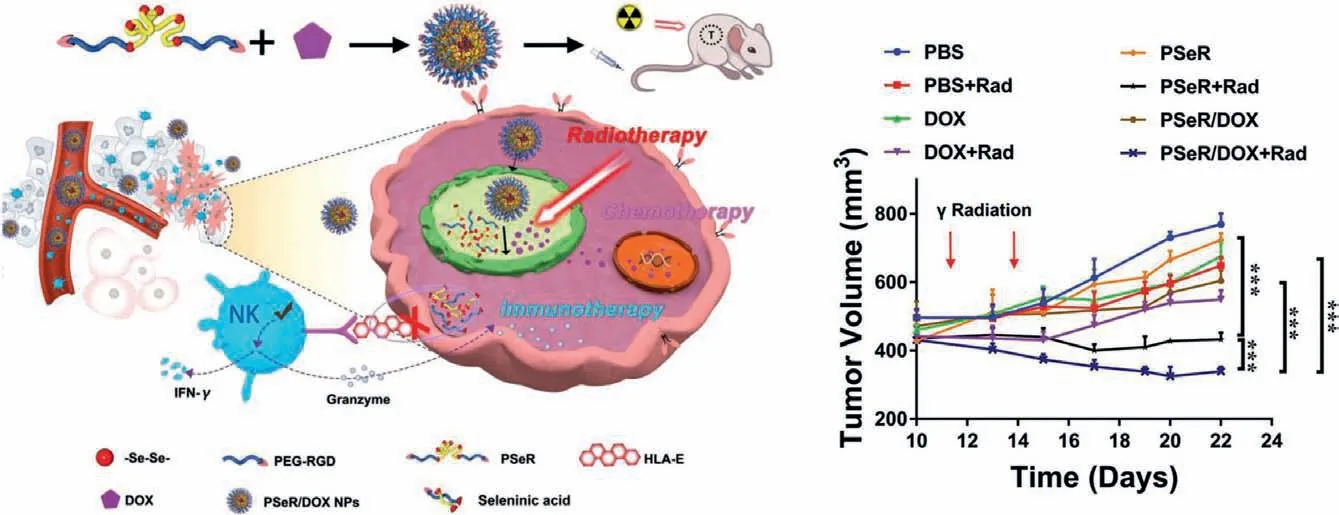
Fig.4.Radiotherapy induces the immune effect of selenium-containing nanomaterials to realize the combination of multiple therapeutics.Reproduced with permission [50].Copyright 2021, Nature Publishing Group.
4.Biomaterials assisting internal radioisotope therapy to trigger antitumor immunity
Internal radioisotope therapy refers to the placement of radioactive isotopes into the body to achieve local irradiation of tumors.Different from external irradiation, radioactive nuclide in the body can continuously emit high-energy particles to kill tumor cells.Idoine-125 beads and Yittrum-90 microspheres are two types of radioisotope devices widely used in clinic as brachytherapy strategies to treat different types of solid tumors such as liver cancer [51] and prostate cancer [52,53].Even so, the therapeutic effect of both internal and external radiotherapy will be weakened by the hypoxic tumor microenvironment.Moreover, the therapeutic efficacy of radioisotope-based brachytherapy to treat distant metastatic lesions is usually quite limited.
Tumor-homing biocompatible agents can be labeled with radionuclides to synergistically enhance the effect of radiotherapy while reducing peripheral damages [54,55].In a recent work, Peiet al.synthesized gold nanoclusters (Au NCs) with good biocompatibility by reducing HAuCl with glutathione [56].Through simple chelation,99mTc and177Lu can be labeled on the surface to obtain99mTc@Au NCs and177Lu@Au NCs.Interestingly, in their study, gold nanoparticles labelled with nontherapeutic99mTc showed a significant tumor suppressive effect because Au could act as an effective radiosensitizer.The therapeutic effect of177Lu@Au NCs would be even more powerful to kill tumors at low doses, further leading to the release of tumor-related antigens.When combined with PD-L1 blockade therapy, the combined treatment of177Lu@Au NCs plus anti-PD-L1 significantly prolonged the survival of mice (Fig.5a).
Hydrogels have been extensively used for local release of therapeutics.In a study from our group, Chaoet al.used a mixed solution composed of Idoine-131-labeld catalase (Cat), alginate (ALG)and F cytosine-phosphate-guanine motifs (CpG) to achieve the combined treatment of tumors [57].After intratumoral injection of the composite solution, ALG would interact with calcium ions to form a hydrogel, which would then fix the injected therapeutics(e.g., I131-labeld catalase) within the tumor.Catalase would then alleviate local hypoxia of the tumor to enhance the therapeutic effect of I131, leading to remarkably enhanced tumor inhibition effect.As a toll-like receptor 9 (TLR-9) agonist, CpG would induce powerful immunotherapeutic effects.As shown in different types of tumor models, local injection of131I-CAT/CpG/ALG plus systemic injection of anti-CLTA4 would result in powerful synergistic effect to eliminate both local tumors and distant metastatic tumors.Again,a long-term immune memory effect was observed for those mice with their tumor eliminated by injection of131I-CAT/CpG/ALG (Fig.5b).In fact, we are now working hard to push this technology into clinical use.
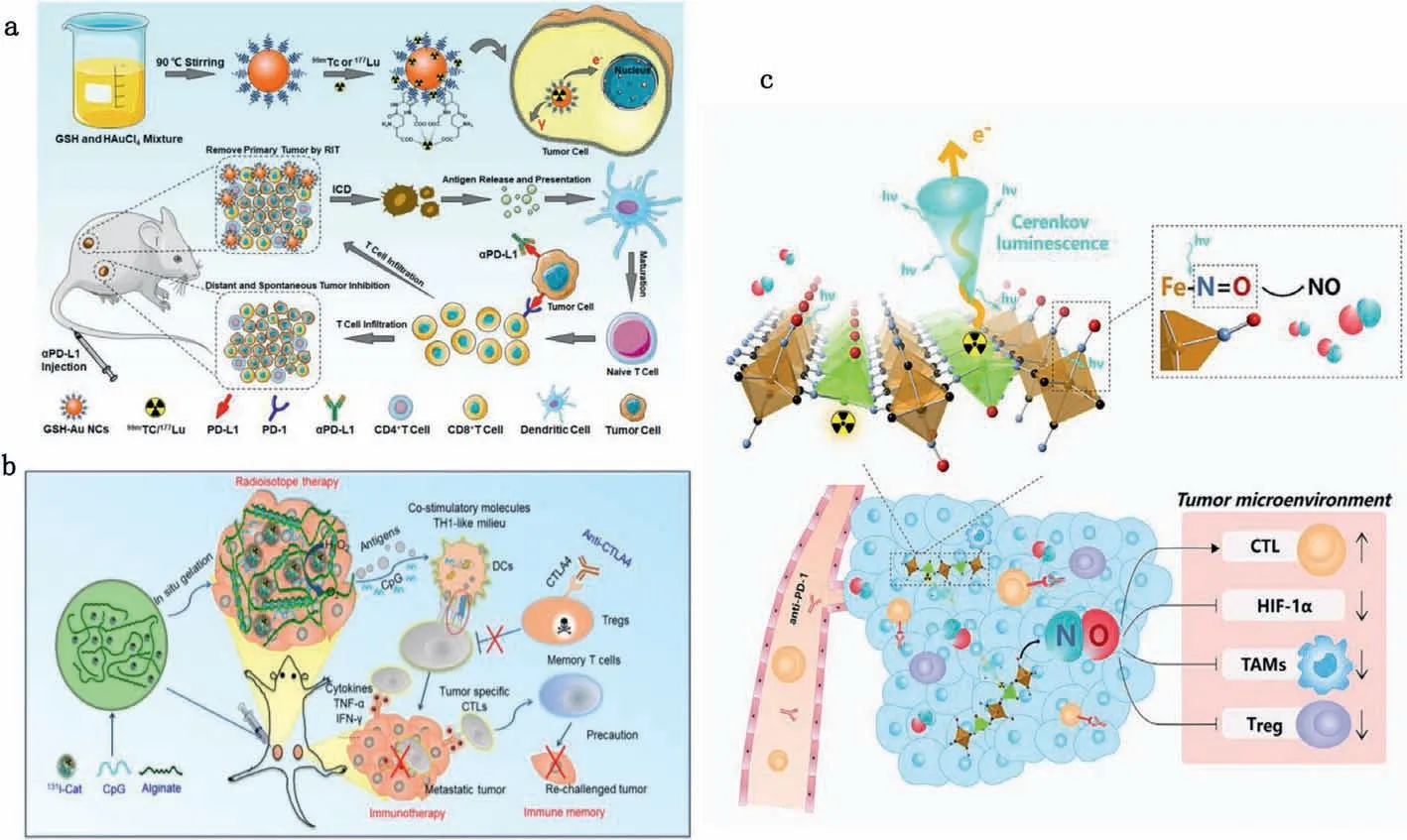
Fig.5.Internal irradiation-induced immunotherapy.(a) Synthetic procedure of radionuclide labelled Au NCs and the mechanism of antitumor immune responses induced by radionuclide labelled Au NCs in combination with checkpoint-blockade to inhibit distant and spontaneous tumors.Reproduced with permission [56].Copyright 2021,Elsevier BV.(b) Mechanism of anti-tumor immune responses induced by 131I-Cat/CpG/ALG-based RIT in combination with checkpoint blockade.Copied with permission[57].Copyright 2018, Nature Publishing Group.(c) The mechanism of antitumor immune responses induced by radionuclide labelled ZnFe(CN)5NO Nanosheets to enhance radioisotope-immunotherapy.Copied with permission [58].Copyright 2019, Cell Press.
In addition to playing a therapeutic role, radionuclides can also act as external switches to regulate the release of therapeutic molecules.In another work, we designed a multifunctional ZnFe(CN)5NO nanosheets labeled by phosphorus 32 (32P).The high-energy particle beam released by32P could directly kill tumor cells [58].Meanwhile, under the stimulation of32Ptriggered Cerenkov luminescence, continuously release nitric oxide(NO) from nanosheets was observed.Notably, NO could effectively modulate the immunosuppressive tumor microenvironment by inhibiting the tumor expression of hypoxia-inducing factorα(HIFα), increasing the cytotoxic T cell infiltration at the tumor site, and reducing the levels of immunosuppressive cell types such as regulatory T cells and tumor-associated macrophages within the tumor (Fig.5c) [59].Combined application of ZnFe(CN)5NO(P32) with PD-1 blockade induced strong antitumor immune responses and generated a long-term immune memory that could inhibit tumor metastasis.
5.Prospects and discussions
As a traditional tumor treatment method, radiotherapy has aroused extensive research interests due to its ability to trigger antitumor immune responses, making radiotherapy a great partner for cancer immunotherapy.This mini review summarizes various types of biomaterials and nanomedicine platforms rationally designed to boost the antitumor immunity post radiotherapy of tumors.Viamodulating the tumor microenvironment (e.g., relieving tumor hypoxia) with biomaterials, not only the efficacies of radiotherapies could be improved, the responses of tumors to immunotherapy would also be enhanced[60].In the presence of immune stimulating agents administrated into the tumor, the tumor antigens released after radiotherapy induced ICD would trigger tumor-specific immune responses,which would be particularly potent if in combination with ICB therapies.
How to translate those unique strategies into clinic use, would thus be the utmost important task in this reach direction.Generally speaking, the biomaterials and nanomedicine platforms would show prefect biocompatibility, and ideally, should be biodegradable[61,62].The formulations of those agents should be easily scaled upviaa controllable manner.Besides, the immunogenicity and potential side effects should be carefully evaluated prior to clinical trials.
Currently, most of those immune-stimulating biomaterials or nanomedicines are administrated directly into the tumor to enhance the antitumor immunity post radiotherapy.Although intratumoral injection may be less convenient for clinical practices compared with intravenous systemic administration, local injection may still be the most feasible way to realize this particular purpose, as systemic injection of immune stimulating agents may cause severe side effects such as cytokine storms.Triggering systemic antitumor immune responses after local injection of pharmaceutics and local radiotherapy may thus be a promising strategy to be explored in future clinic trials.The authors here believe that the combination of biomaterials-assisted radiotherapy with currently used immunotherapy (e.g., ICB therapies such as anti-PD1/PDL1) may indeed bring significant advantages to cancer patients in the years to come.
Declaration of competing interest
No conflict of interest exits in this manuscript.
Acknowledgments
This work was partially supported by the National Natural Science Foundation of China (Nos.21907073, 52032008, 51803146),the Jiangsu Social Development Project (No.BE2019658), and a Collaborative Innovation Center of Suzhou Nano Science and Technology.
 Chinese Chemical Letters2022年9期
Chinese Chemical Letters2022年9期
- Chinese Chemical Letters的其它文章
- A review on recent advances in hydrogen peroxide electrochemical sensors for applications in cell detection
- Rational design of nanocarriers for mitochondria-targeted drug delivery
- Emerging landscapes of nanosystems based on pre-metastatic microenvironment for cancer theranostics
- Development of environment-insensitive and highly emissive BODIPYs via installation of N,N’-dialkylsubstituted amide at meso position
- Programmed polymersomes with spatio-temporal delivery of antigen and dual-adjuvants for efficient dendritic cells-based cancer immunotherapy
- The effect of organic ligand modification on protein corona formation of nanoscale metal organic frameworks
