Early diagnosis of pancreatic cancer: What strategies to avoid a foretold catastrophe
Valeria Tonini,Manuel Zanni
Abstract While great strides in improving survival rates have been made for most cancers in recent years, pancreatic ductal adenocarcinoma (PDAC) remains one of the solid tumors with the worst prognosis. PDAC mortality often overlaps with incidence. Surgical resection is the only potentially curative treatment, but it can be performed in a very limited number of cases. In order to improve the prognosis of PDAC, there are ideally two possible ways: the discovery of new strategies or drugs that will make it possible to treat the tumor more successfully or an earlier diagnosis that will allow patients to be operated on at a less advanced stage. The aim of this review was to summarize all the possible strategies available today for the early diagnosis of PDAC and the paths that research needs to take to make this goal ever closer. All the most recent studies on risk factors and screening modalities, new laboratory tests including liquid biopsy, new imaging methods and possible applications of artificial intelligence and machine learning were reviewed and commented on. Unfortunately, in 2022 the results for this type of cancer still remain discouraging, while a catastrophic increase in cases is expected in the coming years. The article was also written with the aim of highlighting the urgency of devoting more attention and resources to this pathology in order to reach a solution that seems more and more unreachable every day.
Key Words: Pancreatic cancer; Pancreatic ductal adenocarcinoma; Early diagnosis; Liquid biopsy; Pancreatic cancer biomarkers; Artificial intelligence; Pancreatic cancer screening
lNTRODUCTlON
Pancreatic ductal adenocarcinoma (PDAC) is ranked as the seventh leading cause of cancer deaths worldwide, while it ranks fourth in the Western world, just behind lung, colorectal and breast cancers.Rahibet al[1] estimated that it will become the second leading cause of cancer death by 2030. The 2020 global cancer statistics reported a total of nearly 496000 new cases of PDAC and more than 466000 related deaths. PDAC mortality is almost overlapping with incidence[2].
The 5-year survival rate of PDAC is less than 10%[3]. A study that included 84275 patients showed that the 5-year survival rate increased from 0.9% in 1975 to 4.2% in 2011, considering all stages of PDAC.In patients undergoing surgical resection, it increased from 1.5% to 17.4%[4], while in unresected patients by 0.8% in 1975 and 0.9% in 2011. The high mortality and poor improvement in survival rates over the years are due to several factors. First, the retroperitoneal location of the pancreas results in the appearance of symptoms only when the neoplasm has reached considerable size, and diagnosis is often made at an advanced stage of the disease. Second, PDAC is inherently characterized by a fierce biology with early metastasis, and in fact about half of patients have metastatic disease at the time of presentation. Third, PDAC drastically weakens patients, limiting the possibility of aggressive treatments. Finally, through the desmoplastic reaction, it shows resistance to many antineoplastic therapies[5,6].
The 5-year survival rate for patients with stage 0 (in situ) according to the Union for International Cancer Control classification is 85.8%, while that of patients with stage IA is 68.7%. In the early stages of the disease, therefore, the prognosis is relatively good[7,8]. Early diagnosis of the disease is therefore essential.
Our efforts should focus on recognizing risk factors that contribute to the development of the disease in order to define the population at risk that could benefit from a screening protocol and on researching new techniques for early diagnosis[9-12].
RlSK FACTORS AND STRATlFlCATlON
Several non-modifiable and modifiable risk factors are correlated with PDAC. Non-modifiable risk factors include the patient’s age, ethnicity, gender, blood type, microbiota, diabetes mellitus, family history and genetic predisposition, while modifiable risk factors include tobacco use, alcohol consumption, diet, pancreatitis, obesity and socioeconomic status[12]. According to some studies, onethird of all cancers could be prevented through lifestyle improvement. The EPIC study, for example,evaluated the association between healthy lifestyle index score and pancreatic cancer[13,14]. A threepoint increase in this score, achieved through adherence to healthy behaviors, is associated with a 16%-23% lower risk[15]. No smoking, making your home/workplace smoke-free, maintaining a normal body weight, having a diet rich in grains, legumes, and vegetables and limiting alcohol intake are key factors in the prevention of PDAC.
According to several studies, the new onset of diabetes in an elderly patient should suggest PDAC,especially if such a finding is associated with unintentional weight loss[16-18]. A study by Pelaez-Lunaet al[19] evaluated the use of computed tomography (CT) scans in asymptomatic patients at the time of diabetes diagnosis and found a higher likelihood of detecting potentially resectable tumors compared with scans performed 6 mo later. However, CT-based screening of all elderly patients with new-onset diabetes (NOD) is not feasible[18]. Screening programs and guidelines will likely be updated when the features that differentiate pancreatic cancer-associated diabetes from other cases of NOD are identified.
The creation of a pancreatic cancer risk prediction model based on the integration of multiple risk factors could contribute to its early detection[20]. Sharmaet al[21] developed a model called Enriching New-Onset Diabetes for Pancreatic Cancer that weights the scores of three factors including weight change, blood glucose change and age at diabetes onset in patients with NOD. A score of at least three points in the Enriching New-Onset Diabetes for Pancreatic Cancer model was able to identify individuals who developed PDAC within 3 years of the onset of diabetes with good sensitivity and specificity[21].
In addition to the strictly environmental risk factors, familial pancreatic cancer and genetic syndromes (hereditary breast and ovarian cancer syndrome, Lynch syndrome, familial atypical multiple melanoma, Peutz-Jegher syndrome, Li-Fraumeni syndrome and hereditary pancreatitis) are added.Familial pancreatic cancer is defined by the occurrence of PDAC in at least two first-degree relatives and accounts for up to 10% of all cases of PDAC[22].
Patients at high risk for developing PDAC include those with inherited risk factors (both genetic syndromes and familial pancreatic cancer), those with NOD and those with cystic lesions of the pancreas.
Pancreatic cysts are found in approximately 8% of individuals over the age of 70 years[23] and include intraductal papillary mucinous neoplasms (IPMN) and mucinous cystic neoplasms, both of which are precursors to PDAC. IPMN and mucinous cystic neoplasms are collectively referred to as mucinous cystic lesions. In contrast to the third precursor lesion, pancreatic intraepithelial neoplasia,which can be identified only at surgical histopathology, mucinous cystic lesions are easy to detect and are found incidentally in 3% of CT subjects[23]. Therefore, their identification offers the potential for early diagnosis of PDAC. However, there are two problems. First, not all pancreatic cystic lesions are IPMN or mucinous cystic neoplasms. Many are cystic lesions without risk of malignant transformation,and therefore do not require surveillance. Second, most IPMN and mucinous cystic neoplasms do not progress to PDAC. Over the years, evidence has been found to predict the possibility of progression to PDAC[23].
In mucinous cystic neoplasms the presence of eggshell calcification, larger tumor size or a mural nodule on cross-sectional imaging is suggestive of malignancy[24]. Regarding IPMN, worrisome (main duct 5-9 mm, enhancing mural nodule < 5 mm, thickened, enhancing cyst wall, branch duct IPMN > 3 cm, abrupt caliber change in main duct with upstream atrophy, lymphadenopathy, pancreatitis,increased serum 19-9, cyst growth > 5 mm over 2 years) and high-risk features (main duct > 1 cm,enhancing, mural nodule > 5 mm, jaundice) have been defined[25].
However, these clinical features are still imperfect in differentiating between benign cysts and mucinous cystic lesions that harbor high-grade dysplasia or PDAC and require surgical resection and mucinous cystic lesions that have low-grade dysplasia and are safe to look at.
For the time being, a screening program is offered to individuals with a strong family history and/or genetic predisposition to develop pancreatic cancer and subjects with mucinous cystic lesions of the pancreas. The primary goals of screening are the detection of high-grade dysplastic precancerous lesions(IPMN and pancreatic intraepithelial neoplasia) and T1N0M0 pancreatic cancer that are more amenable to potentially curative resection[26].
The current recommendation is to perform endoscopic ultrasound (EUS) or magnetic resonance imaging (MRI)/magnetic resonance cholangiopancreatography. Screening is recommended at age 50 years or 10 years before the youngest relative with PDAC in familial pancreatic cancer cases. In other settings, screening is performed between the ages of 35 years and 45 years. In case the patient had a normal pancreas on imaging, it is recommended to repeat the procedure every year alternating EUS and magnetic resonance cholangiopancreatography. However, no consensus has been found on the preferred modality and optimal timing/frequency. This reflects the absence of robust data in the literature and underscores the lack of biological tools to detect precancerous lesions early.
lMAGlNG
There are several imaging methods that can identify pancreatic cancer at an early stage. Contrastenhanced CT and MRI according to Japanese guidelines[27] are the first methods to be performed in patients with suspected PDAC based on clinical symptoms, serum pancreatic enzymes, tumor markers and transabdominal US. They are supplemented by EUS and endoscopic retrograde cholangiopancreatography (ERCP).
A study evaluated the diagnostic accuracy of US, CT, MRI, and EUS in 200 cases of PDAC stage 0/1.Only 20% of patients were symptomatic[28]. The diagnostic accuracy was 67.5%, 98.0%, 86.5%, and 86.5%, respectively. According to some authors, CT and US are procedures with limitations in the early detection of pancreatic cancer because only indirect signs, such as pancreatic duct dilatation, localized pancreatic atrophy or local fat changes in the pancreatic parenchyma, can be detected with these methods[20].
Two systematic reviews[29,30] evaluated the performance of EUS in the diagnosis of pancreatic cancer. In the first review, EUS was shown to have higher sensitivity than CT (91%-100%vs53%-91%),while in the second review, Kitanoet al[30] reported that EUS was more sensitive than US and CT (94%vs67% and 98%vs74%, respectively).
However, conventional EUS does not distinguish carcinoma from other etiologies very well because most pancreatic tumors, including benign ones, have a hypoechogenic appearance. Contrast-enhanced EUS can improve imaging of parenchymal perfusion and microvessels in pancreatic pathology. This method has higher sensitivity (94.5%vs83.1%) and specificity (84.1%vs78.6%) than conventional EUS[31,32].
Endoscopic ultrasonography guided fine needle aspiration (EUS-FNA) represents the first-line method for pathological diagnosis. In relation to lesion size, the accuracy of EUS-FNA is 93.4% for lesions ≥ 20 mm, 83.5% for lesions of 10-20 mm and 82.5% for lesions of 10 mm or less[33]. Sometimes CT, MRI and EUS fail to detect early stage pancreatic tumors and it is difficult to collect specimens with EUS-FNA. In this situation, especially with regard to PDAC in situ, the only available imaging finding is localized stenosis of the main pancreatic duct. Detailed evaluation of the pancreatic duct by ERCP and subsequent cytology of pancreatic juice become extremely important for diagnosis. In this context, ERCP has a sensitivity and specificity of 57.9% and 90.6%[34]. The sensitivity of pancreatic juice cytology in the diagnosis of PDAC in situ is 72.2%-100%[28,35].
ERCP is particularly useful in distinguishing autoimmune pancreatitis from PDAC, especially in patients[36] with atypical pancreatic parenchymal findings, such as focal enlargement of the pancreas and mass formation.
Ikemotoet al[37] proposed a recent algorithm for early diagnosis of PDAC in stage 0 and IA, with a promising long-term prognosis. In addition to pancreatic laboratory tests, US should be performed earlier in patients with risk factors in order to identify asymptomatic patients. Patients with an obvious tumor are managed according to conventional algorithms. Patients who do not have an overt pancreatic tumor but have indirect findings, such as abnormalities of the main pancreatic duct, cystic lesions or pancreatic atrophy, should be evaluated by MRI with magnetic resonance cholangiopancreatography. If the MRI shows abnormalities suggestive for PDAC, EUS-FNA is performed[37].
ARTlFlClAL lNTELLlGENCE APPLlED TO lMAGlNG
Great hopes are now pinned on artificial intelligence (AI) for solving the most difficult problems in medicine, and these include the early diagnosis of PDAC. AI is the ability of a computer to perform functions and reasoning typical of the human mind completely autonomously. In the deepest sense, it is the ability of a machine to learn and improve automatically based on experience, provided directly through data. In this way, AI becomes a powerful tool for discovering signals that are difficult for humans to infer or describe and for expanding the frontiers of our scientific capabilities.
Muhammadet al[38] used AI to predict the risk of developing PDAC. By analyzing variables such as demographic data, comorbidities and family history, they built a model capable of predicting the development of PDAC with good accuracy [area under the curve (AUC) of 0.85][38,39].
The application of AI in the field of radiology is also very promising, as AI is capable of analyzing thousands of images on a pixel-by-pixel level, does not make human errors and achieves data processing in a short time[40]. Several studies have reported the application of AI in EUS image analysis of pancreatic diseases. Daset al[41] evaluated the performance of AI in differentiating PDAC from normal pancreas and chronic pancreatitis. The algorithm they used identified neoplasia with an AUC of 0.93. A recent study by Zhuet al[42] reported an overall accuracy of 94% by AI in distinguishing pancreatic cancer from chronic inflammation. CT is the most explored medical imaging modality with AI. Liuet al[43] reported an AUC of 0.963 for the diagnosis of PDAC using CT with the AI platform. In addition, the time to diagnosis was 20 s/case, certainly less than the time needed by radiologists. The same authors, in more recent work, found 99% accuracy for analysis based on the use of AI. In this study, AI provided higher sensitivity than radiologists (0.983vs0.929, respectively)[44]. AI missed 3(1.7%) of 176 PDACs (1.1-1.2 cm), while radiologists missed 12 (7%) of 168 PDACs (1.0-3.3 cm), of which 11 (92%) were correctly detected by AI.
Two important ongoing projects should be noted. Project Felix is a multidisciplinary study led by Johns Hopkins University, which compared 156 PDAC cases and 300 healthy controls using deep learning computer models with manually segmented images. In an initial report, they reported a sensitivity and specificity of 94% and 99%, respectively[45]. The analysis was subsequently expanded to 575 normal patients and 750 patients with PDAC. The second ongoing project is being conducted by the Alliance of Pancreatic Cancer Consortium Imaging Working Group[46]. The goal of the project is to create a shared repository by collecting pre- and post-diagnosis CT, MRI and US images of patients with PDAC to develop AI that can predict the onset of pancreatic cancer and/or diagnose it at an early stage[47].
LlQUlD BlOPSY
Serum biomarkers
Carbohydrate antigens:The most validated serum tumor marker in terms of diagnostic, prognostic and surveillance capacity for pancreatic cancer is CA19-9. The sensitivity and specificity of elevated CA19-9 to detect PDAC are 79% and 82%, respectively[48,49].
However, the use of CA19-9 has several limitations. Approximately 10% of the Caucasian population has reduced CA19-9 production due to Lewis antigen dependence. In addition, there are several conditions that result in the increase of the biomarker, such as obstructive jaundice, liver cirrhosis,chronic pancreatitis and cholangitis. The low positive predictive value of CA19-9 limits its application as a screening tool for larger populations[48,50-52]. Other carbohydrate antigens have been evaluated for early diagnosis of pancreatic cancer, such as CA125, CA72-4[53], CA50, CA199 and CA242[48,54]. The solitary diagnostic potential of these biomarkers could not be verified; however, they could help in discriminating between benign and malignant pancreatic lesions in combination with CA19-9[48].
Circulating tumor DNA and circulating tumor cells:New and interesting diagnostic tools in the field of pancreatic cancer are circulating tumor DNA (ctDNA) and circulating tumor cells (CTCs). In patients with malignancies, cell-free circulating DNA (cfDNA) molecules are released from tumor cells by apoptosis, necrosis or active release and are called ctDNA. The ctDNA contains mutations specific to the cancer cells from which they are released[55,56]. Thanks to these DNA molecules, it is therefore possible to trace the presence or absence of cancer.
However, a recent meta-analysis evaluated the role of ctDNA in the diagnosis of PDAC and found a rather low sensitivity[57]. This happens because in the early stages the rate of necrosis and apoptosis is lower and not enough ctDNA is released into the circulation (in the early stages of PDAC, only one molecule of circulating tumor DNA can be detected for every 5 mL of plasma)[57]. This challenge could be solved with technological advances, and ctDNA could become an important tool for early diagnosis.
CtDNA has been studied together with other biomarkers to improve its sensitivity and specificity.The combination of KRAS mutations in ctDNA and CA19-9 proved to be particularly interesting.Indeed, it showed a sensitivity and specificity of 0.98 and 0.77, respectively, to differentiate PDAC from chronic pancreatitis and sensitivity and specificity of 0.82 and 0.81 to differentiate PDAC from benign pancreatic tumors[56,58]. Combining the KRAS mutation in ctDNA with four protein biomarkers (CEA,CA19-9, hepatocyte growth factor and osteopontin) identified 64% of patients with pancreatic cancer with a specificity of 0.99[59]. This strategy seems to be very promising; however, it needs validation through studies on large populations.
Analysis of epigenetic alterations in cfDNA also seems to play an important role. By assessing the methylation status of two genes (ADAMTS1andBNC1) in cfDNA, it seems possible to identify pancreatic cancer early with a sensitivity of 0.95 and specificity of 0.92[60]. In a pilot study, it was reported that a model combining changes in 5-methylcytosine and 5-hydroxymethylcytosine in cfDNA achieved a sensitivity of 0.94 and specificity of 0.95, with an AUC of 0.99 for the diagnosis of PDAC[61].
The ability of targeted cfDNA methylation analysis to detect and localize multiple cancer types at all stages was evaluated. Among patients included with PDAC at different stages, a sensitivity of 0.63 in stage I, 0.83 in stage II, 0.75 in stage III and 1.0 in stage IV was found[62]. These changes in cfDNA methylation could be very useful for monitoring risk groups[63].
CTCs can be isolated tumor cells or cells organized in a group to form a tumor microthrombus[64]and are detected in 21%-100% of patients with PDAC[65]. According to some studies, they can be detected in 75%-80% of patients with early-stage tumors[66] and up to 88% of patients with precursor lesions, predominantly IPMNs[67-69]. Notably, CTCs identify patients with high-grade dysplasia,indicating its potential to stratify high-grade IPMNs against low-grade IPMNs and other benign cysts[67]. In a meta-analysis, the sensitivity, specificity and AUC for PDAC diagnosis of ctDNA, exosomes and CTCs were evaluated. They were 0.64, 0.92 and 0.94 for ctDNA, 0.93, 0.92 and 0.98 for exosomes and 0.74, 0.83 and 0.81 for CTCs, respectively[57]. This lower AUC of CTCs is due to the possibility that CTCs become trapped in the liver when traveling through the portal vein[57]. The ability to detect CTCs by analyzing portal vein blood is greatly increased. They can be found in 100% of patients with metastatic PDAC[70] and in 58% of resectable patients[71]. As with ctDNA, the low amount of CTCs in the early stages is the main factor hindering their use as biomarkers[57].
RNA, metabolites and exosomes:The most significant microRNAs aremiR-21,miR-25andmiR-233.miR-21has a sensitivity for early diagnosis of 0.90 and a specificity of 0.72, whilemiR-25has a sensitivity of 0.75 and 0.93, respectively[72,73]. In contrast,miR-233has proven useful in the differential diagnosis between benign and malignant IPMNs[74]. The microRNAs offer a cumulative sensitivity for earlystage pancreatic cancer of 0.79 and a specificity of 0.74[75]. The combined use of CA19-9 and microRNAs can improve diagnostic accuracy, especiallymiR-216[76-77].
Potentially useful biomarkers also include long non-coding (lnc)RNAs.SNHG15lncRNA expression is found to be increased in patients with pancreatic cancer compared to healthy controls[78]. Permuthet al[79] demonstrated that the differential diagnosis between malignant and nonmalignant IPMNs can be made through the combination of eight lncRNAs. In addition, some lncRNAs (HAND2-AS1,CTD-2033D15.2andlncRNA-TGF) are early markers of IPMNs[80]. Other lncRNAs that might be useful in the early detection of pancreatic cancer and IPMN areHOTAIR,MALAT1,MEG3,H19,PVT1,HOTTIP[81],
HAND2-AS1,CTD-2033D15.2andlncRNA-TGF[82].The role of serum metabolites in pancreatic cancer has become of interest with the advent of metabolomic technologies involving nuclear magnetic resonance and mass spectrometry[83]. An important study was performed by Michálkováet al[84], who developed a nuclear magnetic resonancebased model that included 12 metabolites (3-hydroxybutyrate, lactate, glutamine, alanine, valine, lysine,citrate, histidine, isoleucine, glutamate, acetone and dimethylamine). The model has 94% accuracy,100% sensitivity and 90% specificity in distinguishing patients with PDAC from healthy individuals[84].
Another study compared the metabolomic profiles of serum samples from patients with NOD and those with PDAC and NOD[85]. This identified 62 different metabolites and found that a panel including N-succinyl-L-diaminopimelic and PE (18:2) had high sensitivity (93.3%) and specificity(93.1%). Currently, studies focusing on metabolomics are expensive and consequently rare; however, it is offering great results on the early diagnosis of PDAC. Further studies are desperately needed.
Recent studies are focusing on multimarker panels in combination with CA19-9. The combined use of eight proteins (S100A11, ITGB5, PPY, ERBB3, SCAMP3, RET, 5-NT, CEACAM1) discriminated with fair accuracy between patients with early stage I/II PDAC and healthy individuals[48,86].
A new and still much to be studied chapter in PDAC concerns the study of exosomes. Kitagawaet al[87] studied molecules of exosomal mRNA (CCDC88A,ARF6,Vav3andWASF2) and nucleolar RNA (SNORA14B,SNORA18,SNORA25,SNORA74AandSNORD22) and obtained excellent results for earlystage neoplasia. Tumor-specific expression of exosome surface proteins, the so-called tumor-specific surfaceome, can also be analyzed. Castilloet al[88] characterized six PDAC-specific surfaceome proteins,such as CLDN4, EPCAM, CD151, LGALS3BP, HIST2H2BE and HIST2H2BF. These proteins were suggested as promising biomarkers for PDAC diagnosis by the authors. Yuet al[89] developed a signature with long RNAs from plasma extracellular vesicles. This signature identified stage I/II pancreatic cancer with very high accuracy and performed better than CA19-9 in distinguishing PDAC from chronic pancreatitis (AUC 0.931vs0.873)[89]. Serum biomarkers are summarized in Table 1.
Pancreatic juice and pancreatic cyst fluid
In addition to blood, other body materials can be exploited to diagnose PDAC. For example, pancreatic juice collected during ERCP and cyst fluid obtained by EUS-FNA can be analyzed for specific markers.They include KRAS and GNAS mutants (the latter specific for IPMNs) as well as TP53, SMAD4,PIK3CA, PTEN and AKT1, which are generally related to IPMN-associated tumors[90-92].
Biomarkers still under study include mucins (MUCs). Normal pancreatic tissue expresses low levels of MUCs, whereas in branch duct IPMNs there is upregulation of the mucin gene and even more pronounced changes in PDAC[93-95]. MUC4 and MUC16 are 100% specific for pancreatic cancer but have sensitivities of 63% and 67%, respectively[95]. The combined biomarker panel consisting of MUC5AC and CA19-9 also showed excellent performance in distinguishing pancreatic cancer subjects from healthy controls[96].
It also seems possible to distinguish pancreatic cystic lesions with high-grade dysplasia or malignancy by assessing interleukins (IL-1b, IL-5 and IL-8) present in pancreatic juice or by using the monoclonal antibody Das-1. Das-1 can detect pancreatic cysts at risk of malignancy with a sensitivity of 88% and specificity of 98%[97-99].
In recent work by Majumderet al[100], a panel of three methylated DNA markers (C13orf18, FER1L4 and BMP3) in pancreatic juice discriminated cases from controls with good accuracy. Using a specificity cutoff value of 86%, the panel distinguished patients with any stage of pancreatic cancer from controls with a sensitivity of 83% and identified patients with stage I or II PDAC or IPMN with high-grade dysplasia with a sensitivity of 80%[100].
Saliva
Progress has also been made in saliva evaluation. A recent study[101] identified seven upregulated genes (MBD3L2,KRAS,STIM2,DMXL2,ACRV1,DMDandCABLES1) and five downregulated genes (TK2,GLTSCR2,CDKL3,TPT1andDPM1) in subjects with PDAC compared with healthy controls or those with chronic pancreatitis. It was possible to discriminate patients with pancreatic cancer with sensitivity and specificity greater than 90% by combining the mRNAs ofMBD3L2,KRAS,ACRV1andDPM1[101]. Xieet al[102] evaluated the expression of lncRNAs and found an upregulation ofHOTAIRandPV1Tin the PDAC group compared with controls and benign pancreatic cancers. The combination of salivaryHOTAIRandPVT1differentiated PDAC from healthy controls with a sensitivity of 78.2%and specificity of 90.9% and PDAC from benign tumors with a sensitivity of 81.8% and specificity of 95%[103].
Urine
Radonet al[104] used three protein biomarkers (REG1A, TFF1 and LYVE1) to form a powerful urinary panel that could detect patients with stage I-II PDAC with an accuracy of more than 90%. Brezgyteet al[105] found increased levels ofmiR-143,miR-204andmiR-223and reduced levels ofmiR-30ein the urineof patients with stage I PDAC compared with the healthy population. However, further studies are needed to validate their clinical utility.

Table 1 Serum biomarkers
A case-control study that included 914 PDAC patients found the superiority of a panel of metabolites(proline, sphingomyelin, phosphatidylcholine, isocitrate, sphinganine-1-phosphate, histidine, pyruvate,ceramide, sphingomyelin) over CA19-9 in discriminating early-stage PDAC from chronic pancreatitis[106]. According to the authors, the metabolic panel could result in changes in the diagnostic pathway and treatment stratification for one-third of the included patients[106]. Biomarkers of pancreatic juice and cystic fluid, saliva and urine are listed in Table 2.
ARTlFlClAL lNTELLlGENCE AND BlOMARKERS
AI can be applied to the identification of biomarkers. Zhanget al[107] identified a nine gene pair signature that can distinguish PDAC patients from non-PDAC patients. Alizadeh Savarehet al[108]evaluated the best miRNAs using a machine learning method to aid in the early detection of PDAC. The final model includedmiR-92a-2-5p,miR-125b-3p,miR-532e5p,miR-663a and miR-1469with a high performance in differentiating PDAC from controls (accuracy, 0.93; sensitivity, 0.93 and specificity,0.92).
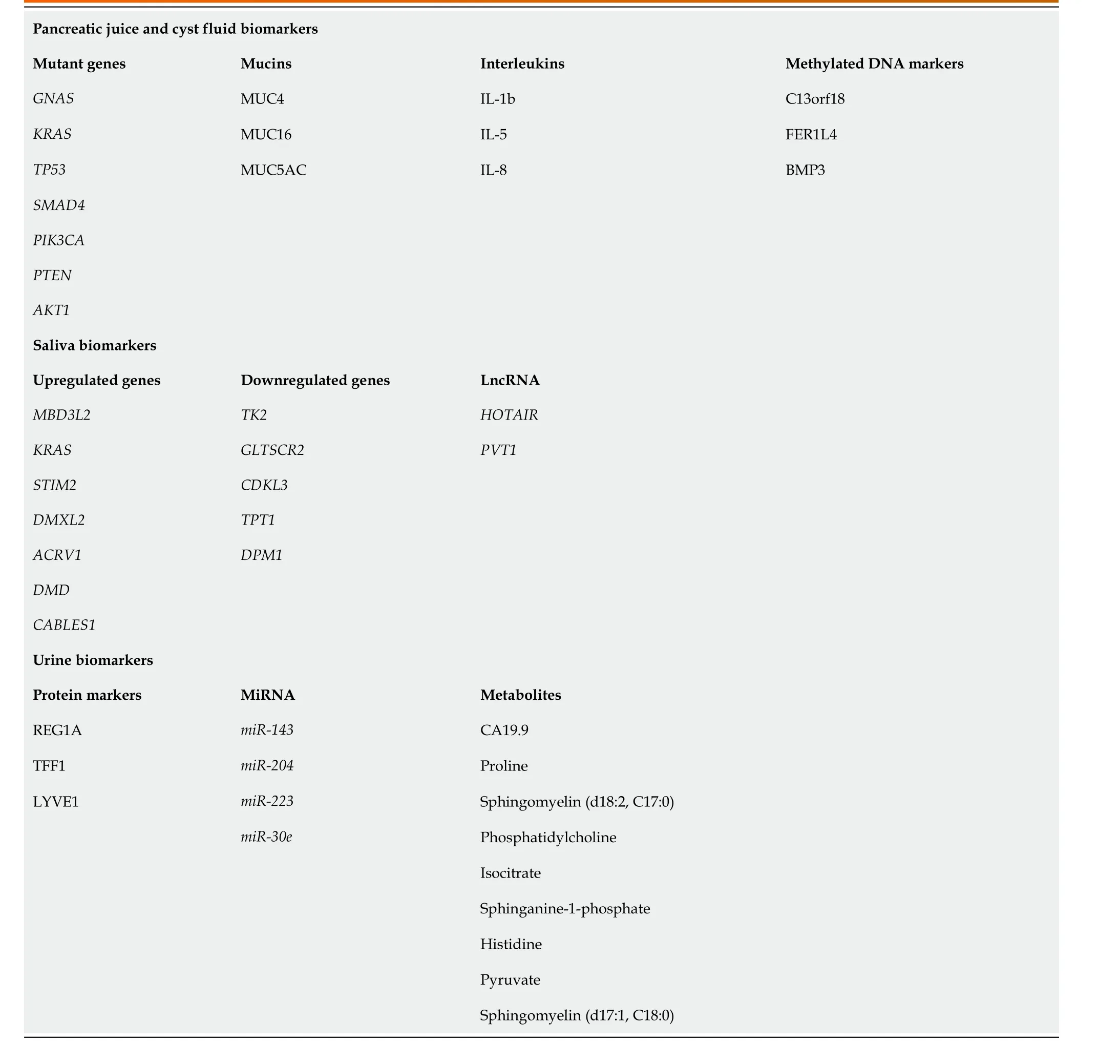
Table 2 Pancreatic juice and cyst fluid biomarkers, saliva biomarkers, urine biomarkers
WHAT STRATEGlES TO AVOlD A FORETOLD CATASTROPHE
As we have already mentioned in the introduction, the current predictions for PDAC give us a glimpse of a catastrophe on the horizon. If the increase in annual PDAC cases continues at the current rate, we will soon have a staggering number of cases without the weapons to stem this foretold catastrophe. The only option is to arm ourselves and not arrive unprepared for this hard battle. What strategies should we adopt to prepare for this ordeal? Undoubtedly first, we need to make academia, industry and the politics/economic world understand the urgency of finding solutions quickly, trying to interact with each other according to specific competencies. On the one hand, academia and industry will have to move forward together, as quickly as possible, in those research paths that we have broadly summarized in this article. On the other hand, the political/economic world, made aware of the emergency to be faced, will have to commit itself both to allocating more funding for research in this field and to lavishing more funding on public health. If public health had sufficient funds to subject all patients of a certain age to a simple screening ultrasound of the abdomen, perhaps many patients could be saved. But at present, with current resources, this scenario remains a pipe dream.
CONCLUSlON
In this article, we have summarized all the possible strategies we have available today for the early detection of PDAC and the paths that research must pursue to make this goal ever closer. Unfortunately, in 2022 the results for this type of cancer still remain discouraging, while a catastrophic increase in cases is expected in the coming years. The article has been written with the aim of highlighting the urgency of devoting more attention and resources to this pathology in order to reach a solution that seems more and more unreachable every day.
FOOTNOTES
Author contributions:Tonini V and Zanni M contributed equally to this work; Both authors designed the research study, wrote the manuscript and read and approved the final manuscript.
Conflict-of-interest statement:All authors report no relevant conflicts of interest for this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Italy
ORClD number:Valeria Tonini 0000-0003-3130-2928; Manuel Zanni 0000-0001-7732-7739.
S-Editor:Ma YJ
L-Editor:Filipodia
P-Editor:Ma YJ
 World Journal of Gastroenterology2022年31期
World Journal of Gastroenterology2022年31期
- World Journal of Gastroenterology的其它文章
- Duodenal-jejunal bypass reduces serum ceramides via inhibiting intestinal bile acid-farnesoid X receptor pathway
- Preoperative contrast-enhanced computed tomography-based radiomics model for overall survival prediction in hepatocellular carcinoma
- Prevalence and clinical characteristics of autoimmune liver disease in hospitalized patients with cirrhosis and acute decompensation in China
- Application of computed tomography-based radiomics in differential diagnosis of adenocarcinoma and squamous cell carcinoma at the esophagogastric junction
- Radiomics and nomogram of magnetic resonance imaging for preoperative prediction of microvascular invasion in small hepatocellular carcinoma
- Insights into induction of the immune response by the hepatitis B vaccine
