Radiomics and nomogram of magnetic resonance imaging for preoperative prediction of microvascular invasion in small hepatocellular carcinoma
Yi-Di Chen, Ling zhang, Zhi-Peng Zhou, Bin Lin, Zi-Jian Jiang, Cheng Tang, Yi-Wu Dang, Yu-Wei Xia, BinSong,Li-Ling Long
Abstract
Key Words: Magnetic resonance imaging; Hepatocellular carcinoma; Radiomics; Nomogram
lNTRODUCTlON
Hepatocellular carcinoma (HCC) is the fourth most common cause of cancer-related death and ranks sixth in terms of incident cases worldwide[1]. HCC is an important public health problem worldwide,and the death rate has increased over the past few years[2,3]. The cut-off size to define small HCC(sHCC) has been adopted as 3.0 cm[4]. Although the prognosis of sHCC is better than other types of HCC, the higher postoperative recurrence rate results in poor long-term outcomes after resection of sHCC[5]. Previous studies have confirmed that tumor size, higher tumor stage, worse histological differentiation, and the presence of microvascular invasion (MVI) are significant risk factors for shortterm recurrence of HCC[6-8]. In particular, the incidence of MVI, which is an independent poor prognostic factor for progression-free survival and overall survival of patients with sHCC, is generally about 20% in sHCC[9]. The presence or absence of MVI also suggests the need for different therapeutic options for HCC. Research has indicated that transcatheter arterial chemoembolization combined with intensity-modulated radiotherapy and sorafenib showed obvious clinical benefits in HCC patients with MVI[10]. Enlarged hepatectomy may be necessary for patients with sHCC and MVI.
Pathological examination of postoperative specimens is the gold standard for the diagnosis of MVI[11]. However, postoperative specimens exhibit hysteresis, which is not ideal for guiding treatment. In addition to being an invasive method, biopsy carries some risks of bleeding or tumor seeding[12].Gadolinium ethoxybenzyl-diethylenetriamine pentaacetic acid (Gd-EOB-DTPA) contrast-enhanced liver magnetic resonance imaging (MRI) is a noninvasive examination used to diagnose a variety of liver diseases[13] and can be used to assess liver function in patients with various stages of liver disease[14].Gd-EOB-DTPA MRI has been used to predict MVI based on tumor size, non-smooth tumor margin,incomplete capsule, and peritumoral hypointensity in the hepatobiliary phase[15-18]. However, sHCC has a small size, regular margin, complete capsule (or no capsule), and is usually free of peritumoral hypointensity. Therefore, it is difficult to predict the MVI of sHCC using traditional GD-EOB-DTPA MRI features.
Radiomics is an emerging field that attempts to quantify tumor heterogeneity related to the tumor parenchyma and microenvironment, including cellularity, extracellular matrix deposition, angiogenesis,necrosis, and fibrosis[19,20]. Machine learning is a scientific method of algorithms and statistical models that uses computers to interpret or predict patterns and inferences[21]. In many medical situations,medical imaging can be analyzed by machine learning through a series of processes, such as image registration, image segmentation, object detection, classification, and outcome prediction[22,23].Automated computer algorithms can be used for quantitative image analysis, which can objectively quantify the heterogeneity of an image by measuring the spatial variation in the pixel intensity[24].Radiomics with quantitative analysis provides a potential method for the diagnosis and prognosis of cancers[25,26]. Although a few studies have explored the feasibility of using radiomics based on computed tomography (CT) or MRI features to predict MVI in HCC[27-29], to our knowledge, previous studies have not investigated the prediction of MVI in sHCC. Therefore, this study aimed to explore the diagnostic value of liver Gd-EOB-DTPA MRI features in MVI of sHCC and to construct and validate the predictive efficacy of radiomics signatures and a nomogram for MVI in sHCC. This study also aimed to confirm the best modeling sequences, including images of T1 weighted imaging (T1WI), T2 weighted imaging (T2WI), diffusion-weighted imaging (DWI), and post-Gd-EOB-DTPA enhancement images of the arterial phase (AP), portal vein phase (PVP), and hepatobiliary phase (HBP), for extracting radiomics signatures by machine learning.
MATERlALS AND METHODS
Study cohort
The ethical review board of our institution approved this multi-center and external validation study(No. 2019 KY-E-134). This study adhered to the principles of the Declaration of Helsinki and the requirement for informed consent was waived. First, we retrospectively searched our institution’s(Guangxi Medical University First Affiliated Hospital, Hospital A) departmental electronic database for patients with consecutive hospital visits who had undergone upper-abdomen MRI between January 2016 and June 2020. A total of 221 patients were enrolled who met the following inclusion criteria: (1)Patients received Gd-EOB-DTPA enhanced upper-abdomen MRI and small HCC (tumor size ≤ 3.0 cm)were diagnosed; (2) no macrovascular tumor invasion on MRI(i.e., no tumor thrombus in the hepatic or portal veins); (3) primary HCC were diagnosed by histopathologic examination within two weeks after the MRI examination; and (4) MR images were of sufficient image quality. The exclusion criteria of this study were: (1) Patients who had undergone previous hepatobiliary surgery or liver-directed therapy (i.e., transarterial chemoembolization or ablation); and (2) the lesions were diagnosed other than primary HCC. Second, we continuously recruited 94 and 100 participants as independent external validation sets from two other hospitals (Affiliated Hospital of Guilin Medical University and West China Hospital,Hospital B and C) between July 2020 and August 2021 using the same inclusion and exclusion criteria.All patients underwent hepatectomy and pathologic assessment within two weeks of the MRI examination. The alpha fetal protein (AFP), Child-Pugh grades (grade A to C), and model for end-stage liver disease (MELD) scores were also analyzed and calculated for all patients (Figure 1).
Histopathologic analysis
Two experienced pathologists performed all the histological analyses in our central pathology laboratory. The Edmondson-Steiner classification was used to identify the major histological grades of HCC. When a tumor within a vascular space was lined by the endothelium, MVI was confirmed to be visible only microscopically, and the sites of positive MVI were documented. All disagreements were resolved by consensus.
MRI examination
All patients underwent 3.0 T MRI with six sequences of Gd-EOB-DTPA enhancement and DWI(Discovery MR750, GE Healthcare, Waukesha, WI, United States; Prisma and MAGNETOM Verio,Siemens Healthcare, Erlangen, Germany), including T1WI, T2WI, DWI, and post-injection phases of EOB as AP, PVP, and HBP. Detailed descriptions of the imaging acquisition protocols are summarized in Supplementary Table 1. For advanced DWI image quality, respiratory triggering, propeller, and resolve technical proposals were adopted.
Conventional radiological features analysis
Conventional radiological features were carefully evaluated based on the Liver Imaging Reporting and Data System (LI-RADS v2018), which included the tumor size, AP hyperenhancement, blood products in mass, capsule, corona enhancement, delayed central enhancement, diffusion restriction, fat or iron in mass more than the adjacent liver, fat or iron sparing in a solid mass, mosaic appearance, hepatobiliary phase hypointensity, hepatobiliary phase isointensity, and nodule-in-nodule appearance. The following MRI features were selected in this study: (1) Tumor size; the maximum diameter was measured on HBP axial images; (2) non-smooth tumor margin, which was defined as nodular with extranodular growth or multinodular confluence; (3) incomplete capsule, the region where the tumor border with liver tissue has no or incomplete capsule on portal venous phase or delayed phase; and (4) peritumoral hypointensity on HBP, wedge-shaped hypointense located outside of the tumor margin on HBP. After independent evaluation by three senior radiologists, discussions were conducted to reach a consensus wherever discrepancies occurred.
RADlOMlCS SlGNATURES AND REPRODUClBlLlTY ANALYSlS
Segmentation of the volume of interests
The Digital Imaging and Communications in Medicine images were transferred to the Big Data Intelligent Analysis Cloud Platform (Huiying Medical Technology Co., Ltd., Beijing, China). Two experts in liver MRI (senior radiologists with 15 and 25 years of experience) reviewed all images, and a radiologist manually segmented all target lesions who were blinded to the clinical information, creating a segmented volume of interest (VOI). After completion of the VOIs by a junior radiologist, the VOIs were reviewed by a senior radiologist for validation. To minimize the intensity variations caused by different scanning equipment and scanning parameters, these MR images were normalized by the standard deviation (μ-3σ, μ + 3σ) before feature extraction, and all delineated VOIs were automatically analyzed (Figure 2).
As two radiologists measured the radiomics features to assess reproducibility, we calculated the intraclass correlation coefficient (ICC). When the ICC was > 0.80, consistency was considered excellent.
Features extraction
We extracted 1409 quantitative imaging features from VOIs using the cloud platform big data intelligent analysis (http://radcloud.cn/). The features were categorized into four groups. The first-order statistical features were considered as group 1 (including a total of 18 descriptors), which delineated the distribution of voxel intensities in the MR images through common and basic metrics. Group 2 included shape- and size-based features (containing 14 three-dimensional features) that reflected the shape and size of the lesion areas. Group 3 included features of two-order texture, gray-level co-occurrence, and gray-level run-length texture matrices that were used to calculate those features, and 75 texture features were extracted to quantify the heterogeneity of lesions. The higher-order filter features such as group 4,Laplacian, wavelet, logarithmic, and exponential filters were applied to medical images, and then the first-order statistics and texture features were extracted based on the filtered image (1302 filter features).
Features selection
Model development and validation
The retrospective data (Hospital A) were separated from the training and testing datasets using a random method with a ratio of 7:3, and external data (Hospitals B and C) as the independent validation sets. After feature qualification, based on the selected features, several machine learning classifiers can be used for classification analysis, creating models that can separate or predict MVI-positive data. In this study, radiomics-based LASSO models (machine learning) were constructed using T1WI, T2WI, DWI,AP, PVP, and HBP. We selected K-nearest neighbor (KNN), support vector machine (SVM), extreme gradient boosting (XGBoost), random forest (RF), logistic regression (LR), and decision tree (DT) as the machine learning classifiers, and the effectiveness of the model was improved using the validation method (Figure 2).
Confirmation of radiomics nomogram
R package (version 3.0, http://www.r-project.org/) was used to analyze the radiomics nomogram.Multivariate logistic regression analysis was performed to develop a model for predicting MVI, and all variables associated with MVI at a significant level were candidates for stepwise multivariate analysis.A nomogram was constructed based on the results of the multivariate logistic regression analysis. The receiver operating characteristic (ROC) curve was used to calculate the discrimination performance of the established models, and the values of the area under the curve (AUC) were compared using the Delong non-parametric approach. The calibration of the radiomics model was assessed using calibration curves. External data from the independent validation sets (hospitals B and C) were used to test the performance of the radiomics model. Finally, we constructed decision curves by calculating the net benefits for a range of threshold probabilities.
Statistical analyses
MedCalc 16.2.1 (Ostend, Belgium) and SPSS (version 22.0; Armonk, NY, United States) were used for the statistical analyses. The Kolmogorov-Smirnov method was used to identify the normal distribution of continuous variables. The differences in categorical and continuous variables were compared using theχ2test, Fisher’s exact test, two-samplet-test, or Mann-WhitneyUtest, respectively. ROC analyses were performed to evaluate the predictive performance of MVI for sHCC. The Youden index was used for determining the cut-off values. Then, the AUC, sensitivity, and specificity were calculated, and aZtest was used to compare the differences between the AUCs. Statistical significance was set atP< 0.05.

Figure 2 Flow diagram for the radiomics of machine learning. A: Construct radiomics models, the volume of interest was delineated by experienced radiologists and three-dimensional images were formed, extracting quantitative features by software; B: Pathologic examination, firstly obtaining specimens of small hepatocellular carcinoma tissue, and then taking pathologic diagnosis for microvascular invasion; C: Data cleaning and dimensions reduction; D: Establishing the model for predicting microvascular invasion by machine learning. LR: Logistic regression; KNN: K-Nearest neighbor; SVM: Support vector machine; RF: Random forest.
RESULTS
Patients and serological examinations
A total of 415 patients with qualified sHCC were enrolled in the final study (Figure 1). In hospitals A, B,and C, the mean participant age was 51.2 ± 10.9 (range 29-78) years, 53.04 ± 10.59 (range 28-77) years,and 54.01 ± 10.82 (range 28-85) years, respectively. Histological examination confirmed MVI in 64(28.9%), 22 (23.4%), and 16 (16.0%) patients. The number of patients with hepatitis B, C and alcoholic hepatitis were 162 (73.3%), 21 (9.5%), 29 (13.1%); 71 (75.6%), 10 (10.6%), 8 (8.5%); and 82 (82.0%), 6(6.0%), 2 (2.0%), respectively. The numbers of patients with cirrhosis were 173 (78.3%), 69 (73.4%), and 70 (70%), respectively. The median serum AFP levels were 26.10 (range 0.98-25451.00) ng/mL, 9.34(range 1.09-6740.42) ng/mL, and 31.070 (range 0.713-4587.000) ng/mL, respectively. The median serum total bilirubin levels were 12.5 (range 2.9-64.6) μmol/L, 17.4 (range 3.6-446.9) μmol/L and 13.2 (range 4.4-47.2) μmol/L, respectively. The median direct bilirubin levels were 3.9 (range 1.0-17.0) μmol/L, 4.5(range 1.0-218.9) μmol/L and 5.50 (range 1.50-26.84) μmol/L, respectively. The MELD scores were 13.9 ±4.8 (range 7.0-26.9), 13.8 ± 5.8 (range 6.0-35.5) and 11.8 ± 4.5 (range 5.2-25.6). The number of Child-Pugh classes A, B, and C were 205 (93.2%), 13 (5.9%), 2 (0.9%), 81 (86.2%), 12 (12.8%), 1 (1.1%), 86 (86.0%), 13(13.0%), and 1 (1.0%), respectively. There were 32 (14.5%), 142 (64.3%), 47 (21.2%); 12 (12.8%), 68 (72.3%),14 (14.9%) and 8 (8.0%), 71 (71.0%), 21 (21.0%) cases that were histological grades I, II, and III,respectively (Table 1).
Conventional radiological features
In the group comparison of MVI-positive and negative, the AFP and tumor size were 33.91 (range 1.4-25451.0) and 22.52 (range 0.98-18929.00) (ng/mL) (P= 0.026), 2.34 ± 0.56 and 1.92 ± 0.67 (cm) (P= 0.036)in hospital A; 38.97 (range 1.90-6740.40) and 5.43 (range 1.10-2018.79) (ng/mL) (P= 0.01), 2.43 ± 0.57 and 2.11 ± 0.66 (cm) (P= 0.047) in hospital B; 109.72 (range 0.80-2278.00) and 24.41 (range 0.71-4587.00)(ng/mL) (P= 0.032), 2.47 ± 0.43 and 2.21 ± 0.64 (cm) (P= 0.054) in hospital C. In the MVI-positive group,the proportion of patients with non-smooth tumor margin, incomplete capsule, and peritumoral hypointensity was 39.7% (27/68) (P= 0.019), 40.3% (25/62) (P= 0.02), and 51.5% (17/33) (P= 0.002) in hospital A; 52.9% (9/17) (P= 0.003), 59.5% (25/42) (P= 0.062), and 35.7% (5/14) (P= 0.304) in hospital B;and 31.3% (10/32) (P= 0.004), 14.6% (6/41) (P= 0.759), and 63.6% (14/22) (P= 0.002) in hospital C(Table 2).
For discriminating MVI-positive, in hospital A, B and C the AUC of AFP was 0.597 [95% confidence interval (CI):0.528-0.662], 0.683 (95%CI):0.528-0.662] and 0.669 (95%CI:0.568-0.760), respectively; the AUC of tumor size was 0.675 (95%CI:0.609-0.736), 0.639 (95%CI:0.553-0.735) and 0.576 (95%CI:0.473-0.675), respectively; the AUC of non-smooth tumor margin was 0.580 (95%CI:0.512-0.646), 0.649(95%CI:0.544-0.745) and 0.682 (95%CI:0.581-0.771), respectively; the AUC of incomplete capsule was 0.577 (95%CI:0.509-0.643), 0.595 (95%CI:0.489-0.695) and 0.521 (95%CI:0.419-0.622), respectively; the AUC of peritumoral hypointensity on HBP was 0.582 (95%CI:0.514-0.648), 0.551 (95%CI:0.445-0.654) and 0.667 (95%CI:0.565-0.758), respectively (Table 3).
Radiomics signatures
There were 155 and 66 patients with sHCC in the training and test datasets, respectively. The proportions of MVI-positive patients were 27.1% and 29%, respectively. There were no significant differences in patient characteristics between the training and testing cohorts (P> 0.05). Among the 1409 radiomics features in each T1WI, T2WI, DWI, AP, PVP, and HBP model, 443, 483, 467, 554, 462, and 453 features were selected based on a variance threshold of over 0.80. After LASSO analysis, five, 22, 33,four, eight, and 30 features were selected for T1WI, T2WI, DWI, AP, PVP, and HBP, respectively.
Robustness analysis results
We found that 70.5% (993/1409) of the features extracted from T1WI images had excellent consistency(ICC > 0.8), and all five features selected for modeling had excellent consistency (ICC median, 0.969;minimum, 0.877; maximum, 1.000). The features of 51.9% (731/1409) extracted from T2WI images had excellent consistency (ICC > 0.8), and most of the 22 features selected for modeling had good consistency (ICC median, 0.701; minimum, 0.41; maximum, 0.94). The features of 60.04% (846/1409)extracted from DWI images had excellent consistency (ICC > 0.8), and most of the 33 features selected for modeling had excellent consistency (ICC median, 0.869; minimum, 0.41; maximum, 0.98). The features of 67.8% (956/1409) extracted from AP images had excellent consistency (ICC > 0.8), and the ICC of the four features selected for modeling were 0.902, 0.884, 0.734, and 0.891. The features of 62.1%(875/1409) extracted from PVP images had excellent consistency (ICC > 0.8), and most of the eight features selected for modeling had excellent consistency (ICC median = 0.844, minimum = 0.500,maximum = 1.000). The features of 82.5% (1163/1409) extracted from HBP images had excellent consistency (ICC > 0.8), and most of the 30 features selected for modeling had excellent consistency (ICC median, 0.917; minimum, 0.690; maximum, 1.000).
OMI的SO2卫星监测数据时间为2008年1月—2018年2月,前一年的12月和翌年1月、2月为冬季、3月、4月、5月为春季、6月、7月、8月为夏季、9月、10月、11月为秋季;SO2年总量值以整年各月份柱浓度累加得到。因为环境监测站SO2数据时间较短,所以本研究所用地面监测 SO2的时段为2013年1月—2018年2月。

Table 1 Demographics, alpha fetal protein, bilirubin, tumor characteristics, and microvascular infiltration of the patients with small hepatocellular carcinoma in data sets of three hospitals
Predictive performance of the machine learning classifiers
The machine learning classifiers used in this study were KNN, LR, MLP, RF, SVM, and DT. In general,all classifiers achieved satisfactory performance, with LR being the best machine learning method. To predict MVI, T1WI, T2WI, DWI, AP, PVP, and HBP radiomics models were constructed and validated.In the testing set, the AUCs were 0.776 (95%CI: 0.611-0.895), 0.813 (95%CI: 0.651-0.922), 0.971 (95%CI:0.858-0.999), 0.788 (95%CI: 0.642-0.894), 0.790 (95%CI: 0.630-0.904) and 0.979 (95%CI: 0.911-1.000). In validation hospital B, the AUCs were 0.834 (95%CI: 0.742-0.904), 0.825 (95%CI: 0.732-0.896), 0.816(95%CI: 0.678-0.876), 0.810 (95%CI: 0.715-0.884), 0.847 (95%CI: 0.758-0.913) and 0.970 (95%CI: 0.912-0.994). In validation hospital C, the AUCs were 0.766 (95%CI: 0.672-0.844), 0.761 (95%CI: 0.669-0.839),0.801 (95%CI: 0.710-0.871), 0.824 (95%CI: 0.737-0.892), 0.833 (95%CI: 0.748-0.898) and 0.803 (95%CI: 0.680-0.834) (Figure 3, Table 4).
Development and validation of MVI predicting nomogram
The C-indexes of the radiomics and clinic combined nomogram with the model of T1WI, T2WI, DWI,AP, PVP and HBP were 0.771 (95%CI: 0.695-0.836), 0.895 (95%CI: 0.834-0.940), 0.990 (95%CI: 0.957-0.999),0.774 (95%CI: 0.706-0.833), 0.746 (95%CI: 0.668-0.814) and 0.990 (95%CI: 0.944-0.993) in the training set,respectively; 0.846 (95%CI: 0.594-0.883), 0.917 (95%CI: 0.640-0.915), 0.970 (95%CI: 0.843-0.997), 0.794(95%CI: 0.615-0.876), 0.831 (95%CI: 0.650-0.916) and 0.971 (95%CI: 0.892-0.999) in the testing set,respectively; 0.895 (95%CI: 0.775-0.925), 0.886 (95%CI: 0.746-0.906), 0.843 (95%CI: 0.685-0.881), 0.886(95%CI: 0.695-0.899), 0.918 (95%CI: 0.791-0.934) and 0.912 (95%CI: 0.918-0.996) in validation hospital B,respectively; 0.830 (95%CI: 0.667-0.850), 0.808 (95%CI: 0.654-0.867), 0.869 (95%CI: 0.694-0.899), 0.874(95%CI: 0.674-0.884), 0.870 (95%CI: 0.732-0.887) and 0.808 (95%CI: 0.635-0.892) in validation hospital C,respectively (Figure 4, Table 5).
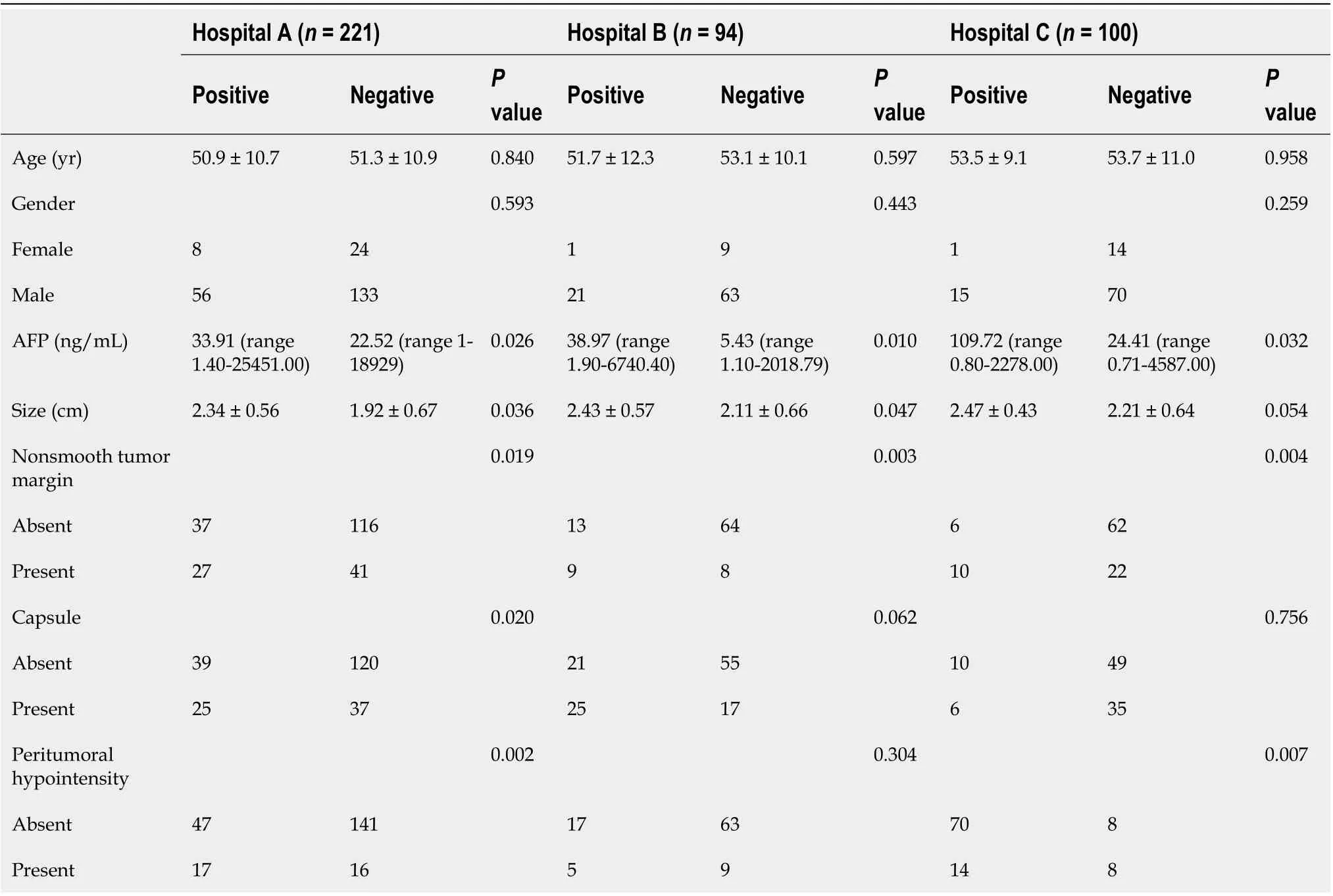
Table 2 Age, gender, alpha-fetoprotein and radiologic features of patients with small hepatocellular carcinoma and relationship with microvascular infiltration
Decision curve analysis showed adequate performance for radiomics nomogram models for predicting MVI in sHCC. The proposed radiomics model to predict MVI showed a greater advantage than the “clinicoradiological” scheme (P< 0.05). There was no significant difference in predictive efficacy between the combination nomogram model and the single radiomics model (P> 0.05)(Figure 5).
DlSCUSSlON
In this multi-center study, we analyzed the clinical and imaging data of 415 patients with sHCC who underwent DWI, Gd-EOB-DTPA-enhanced MRI, and hepatectomy. We used a machine learning approach to construct radiomics signatures and nomogram models for preoperative prediction of MVI and then independently validated the machine learning and nomogram models. Our data showed that clinical and common MRI radiological features, including AFP, tumor size, non-smooth tumor margin,incomplete capsule, and HBP peritumoral hypointensity, have limited diagnostic value for MVI of sHCC. The LR classifier was the best machine learning method, and the radiomics scores of HBP and DWI had great diagnostic efficiency for predicting MVI of sHCC. The nomogram model of combined radiomics scores, APF, and common MRI features exhibited good calibration and discrimination in the training, testing, and independent external validation cohorts.
Gd-EOB-DTPA with a pendant ethoxybenzyl group covalently attached to gadopentetate dimeglumine is a hepatocyte-specific MRI contrast agent that can be taken up by hepatocytesviathe organic anion transporting polypeptides[30]. Gd-EOB-DTPA, which has dual extracellular and hepatobiliary properties that provide structural and functional information on liver lesions, can also provide information on nonspecific gadolinium chelates during dynamic enhancement[31,32]. Granitoet al[33]reported that Gd-EOB-DTPA-enhanced MRI may improve the sensitivity of noninvasive diagnosis of small HCC nodules in patients with cirrhosis, and the double hypointensity in the portal/venous and HBP can be regarded as an MRI pattern, which is highly suggestive of hypovascular hepatocellular carcinoma. This previous study revealed that large tumor size, incomplete capsule, non-smooth tumor margin, peritumoral enhancement on AP, and peritumoral hypointensity on HBP could achieve predictive AUCs of up to 0.85 for MVI of HCC[34]. However, for small HCC (large tumor size ≤ 3 cm),the common MRI radiologic features are smooth tumor margin, complete capsule (or no capsule), and no peritumoral hypointensity in HBP. In this study, the results from three hospitals showed that these conventional MRI radiologic features had limited value in evaluating MVI for sHCC.
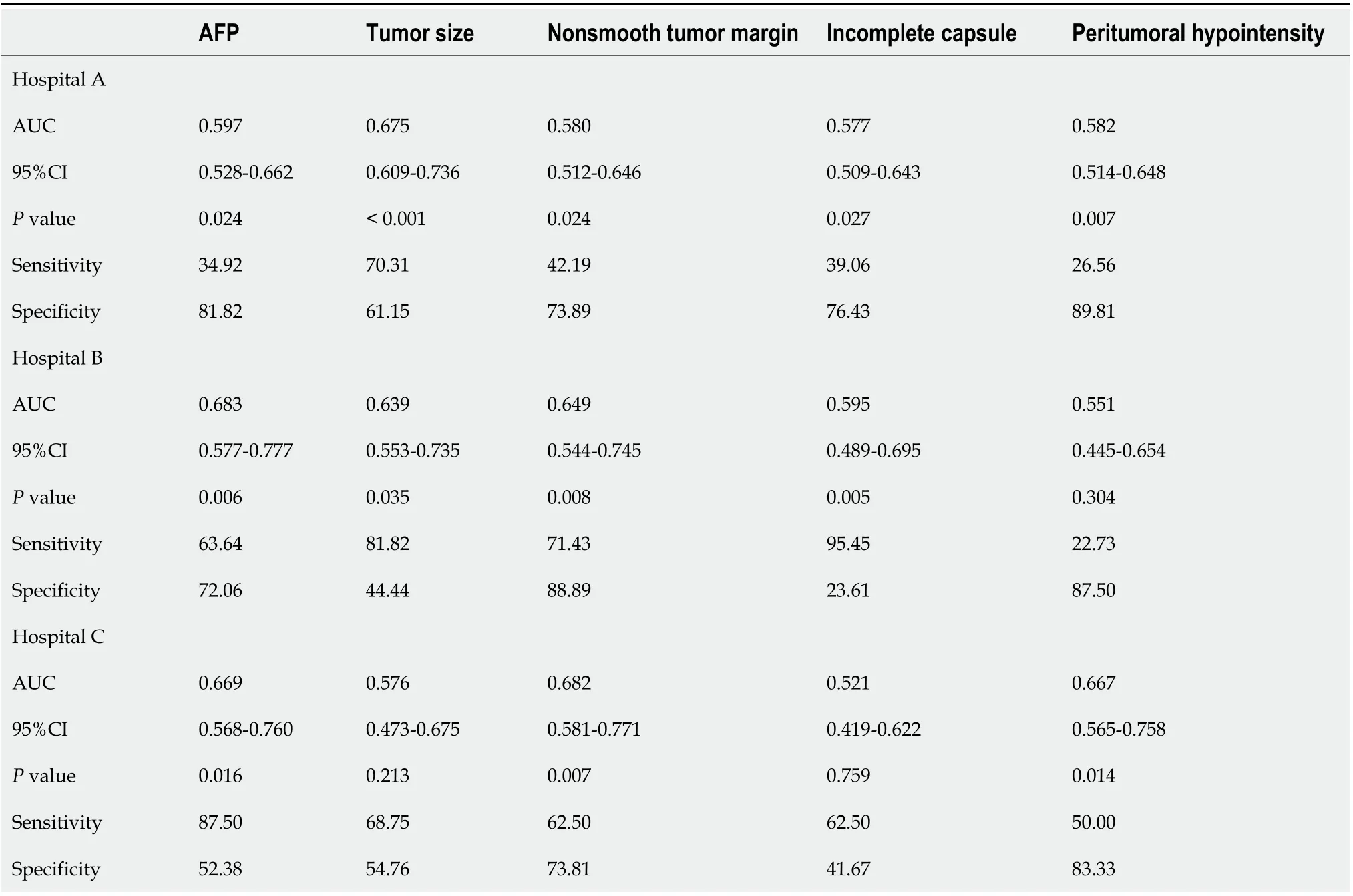
Table 3 Diagnostic performance of alpha-fetoprotein and radiologic features for assessing microvascular infiltration of small hepatocellular carcinoma by receiver operating characteristic curve analysis
Based on these characteristics, we established a Gd-EOB-DTPA MRI radiomics model using machine learning to construct and validate radiomics models for predicting MVI of sHCC. Machine learning has demonstrated capabilities to learn and even master complex tasks, making it useful for computer-aided diagnosis and decision support systems[21]. Radiomics refers to a technique of high-throughput extraction of quantitative imaging features or textures to decode histology and create a highdimensional dataset[35]. However, it was thought that the parameters of the MRI scanner would not have an obvious influence on the results of radiomics analysis after the images were standardized when a previous multi-center study[36] did not demand the same MRI scanners and parameters. However, to minimize the possible influence of other factors, a unified MRI scanner and image standardization process were used in our study. Furthermore, whole-tumor volume analysis was used to decrease sampling bias.
Although previous studies have verified that the radiomics features of CT imaging could predict MVI status in patients with HCC preoperatively, it has high diagnostic efficiency, and the AUC can reach approximately 0.85[27,37]. In addition, Fenget al[38] evaluated Gd-EOB-DTPA-enhanced MRI quantitative features of peri- and intratumoral regions, providing a radiomics model for MVI prediction in patients with HCC. In the validation cohort, the AUC, sensitivity, and specificity were 0.83%, 90.00%,and 75.00%, respectively. However, none of these studies predicted the MVI for sHCC or provided a clinical nomogram. In this study, we extracted radiomics signatures from images of Gd-EOB-DTPAenhanced MRI and then built the model using T1WI, T2WI, AP, PVP, and HBP. The results illustrated that radiomics has the best modeling in HBP and DWI when the LR and classifier of machine learningare utilized, producing great diagnostic efficiency for predicting MVI. Furthermore, the independent external validation results confirmed this efficiency. This may be because the post-Gd-EOB-DTPA contrast enhancement images provide structural and functional information on HBP lesions. The LR algorithm is used to establish a cost function for a classification or regression problem and then solve the optimal model iteratively through the optimization method.

Table 4 Receiver operator characteristic curve analysis of radiomics scores with different sequences of magnetic resonance imaging for predict microvascular infiltration of small hepatocellular carcinoma
Our results also demonstrate that the radiomics characteristics of DWI images can accurately predict the MVI of sHCC. DWI is an MRI technology that can reflect the motion of water moleculesin vivoand can be used to assess tumor cellularity[39]. HCC with MVI is more likely to have higher cellularity and poor differentiation than HCC without MVI[40]. Okamuraet al[41] suggested that the apparent diffusion coefficient (ADC) value is a valuable predictor of poor differentiation and MVI and is significantly related to tumor recurrence. Kimet al[42] illustrated that the tumor-to-liver ADC ratio was a significant independent parameter for the MVI of sHCC and the degree of lymphocyte infiltration.Our research further extracted the radiomics characteristics of the tumor, which were based on DWI images that confirmed that the quantitative characteristics of the radiomics had good performance for predicting the MVI of sHCC.
A nomogram was built in our study, which converted each regression coefficient proportionally in multivariate logistic regression to a 0- to 100-point scale. The effect of features with the absolute value of the highest β coefficient was assigned 100 points. The total points of the independent variables were converted to the predicted probabilities. The concordance index (C-index) was used to predict the performance of the nomogram and calibration with 1000 bootstrap samples to decrease the overfittingbias[43]. Our study incorporated six factors: radiomics signatures, APF, tumor size, non-smooth tumor margin, incomplete capsule, and peritumoral hypointensity. Radiomics combined with the clinicoradiological factors nomogram model achieved good concordance indices in predicting MVI in the training and validation cohorts. In particular, the nomogram with HBP and DWI radiomics model showed excellent predictive efficiency in the two external validation datasets, and decision curve analysis further confirmed the clinical usefulness of the nomogram.

Table 5 Predictive performance of the nomogram prediction model for estimating the risk of microvascular infiltration presence in patients with small hepatocellular carcinoma
Nonetheless, this study had several limitations. First, the included patient population in this study had an inevitable bias in the inter-center distribution, although the application of radiomics and clinical nomogram was ensured by the multi-center nature of this study. To investigate the impact factors of bias on the baseline, we analyzed the age, AFP levels, liver function, and tumor size. Further larger-scale studies with more balanced subjects are needed to validate our results. Second, given the difficulty of collecting scalable medical imaging data for small HCC, many patients with small HCC who underwent transarterial chemoembolization or ablation could not be enrolled in the model of radiomics signatures and clinical nomogram to predict MVI. Given larger medical imaging datasets, deep networks are expected to improve prediction accuracy. Third, due to the lack of prognostic analysis in this study, we analyzed the different prognoses of sHCC patients with positive and negative MVI, which were predicted using a radiomics nomogram.
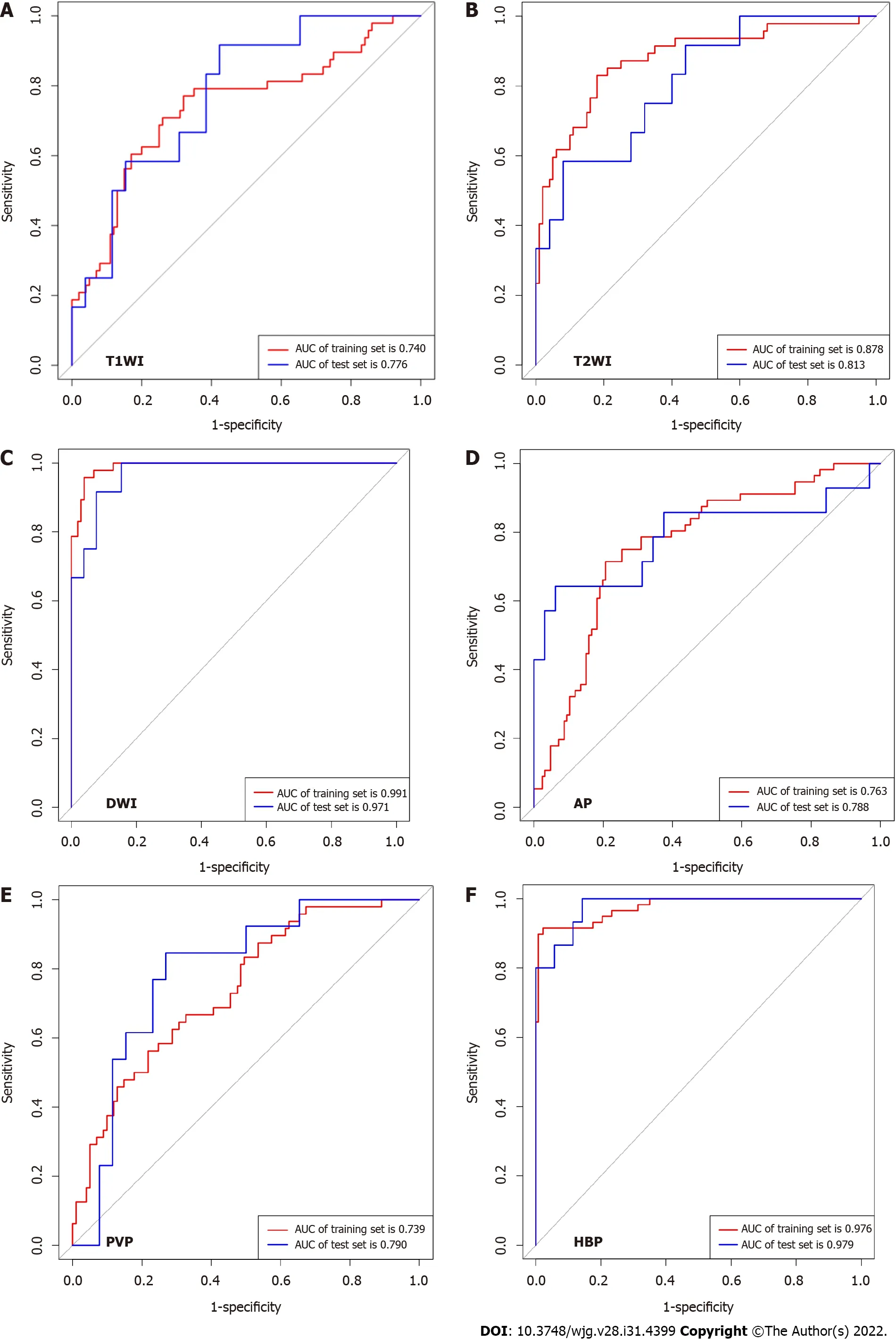
Figure 3 Receiver operating characteristic curve of different radiomics models for diagnosis microvascular invasion in small hepatocellular carcinoma (testing set). A: T1 weighted imaging [area under curve (AUC) was 0.776; 95% confidence interval (CI): 0.611-0.895]; B: T2 weighted imaging [AUC, 0.813; 95% confidence interval (CI): 0.651-0.922]; C: Diffusion weighted imaging (AUC, 0.971; 95%CI: 0.858-0.999); D: Arterial phase (AUC, 0.788;95%CI: 0.642-0.894); E: Portal vein phase (AUC, 0.790; 95%CI: 0.630-0.904); F: Hepatobiliary phase (AUC, 0.990; 95%CI: 0.911-1.000). T1W1: T1 weighted imaging; T2W2: T2 weighted imaging; AUC: Area under curve; DWI: Diffusion weighted imaging; AP: Arterial phase; PVP: Portal vein phase; HBP: Hepatobiliary phase.

Figure 4 Nomogram of diffusion weighted imaging radiomics model to predict microvascular invasion in patients with small hepatocellular carcinoma. A: The nomogram was developed with radiomics signature and clinicoradiological factors. A vertical line was drawn according to the value of radiomics scores to determine the corresponding value of points. Similarly, the points of tumor markers were determined. The total points were the sum of the two points above. Finally, a vertical line was made according to the value of the total points to determine the probability of microvascular invasion (MVI); B: Validity of the predictive performance of the nomogram in estimating the risk of MVI presence in the training cohort; C: Validity of the predictive performance of the nomogram in estimating the risk of MVI presence in the validation cohort. AFP: Alpha-fetoprotein; DWI: Diffusion weighted imaging; Rad_score: Radiomics signatures score.
CONCLUSlON

Figure 5 Decision curve analysis. A and B: Decision curve analysis of the prediction model for training (A) and testing (B) cohort. Y-axis represents the net benefit, which is calculated by gaining true positives and deleting false positives. The X-axis is the probability threshold. The curve of the radiomics and combined nomogram over the clinical features that integrated AFP and radiological signatures showed the greatest benefit. AFP: Alpha-fetoprotein; Rad_score: Radiomics signatures score.
In conclusion, our study revealed that AFP and conventional Gd-EOB-DTPA-enhanced MRI features have poor diagnostic accuracies for MVI in sHCC. The radiomic signatures of HBP and DWI can further improve the ability to predict MVI. Furthermore, as a noninvasive preoperative prediction method, the radiomics nomogram showed favorable predictive accuracy for evaluating MVI in sHCC, which may help reassess the clinical therapeutic regimen for patients with sHCC.
ARTlCLE HlGHLlGHTS

Research perspectives
This clinical prediction model may help in the selection of treatment options for small HCC.
ACKNOWLEDGEMENTS
The authors would like to thank Yingying Ezell for the language recheck and editing, Fuling Huang for his technical support, and Huiting Zhang (Siemens Healthineers, Wuhan, Hubei Province, China) for her constructive suggestions during the MRI scanning.
FOOTNOTES
Author contributions:Chen YD and Zhang L contributed equally to this work; Chen YD and Long LL was the guarantor and designed the study; Zhang L, Lin B, Jiang ZJ, Tang C, Dang YW, and Xia YW participated in the acquisition, analysis, interpretation of the data, and drafted the initial manuscript; Zhou ZP and Song B revised the article critically for important intellectual content.
Supported bythe National Natural Science Foundation of China, No. 82060310; and Science and Technology Support Program of Sichuan Province, No. 2022YFS0071.
lnstitutional review board statement:The study was reviewed and approved by The First Affiliated Hospital of Guangxi Medical University Ethical Review Committee, No. 2019 KY-E-65.
lnformed consent statement:All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement:There are no conflicts of interest to report.
Data sharing statement:The data that support the findings of this study are available in the Baidu Netdisk or our AI Scientific Research Platform (https://mics.radcloud.cn/). Further enquiries can be directed to the corresponding author.
STROBE statement:The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Yi-Di Chen 0000-0001-6293-4624; Ling Zhang 0000-0001-7270-3555; Yi-Wu Dang 0000-0002-7793-1239;Bin Song 0000-0002-7269-2101; Li-Ling Long 0000-0003-3369-8532.
S-Editor:Chen YL
L-Editor:Filipodia
P-Editor:Yuan YY
 World Journal of Gastroenterology2022年31期
World Journal of Gastroenterology2022年31期
- World Journal of Gastroenterology的其它文章
- Duodenal-jejunal bypass reduces serum ceramides via inhibiting intestinal bile acid-farnesoid X receptor pathway
- Preoperative contrast-enhanced computed tomography-based radiomics model for overall survival prediction in hepatocellular carcinoma
- Prevalence and clinical characteristics of autoimmune liver disease in hospitalized patients with cirrhosis and acute decompensation in China
- Application of computed tomography-based radiomics in differential diagnosis of adenocarcinoma and squamous cell carcinoma at the esophagogastric junction
- Insights into induction of the immune response by the hepatitis B vaccine
- Low-grade myofibroblastic sarcoma of the liver misdiagnosed as cystadenoma: A case report
