Effects of post-dilation on coronary blood flow and MACE events following primary percutaneous coronary intervention in patients with STEMI
Meng-Cheng Xu, Hua-Su Zeng, Li Fan, Yang Zhuo, Jun Gu, Jun-Feng Zhang, Yu-Qi Fan,Chang-Qian Wang
Department of Cardiology,Shanghai Ninth People′s Hospital,Shanghai Jiao Tong University School of Medicine,Shanghai 200011,China
Keywords:Post-dilation Primary PCI STEMI No-reflow Slow-flow
ABSTRACT Objective: This retrospective cohort study aimed to evaluate the effect of post-dilation on coronary blood flow and MACE events during hospitalization and 1 year follow-up following primary PCI in patients with ST-segment. Methods: 419 eligible patients who underwent PPCI due to STEMI between January 2015 and October 2019 were enrolled. The CTFC, final QCA, and the incidence of no-reflow/slow-flow during different procedure moments were assayed. Study end points was to compare two groups of patients with clinical characteristics,compared two groups of patients with the incidence of no-reflow and slow-flow, and the incidence of MACE during hospitalization and 1-year follow-up. Results: The incidence of final no-reflow/slow-flow in the post-dilation group was not significantly higher than that in the non-post-dilation group (24.3% vs.19.4%; p = 0.238).There was no significant statistical difference in MACE events during hospitalization, but for the 1-year follow-up, the incidence of Target vessel revascularization and Target lesion revascularization in the post-dilation group was lower than that in the non-post-dilation group. A multivariable logistic regression model revealed that age (OR=1.078, 95%CI=1.038-1.120; P <0.001), history of diabetes (OR=3.009,95%CI=1.183-7.654; P =0.021), post-dilation (OR=0.192, 95%CI=0.067-0.549; P=0.002) were independently correlated with long-term follow-up of MACE.Conclusion: Post-dilation does not increase poor prognosis during hospitalization, and reduces the incidence of TVR and TLR events during long-term follow-up.
1. Introduction
Post-dilation is an procedure in which a non-compliant balloon is applied after stent release to perform high-pressure dilation within the stent to facilitate adequate stent expansion and good apposition.In the current era of drug stent stenting, post-dilation is widely recommended in elective PCI given that incomplete stent expansion and poor apposition are the major predictors of in-stent thrombosis and restenosis[1]. However, Primary PCI(primary percutaneous coronary intervention(PPCI)in acute ST-segment elevated myocardial infarction(STEMI)is often associated with no-reflow/slow-flow phenomenon (noted as no-reflow/slow-flow onward), a phenomenon in which the epicardial coronary vessels have been deconfined, but distal antegrade flow is lost (i.e., thrombolysis in myocardial infarction[TIMI] 0-1 flow or referred to as “no-reflow”)or significantly slowed (i.e., TIMI 2 flow or referred to as “slowflow”), resulting in failure to maintain myocardial perfusion. The occurrence of no-reflow/slow-reflow phenomenon increases the risk of poor prognosis in patients, and a small sample of randomized controlled clinical studies suggests that routine post-dilation in PPCI increases the risk of no-reflow/slow-flow[2].Therefore,interventionalists generally try to avoid post-dilation during PPCI in clinical practice. However, the clinical situation is ever-changing.In PPCI, sometimes the interventional physician will perform postdilation according to his own judgment that it is necessary. There have been few reports on the characteristics of post-dilatation lesions determined by the interventionists in this PPCI and its influence on the prognosis of patients. Through the analysis of data from our center, this study reviewed and analyzed the clinical application status of post-dilation in PPCI and its effect on coronary blood flow, hospitalization and long-term follow-up prognosis.
2. Materials and methods
2.1 The research object
STEMI patients successively enrolled in the Shanghai Ninth People's Hospital Affiliated to Shanghai Jiao Tong University School of Medicine from January 2015 to October 2019.
Inclusion criteria: conforming to the diagnostic criteria of the guidelines for acute ST elevation myocardial infarction [3];STEMI patients who underwent Primary PCI within 12 hours of chest pain and successfully implanted stents.
Exclusion criteria: patients with cardiac shock; STEMI patients secondary to stent restenosis; The criminal vessels had complex lesions such as pseudoaneurysm, bifurcated lesions with double stents; Dilated with kissing balloon;Stents were implanted in two or more criminal vessels within one procedure, or atherectomy was used for calcified lesions. Patients with incomplete images were also excluded.
There were 419 patients who met the enrollment criteria, and they were divided into post-dilation group and non-post-dilation group according to whether the patients underwent post-dilation after stent implantation, of which 259 (61.8%) were in the post-dilation group and 160 (38.2%) were in the non-post-dilatation group, and the study was approved by the ethics committee of our hospital.
2.2 Procedure and Medication
Patients routinely chewed aspirin 300 mg, clopidogrel 300-600 mg or ticagrelor 180 mg before the procedure. All PCI procedures were performed according to PCI guidelines [3]. The procedure was performed either by transradial or transfemoral route. Drug-eluting stents (DES) were used in all patients. In case of intraoperative noreflow/slow flow, the operator injected intracoronary adenosine,nitroprusside or tirofiban as appropriate.If there were no contraindications, statins, beta-blockers, and angiotensin-converting enzyme inhibitors were routinely used postoperatively.
2.3 Observation indexs and detection method
(1) Clinical baseline information: including demographic characteristics, major laboratory tests, and other indicators. It mainly depends on electronic medical records and telephone follow-up.
(2) Coronary angiography data: All angiography images were read and results recorded by two interventional cardiologists who were unaware of the purpose of the study. The corrected TIMI frame count (CTFC) and the postoperative qualitative comparative analysis(QCA) index were measured and recorded at different moments of the procedure. Among them: 1) Quantitative coronary angiography(QCA): was performed by two interventional cardiologists using the QCA-CMS (Medis Medical Imaging Systems bv, Leiden, the Netherlands Netherlands; Medical Imaging Systems, Leiden, the Netherlands). Calibration was performed using a guide catheter filled with contrast; minimum lumen diameter and reference vessel diameter were measured from orthogonal projections in diastolic frames using conventional methods [4]; 2) Thrombolysis in myocardial infarction (abbreviated TIMI ): according to the TIMI classification [5] coronary The corrected TIMI frame count (CTFC):counts the number of frames required to visualize the coronary vessels from the start of contrast shading to a standardized distal marker [6]. The CTFC values were measured independently by interventional cardiologists according to the criteria defined in the reference study [7]. Landmarks used in this study were as follows: the first branch of the posterolateral artery in the right coronary artery(RCA), the distal branch of the lateral left ventricular wall artery in the circumflex system (LCX), and the distal bifurcation known as the “moustache” in the left anterior descending artery (LAD). In general, the CTFC in the RCA was assessed in left anterior oblique cranial view, and the CTFC in the LCX and the LAD was quantified in right anterior oblique caudal view. When the image acquisition seed is 30 frames/second, the CTFC values of normal coronary blood flow should fall within the following ranges: LAD (21.1±2.1 frames, after correction by dividing 1.7 due to the longer length of LAD); LCX (22.2±4.1 frames); RCA (20.4±3 frames). The CTFC values were measured individually before and after the post-dilation procedure using angiography. The blood flow was categorized as noreflow/slow-flow when the CTFC is 2 frames larger than the normal range mentioned above. CTFC was set as 100 frames for TIMI 0-1 flow. Higher CTFC value represents worse coronary blood flow.
2.4 Research endpoint
Main research end point was: 1)to compare two groups of patients with clinical characteristics and pathological lesions features; 2)to compare the incidence of no-reflow/slow -flow rates;3)to compare the differences of major adverse cardiovascular events (MACE)during hospitalization and 1-year follow-up, including cardiac death,non-cardiac death, nonfatal MI, and target vessel revascularization(TVR) between two groups were compared. The hospitalization MACE, comprising of cardiac death,nonfatal myocardial infarction(nonfatal MI), and target vessel revascularization (TVR). The 1-year follw-up of MACE, consisting of cardiac death, targetvessel revascularization, and target lesion revascularization (TLR). Cardiac death was defined as any death attributable to a cardiovascular event(e.g., myocardial infarction, low output failure, fatal arrhythmias).Non-fatal MI was defined as, after 48 hours of PPCI, the elevation of creatine kinase myocardial band (CK-MB) or troponin level by two-fold of the upper limit of normal, accompanying one or more of the following symptoms: new/recurrent sustained ischemic chest pain, hemodynamic decompensation, or new/recurrent ST elevation/depression of ≥0.1 mV. TVR is defined as any repeat percutaneous intervention or surgical bypass of any segment of the target vessel despite the stent restenosis. Target lesion revascularization is defined as in-stent restenosis, which involves revascularization of the lesion site of the target vessel.
2.5 Statistic method
SPSS 25.0 software was used for statistics in this study.Measurement data were expressed as mean ± standard deviation(±s). Normally distributed continuous variables are shown as mean ± standard deviation and compared with Student’s t-test,while non-normally distributed continuous variables were shown as median with interquartile and compared with Mann-Whitney U test. Categorical variables were shown as frequencies and compared using either the chi-square (χ²) or Fisher exact test as appropriate.Using multiple Logistic regression analysis of risk factors for 1 year follow-up MACE events. A p-value less than 0.05 (i.e., p<0.05) was considered statistically significant.
3. Results
3.1 Basic clinical characteristics
As shown in Table 1, there were no statistical differences between the two groups in age, gender, hypertension, diabetes, atrial fibrillation, family history, previous history of PCI, Pain to balloon time. There were also no statistical differences for laboratory parameters such as peak CKMB, C - reactive protein, platelet, uric acid, glycosylated hemoglobin, total cholesterol, triglyceride, low density lipoprotein cholesterol (LDL-C). Patients in the post-dilation group had higher peak Troponin-T and lower creatinine levels on admission compared with non-post-dilation group. There was no significant difference between the two groups in using the antiplatelet agents. However, The post-dilation group has a higher rate of GPIIb IIIa inhibitors using (82.2% vs.53.8%; P=<0.001).
3.2 QCA results
3.2.1 Comparison of the basic coronary arteriography data and lesion characteristics
As shown in Table 2, both groups had similar results, in terms of the distribution of culprit vessel, culprit vessel location and thrombus aspiration (p>0.05). There was no difference existed between the post-dilation and non-post-dilation group in the following parameters: pre-dilation balloon diameter and length, biggest inflation pressure, or dilation time. Completely occluded lesion and direct stent implantation without pre-dilation is more frequent in the non-post-dilation group (p<0.05). Patients in the post-dilation group were more likely to have calcium plaque (22.8% vs. 12.5%;p=0.09), longer stent (28.32±6.78 mm vs. 26.23±6.85 mm; p=0.002),bigger stent diameter (3.24±0.46 vs. 3.09±0.44 mm; p=0.001), and overlapping stents (14.3% vs. 7.5%; p=0.036).
3.2.2 Comparison of coronary blood flow
As shown in Table 3, there was no significant difference in preoperative TIMI blood flow between the two groups, but the preoperative CTFC value of the post-dilation group (85.65 27.94 vs.78.02 32.36; P=0.011) and CTFC immediately after stent release(24.90 13.09 vs.22.23 7.07; P=0.018) was lower than that in nonpost-dilation group. There was no significant difference in TIMI blood flow and CTFC value between the two groups. According to the criterion of no-reflow/slow-flow, the incidence of no-reflow/slow-flow in the non-post-dilation group was slightly higher than that in the post-dilation group (14.4% vs.11.2%; P=0.338) at the stent released moment, but the incidence of no-reflow/slow-flow in the post-dilation group was slightly higher than that in the nonpost-dilation group, and there was no significant difference betweenthe two groups(24.3% vs.19.4%; P=0.238) at the final angiography.There was no statistical difference in the postoperative reference vessel diameter (RVD) measured by QCA between the two groups, but the minimum lumen diameter (MLD, MLD, 2.27±1.38 vs.1.90±2.01, P=0.022) and vessel diameter stenosis rate (DS%,19.49±6.18 vs. 17.50± 9.10, p = 0.023) in the post-dilation group was significantly higher than that of the non-post-dilation group, and the difference was statistically significant.
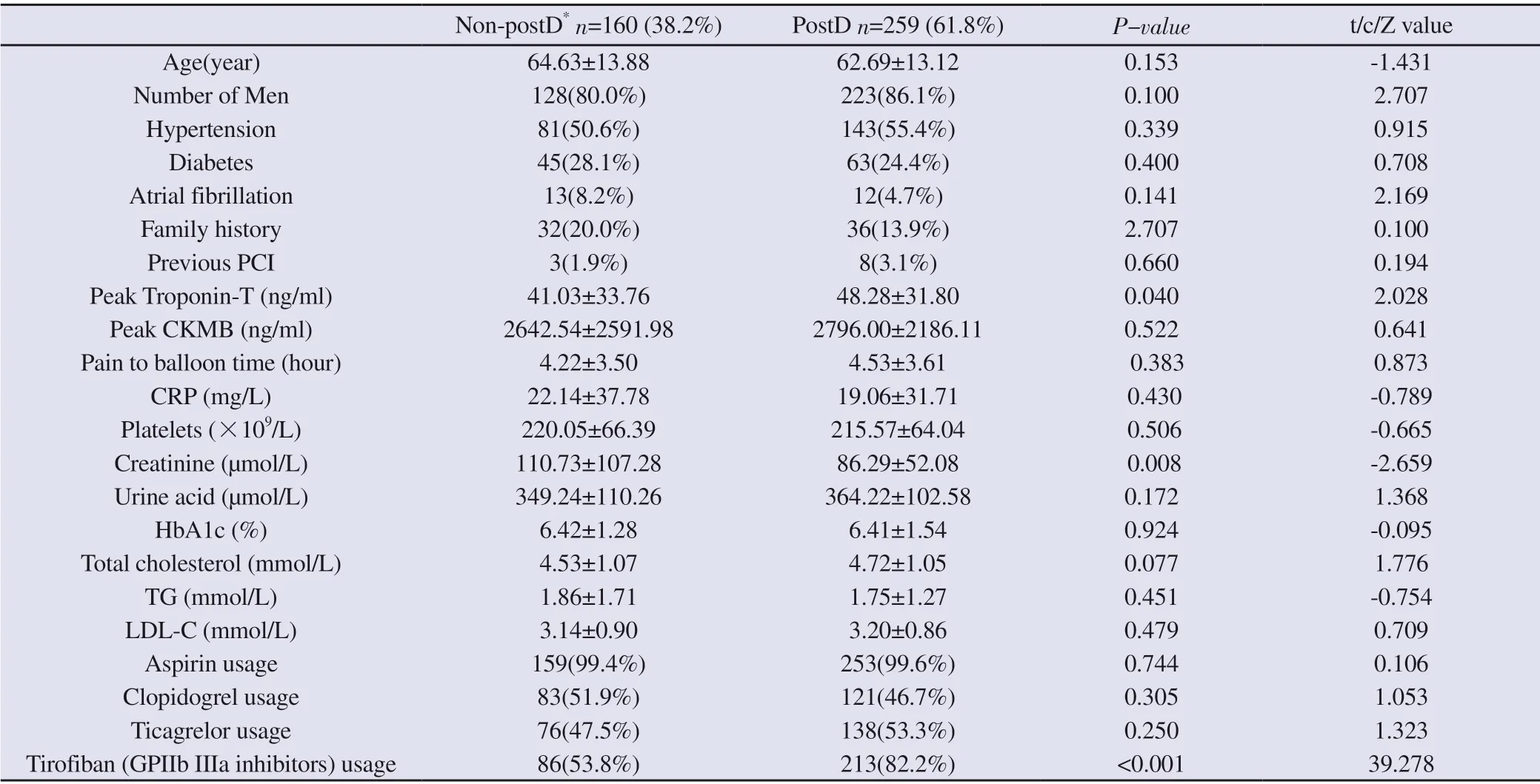
Table 1 Baseline clinical characteristics
3.3 clinical prognosis
3.3.1 Comparasion of the incidence of MACE for both hospitalization and 1-year of follow-up
The incidence of MACE events in the post-dilation and nonpost-dilation group is shown in Table 4. The incidence of MACE events during hospitalization was 3.1% and 1.9% in the non-postdilated and post-dilated groups, respectively (P=0.654), including cardiac death, non-fatal myocardial infarction(non-fatal MI), and TVR events, which were not statistically significantly different.The incidence of MACE events at 1-year follow-up was 9.3% vs.2.3% in the non-post-dilated and post-dilated groups, respectively( P=0.001), with the incidence of TVR (3.1% vs. 0.7%) and TLR(5.0% vs. 0.3%) events being higher in the non-post-dilation group than in the post-dilated group, and the difference in TLR events was statistically different(p=0.005).
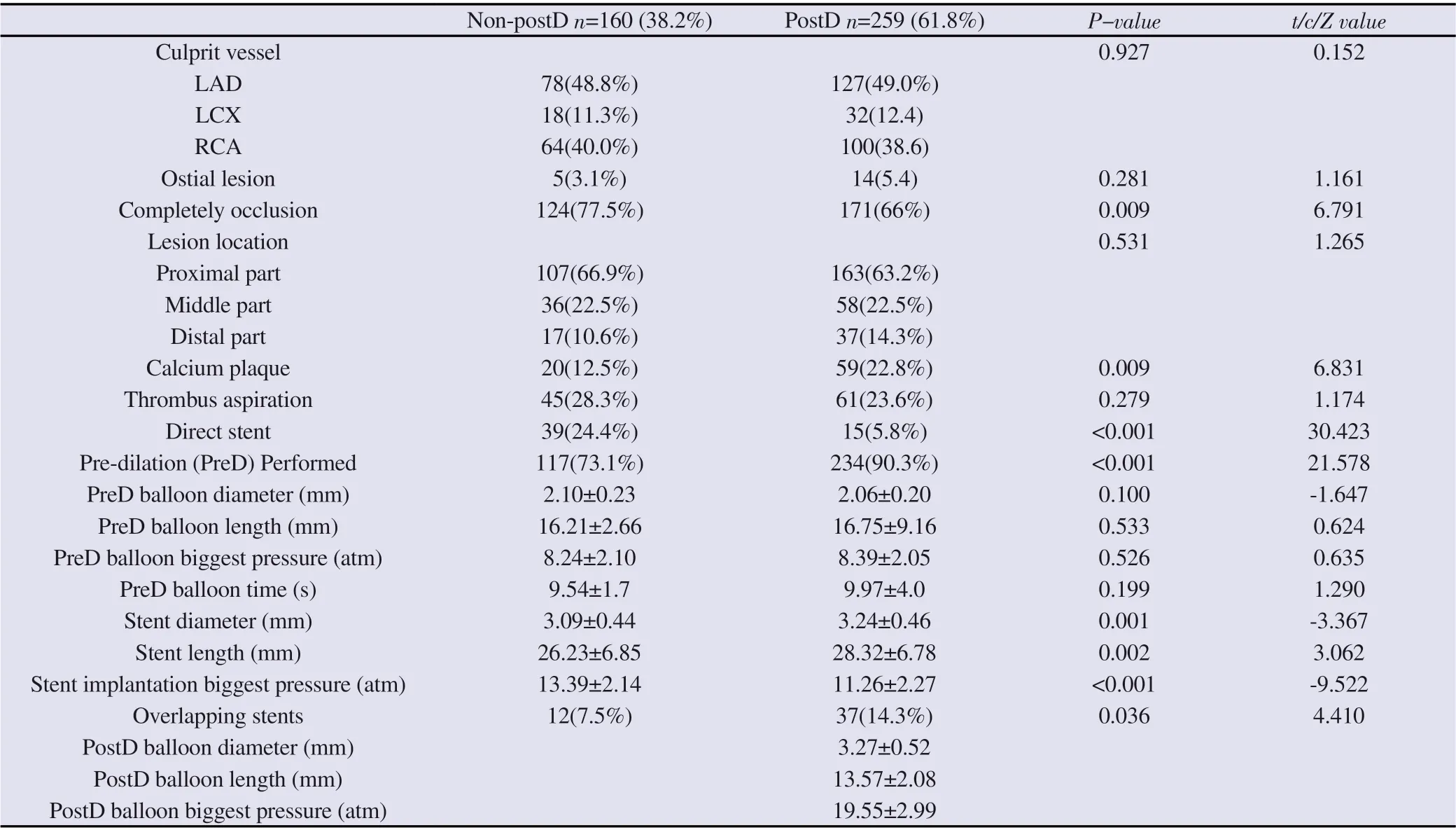
Table 2 QCA analysis results
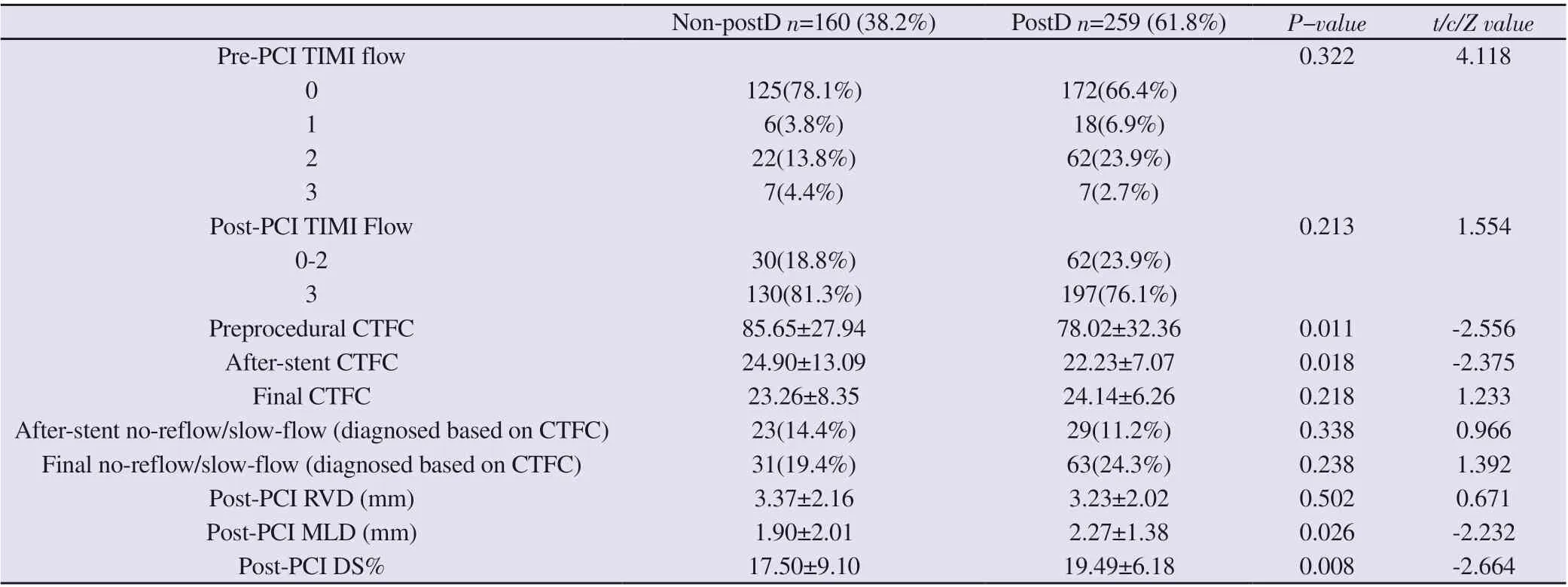
Table 3 Correlative indexes of coronary blood flow
3.3.2 Analysis of independent factors influence MACE events at 1-year follow-up
As in Table 5, variables associated with MACE events screened by univariate analysis were subjected to multiple regression analysis with P<0.01 entered into the equation, in which 4 variables, age,history of hypertension, history of diabetes mellitus, and postdilation, were included in the multiple logistic regression model. The results showed that age (OR=1.078, 95% CI=1.038-1.120; P<0.001),history of diabetes (OR=3.009, 95% CI=1.183-7.654; P=0.021), and post- dilatation (OR=0.192, 95% CI=0.067-0.549; P=0.002) were independently associated with the occurrence of 1-year follow-up MACE events.
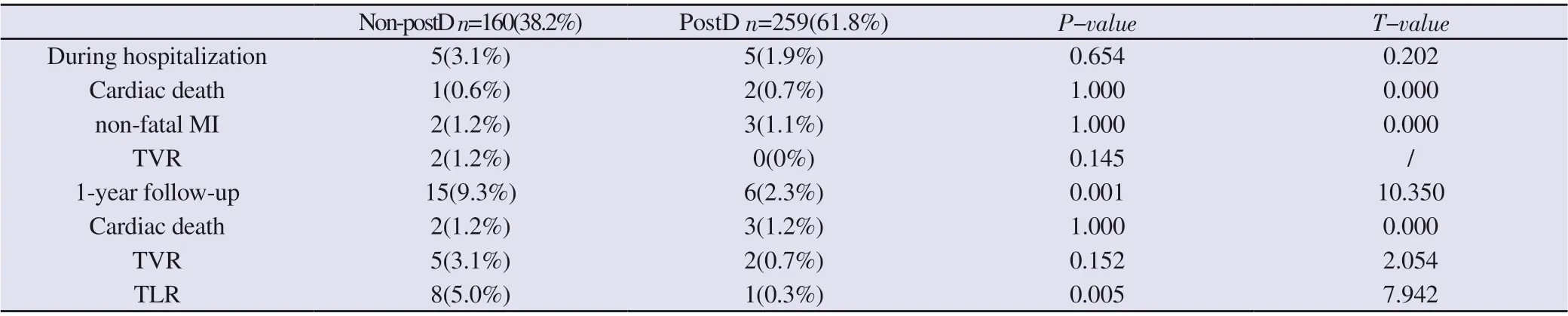
Table 4 Relationship between post-dilation and MACE during hospitalization and 1- year follow-up
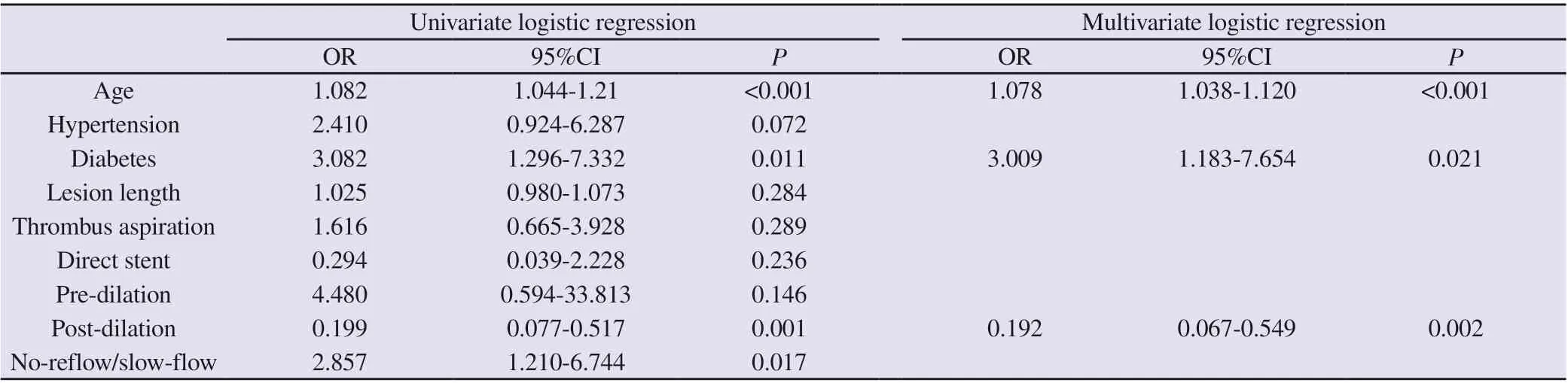
Table 5 Univariate and multivariate logistic regression analysis of independent influencing factors of MACE during 1-year follow-up
4. Discussion
Acute ST-segment elevation myocardial infarction (STEMI) is a symptom of myocardial necrosis caused by acute and persistent complete occlusion of coronary arteries resulting in ischemia and hypoxia. Its main mechanism is thrombosis based on the rupture of coronary atheromatous plaque, which is characterized by rapid onset, rapid changes and high mortality. Reperfusion therapy is the most effective salvage measure for STEMI patients. And primary PCI (PPCI) can open the infarct-related artery in time, restore the antegrade blood flow and reduce the infarction area, which is the most effective reperfusion strategy for treating STEMI patients.However, although this method can effectively open the epicardial blood supply, it does not mean that the myocardial blood supply is restored, and the absence of good restoration of myocardial blood supply at the myocardial level is often manifested as the no/slow flow phenomenon. The no/slow flow phenomenon significantly reduces the efficacy of PPCI and increases the incidence of in-hospital death,malignant arrhythmias, and heart failure. The pathophysiological mechanisms underlying the no-/slow-flow phenomenon are complex and include distal thromboembolism, ischemia-reperfusion injury,microvascular spasm, and endothelial dysfunction [8,9,10]. The noreflow/slow-flow phenomenon occurs in approximately 5%-50% of cases during intracoronary interventions, including more commonly in PPCI for acute coronary syndromes (ACS) [11,12].During PPCI,most of the culprit lesions are accompanied by surface thrombosis,while the endothelium is in the acute inflammatory phase, and the endothelium is relatively fragile. During the mechanical operation of stent implantation, high-pressure expansion and release of the stent will aggravate the thrombus and atheromatous plaque tissue detachment, distal vessel embolism, and microvascular spasm, and there is a risk of no-reflow/slow flow. Therefore, how to reduce the risk of no-reflow/slow-flow in PPCI has been of great concern to interventionalists.
Post-dilation after stent implantation with a high-pressure balloon facilitates adequate stent expansion and good wall apposition and is widely recommended in elective PCI, especially in bifurcation lesions, calcified lesions and long stents and tandem stents, where post-dilation is generally routinely given [13,14,15]. The impact of post-dilation during primary PCI for acute ST-segment elevation myocardial infarction (PPCI) on the risk of no-reflow/slowflow and clinical prognosis remains controversial. Zhang [1] was the first to suggest that post-dilation increases the risk of death/myocardial infarction in patients with AMI, and Karjalainenet et al.[16] suggested that post-dilation reduces nonfatal MI events, but the MACE difference was not statistically significant. Saadat et al. found that post-dilation reduced device-related event endpoints, particularly target lesion/target vessel revascularization [17 18]. Karamasis GV et al. showed that post-dilation may facilitate improved stent apposition and adequate dilation and increase flow reserve fraction after percutaneous coronary intervention without significant effect on coronary microcirculation [19]. Some studies have used finite element modeling to confirm that post-dilation helps to obtain a larger official lumen area after PCI [20]. It is clearly not realistic enough to use endoluminal imaging to guide optimal stent implantation in every primary PCI in real clinical practice [21,22], and PPCI operators also encounter long stents, tandem stents, and calcified lesions where the operator may have to use post-dilation. Analysis of data from our center found that the percentage of post-dilation in PPCI was as high as 61.8% in clinical practice, and patients using post-dilation had more calcified lesions, longer stents, and a higher percentage of tandem stents, suggesting that the rationale for the operator's choice of post-dilation is similar to that of elective PCI. In addition,CTFC of coronary blood flow on immediate stent implantation was significantly better in patients who performed post-dilation than in the non-post-dilation group, suggesting that operators are concerned about the increased risk of no-reflow/slow-flow with post-dilation and will try to avoid post-dilation in patients who have signs of slow flow after stent implantation but are still able to tolerate it. In this study, the incidence of postoperative no-reflow/slow-flow was 24.3%and 19.3% in the post-dilatation and non-post-dilatation groups,respectively, which was numerically higher in the post-dilatation group than in the non-post-dilatation group, but there was no significant difference in the statistical analysis, which may be related to the group bias caused by non-randomized grouping. However,considering that the CTFC of coronary flow on immediate stent implantation was significantly better in post-dilation patients than in the non-post-dilation group, the incidence of no-reflow/slow-flow between the two groups after post-dilatation may still be significant.
In this study, prognostic analysis during hospitalization showed no statistically significant difference in the incidence of MACE events between the two groups. 1-year follow-up of MACE events revealed a lower incidence of TVR and TLR in the post-dilatation group than in the non-post-dilatation group. Multiple regression analysis suggested that MACE events during hospitalization were independently associated with age, history of diabetes mellitus, and postdilatation. This result is consistent with the correlation data read from QCA, where postdilation improved MLD, DS% metrics and optimized stent apposition, resulting in fewer adverse events. It is suggested that in clinical practice, although post-dilation during PPCI has the potential to increase the risk of no-reflow/slow-flow,stent post-dilation decided by the operator on a case-by-case basis can improve long-term prognosis by optimizing the stent-to-lumen reference area and warrants further study in a large sample.
Due to the small sample size and retrospective nature of this study,prospective randomized controlled trials are needed to clarify the need for post-dilation with a non-compliant balloon in STEMI patients undergoing primary PCI.
Author’s Contribution
First author: Meng-Cheng Xu: Participated in the selection and design of the topic, implementation of the experiment, data compilation and statistics, and execution of the paper.
Corresponding author: Changqian Wang: Participated in the selection and design of the topic, reviewer.
Other authors: Zeng Huaxu, Fan Li, Zhuo Yang, Gu Jun, Zhang Junfeng, Fan Yuqi: all were coronary interventionalists and participated in the acquisition of surgical data.
 Journal of Hainan Medical College2022年11期
Journal of Hainan Medical College2022年11期
- Journal of Hainan Medical College的其它文章
- Study on the mechanism of “Salvia chinensis and Radix Ranunculi Ternati” drug pair in the treatment of lung cancer
- Potential targets and mechanism of Xingxiao Pill for the treatment of lung cancer were analyzed based on network pharmacology and molecular docking
- Effect of total glucosides of paeony on serum cytokines in patients with psoriasis and its clinical efficacy: A meta-analysis
- Correlation study between dendritic cell and eosinophil in refractory rhinosinusitis
- An exploration on the protective mechanism of Xuduan Zhongzi prescription against epididymis oxidative damage in oligoasthenospermia model rats based on Nrf2-NQO1/γ-GCS signaling pathway
- Effects of compatibility of Scutellaria baicalensis stems and Polygonum cuspidatum on TRPV1 expression and inflammatory cytokines in rats with acute lung injury
