Recurrence rates after endoscopic resection of large colorectal polyps: A systematic review and metaanalysis
Carola Rotermund,Roupen Djinbachian, Mahsa Taghiakbari, Markus D Enderle, Axel Eickhoff, Daniel vonRenteln
Abstract
Key Words: Colonoscopy; Adenoma; Polyp; Endoscopic mucosal resection; Colorectal cancer
lNTRODUCTlON
Complete endoscopic polyp removal is especially important for large colorectal polyps in order to prevent local polyp recurrence and progression to colorectal cancer[1]. Evidence is growing that polyp removal is frequently incomplete, putting patients at risk of developing post-colonoscopy cancer[2-4]. A meta-analysis published in 2020 found that after snare resection, 15.9% of diminutive and small polyps and 20.8% of polyps 10-19 mm are removed incompletely[5]. For polyps 20 mm or larger, a metaanalysis published in 2014 demonstrated a recurrence rate of 15% after endoscopic mucosal resection(EMR)[6].
In recent years, different techniques for endoscopic resection of large colorectal polyps have evolved or been developed. Cold snare polypectomy (CSP) has been introduced and its use expanded to include the removal of large colorectal polyps[7]. Endoscopic submucosal dissection (ESD) has gained traction in Western countries and EMR has undergone technical modifications by introducing margin ablation or underwater EMR[8,9].
These developments have sparked our interest in providing an up-to-date meta-analysis of local recurrence rates (LRRs) and incomplete resection rates (IRRs) for large (≥ 10 mm) colorectal polyps, and to evaluate the impact of the novel or modified endoscopic resection techniques on LRRs.
MATERlALS AND METHODS
The analysis was conducted adhering to the Preferred Reporting Items for Systematic Reviews and Meta-analysis statement[10].
Literature search
A systematic literature search was performed within MEDLINE, EMBASE, EBM Reviews, and CINAHL databases. All articles published between January 2011 and July 2021 reporting on IRR and/or LRR for colorectal polyps 10 mm or larger removed by endoscopic resection techniques were included in the search. For specific search terms, see Supplementary Table 1. Additionally, a secondary search was performed to identify further records using article reference crosscheck, manual searching, and expert contact.
Article selection
Articles retrieved by the systematic search were collected and duplicates removed. Two researchers(Rotermund C and Taghiakbari M) assessed all articles independently and decided upon inclusion and exclusion. In cases of disagreement, a third researcher (von Renteln D) was consulted.
Inclusion criteria were full-text articles of prospectively performed clinical studies reporting on either LRR or IRR evaluated by margin assessment or margin biopsy of endoscopically removed polyps ≥ 10 mm. Even though often of larger sample size, publications with retrospective study design were excluded from the analysis, as risk for selection bias and risk for missed data is usually higher.
Exclusion criteria were retrospective study design, polyps < 10 mm, IRR evaluated by visual margin assessment, data from first follow-up that exceeded 12 mo, publications solely evaluating difficult polypectomies, publication languages other than English, articles reporting on training of a certain technique, and articles in which results from different polypectomy techniques were not clearly distinguishable.
Data extraction
Relevant data retrieved from the evaluated study included author, year of publication, country, study type, study quality, polyp size, polyp morphology, polyp histology, polyp resection method and adjunct therapy, LRR, IRR, IRR assessment method, submucosal injection rate and solution,en blocresection rate, and endoscopist number and experience level. For analyses, polyps were subdivided according to size: 10-19 mm, ≥ 20 mm (not including polyps < 20 mm), and all polyps ≥ 10 mm (including polyps ≥20 mm). Data were retrieved by one author (Rotermund C) and correct retrieval confirmed by a second author (Djinbachian R).
Outcomes
Primary outcome was LRR for polyps ≥ 10 mm. Local recurrence was defined as the presence of recurrent polyp at the resection site, detected during follow-up examination. Publications, in which the appointments for follow-up examinations exceeded 12 mo between the different patients, were excluded from the analysis. Secondary outcomes were IRR evaluated by either margin assessment or margin biopsy for polyps ≥ 10 mm, as well as factors influencing LRR and IRR, including polyp resection technique [hot snare polypectomy (HSP), CSP, hot and cold EMR, underwater EMR, ESD], adjunct therapy, margin assessment method, submucosal injection status, polyp size, polyp morphology and histology, endoscopist experience and number of endoscopists involved. IRR assessment method was defined as (1) Biopsy from the resection margin (=“margin biopsy”); (2) Histologic assessment of polyp margin (= “margin assessment”); and (3)En blocresection and histologic assessment of polyp margin (=“en blocand margin assessment”). Endoscopist experience was defined as (1) Less experienced for EMR,when a fellow was included in the study or < 2000 colonoscopies had been performed by the endoscopist; (2) Experienced for EMR, when only expert endoscopists (> 2000 colonoscopies) were involved; (3) Less experienced for ESD, when fellows for ESD (< 200 cases) were included in the study;and (4) Experts for ESD (> 200 cases).
Quality assessment and publication bias
Study quality was assessed independently by two researchers (Taghiakbari M and Rotermund C). In cases of disagreement, a third researcher (von Renteln D) was consulted. For evaluation, National Institutes of Health quality assessment forms for case series and randomized controlled trials (RCTs)were used[11]. For RCTs (maximum score: 14), a score of 11-14 was rated as good, a score of 8-10 as fair,and a score below 8 as poor quality. For prospective case series (maximum score: 9), a score of 7-9 was rated as good, a score of 4-6 as fair, and a score below 4 as poor quality. Detailed information on criteria for low and high quality are given in Supplementary Tables 2 and 3.
A sensitivity analysis was performed to determine the effects of excluding poor-quality studies and publication bias was assessed using funnel plots (Supplementary Figure 1). The graph was plotted as proportion vs. sample size instead of log oddsvs1/standard error, as this method has been shown to be more accurate in predicting risk of publication bias for meta-analyses of proportions[12].
Statistical analysis
Proportions were meta-analyzed using the metaprop command of Stata version 16 (StataCorp, College Station, TX, United States), and tests of heterogeneity were performed using theI2statistic. Either a random-effects model or a fixed-effect model was used for the analyses. Proportions were reported with their associated 95% confidence intervals (CIs) with an alpha level of < 0.05 used for statistical significance.
RESULTS
Literature search and study characteristics
Systematic literature search yielded 6922 hits and 6 additional records were identified through reference crosscheck, manual search, and expert contact (Figure 1, Supplementary Table 1). After removal of duplicates, 5010 publications remained. Of these, 4070 were excluded based on title and 672 based on abstract, so that 268 full-text records were evaluated for eligibility. Ultimately, 34 publications were included in the analysis, with 19 reporting on IRR, 13 on LRR, and 2 on both (Figure 1). All studies were prospective and 14 were RCTs.
Quality assessment and publication bias
Local recurrence rate
A total of 15 studies reported on LRR after removal of large colonic polyps ≥ 10 mm. Of these, 15 studies stated LRR obtained during follow-up examinations up to 12 mo, 7 during follow-up up to 24 mo, and 3 from follow-up after more than 24 mo (Supplementary Table 4). Definitions of LRR given in the original studies are presented in Supplementary Table 5. Mean overall LRR at up to 12 mo’ follow-up was 11.0%(95%CI, 7.1%-14.8%; 4904 polyps) (Figure 2A). Overall LRR for follow-up up to 24 mo was 14.6%(95%CI, 8.4%-20.8%; 7 studies) (Supplementary Figure 4).
Local recurrence rate up to 12 mo’ follow-up: Influence of resection method: Resection method was found to exhibit major influence on LRR of polyps ≥ 10 mm (Figure 2B, Table 1). ESD (1.7%; 95%CI,0-3.4%; 3 studies) and EMR with margin ablation (3.3%; 95%CI, 2.2%-4.5%; 2 studies) significantly reduced LRR compared with EMR in which margin ablation was not performed (15.2%; 95%CI,12.5%-18.0%; 4 studies) or only used in some cases (16.5%; 95%CI, 15.2%-17.8%; 6 studies). No prospective studies were found evaluating LRR after HSP, CSP, or cold EMR within the search period.Two studies evaluated LRR after underwater EMR; however, heterogeneity between studies was high,so that a valid analysis could not be performed.
Similarly, when only results for polyps ≥ 20 mm were evaluated, ESD and EMR with margin ablation yielded lower LRRs compared with EMR without margin ablation (Table 1). No prospective studies were found evaluating HSP, CSP, or cold EMR.
Local recurrence rate up to 12 mo’ follow-up: further influencing factors: Polyp size did not influence LRR (≥ 10 mm: 11.0%; 95%CI, 7.1%-14.8%; 15 studiesvs≥ 20 mm: 11.2%; 95%CI, 6.8%-15.6%; 12 studies)(Table 1). Similarly, expert status of the endoscopist was not found to influence LRR (Table 1); however,as only two expert studies were found, the data set was small. The data set was also insufficient for analysis of the influence of polyp morphology or histology on LRR. Only one study included pedunculated polyps (12.1% of all resected polyps); however, the reported LRR was comparable to the rate observed in other studies[13]. Most studies included sessile serrated adenoma/polyps (SSA/Ps).One study compared LRR after EMR removal of SSA/Psvsconventional adenomas and reported significantly reduced LRR for SSA/Ps[14].
Incomplete resection rate
A total of 21 studies reported on IRR after removal of large colonic polyps ≥ 10 mm, using either margin assessment or margin biopsy for evaluation (Supplementary Table 6). Mean overall IRR for all polyps ≥10 mm was 14.9% (95%CI, 11.4%-18.4%; 21 studies; 3563 polyps) (Figure 3). Twelve studies indicated IRR for polyps 10-19 mm, resulting in a mean IRR of 16.0% (95%CI, 10.4-21.7%) (Supplementary Figure 5), and 14 studies reported IRR for polyps ≥20 mm, yielding a mean IRR of 11.7% (95%CI,7.5%-15.8%; 1739 polyps) (Supplementary Figure 6).
Incomplete resection rate: Influence of resection method: Resection method was not found to significantly influence IRR of polyps 10-19 mm, comparing hot EMR (18.5%; 95%CI, 8.9%-28.1%; 8 studies), HSP (16.2%; 95%CI, 10.6%-21.7%; 2 studies), underwater EMR (25.5%; 95%CI, 18.9%-32.2%; 2 studies), and cold EMR (14.0%; 95%CI, 1.8%-26.3%; 3 studies), with studies on cold EMR exhibiting high variability (Table 2). Only two studies evaluated CSP, showing high heterogeneity, so that a valid analysis could not be performed.
Comparison of ESD and EMR for polyps ≥ 20 mm showed a lower IRR for ESD (12.5%; 95%CI,6.2%-18.8%; 9 studies) than for EMR (29.3%; 95%CI, 19.3%-39.2%; 3 studies) (Table 2). Only two studies evaluated IRR for polyps ≥ 20 mm with HSP, yielding high heterogeneity, so that a valid analysis could not be performed. No data were found reporting IRR after CSP or cold EMR for polyps ≥ 20 mm.

Table 1 Factors influencing local recurrence for polyps ≥ 10 mm at 0–12 mo’ follow-up

Figure 1 Literature search strategy.
Incomplete resection rate: Further influencing factors:For polyps sized 10-19 mm, submucosal injection status did not influence IRR. Mean IRR after resection with submucosal injection was 20.0%(95%CI, 11.9%-28.0%; 10 studies) compared with 14.4% (95%CI, 5.4%-23.3%; 6 studies) after resection without submucosal injection (Table 2). For polyps ≥20 mm, IRR was lower after resection with prior submucosal injection (Table 2). Mean IRR after submucosal injection was 12.6% (95%CI 7.7-17.6; 13 studies), compared to 32.4% (95%CI, 0-76.3%; 3 studies) after resection without injection.
由此揭示了个体发展与全体发展的互相促进、互为因果的关系,即发展不仅仅限于满足全体人民的物质文化需要,同样更要满足广大普通个体的生理与心理需求,才能达到社会的和谐。同样,在这段对科学发展观的经典论述中也寻不到社会或国家的影子。
The solution used for submucosal injection was not found to influence IRR, yielding comparable results for saline solution (15.8%, 95%CI, 7.1%-24.8%; 6 studies) and hyaluronic acid (16.3%, 95%CI,8.5%-24.1%; 8 studies) (Table 2).
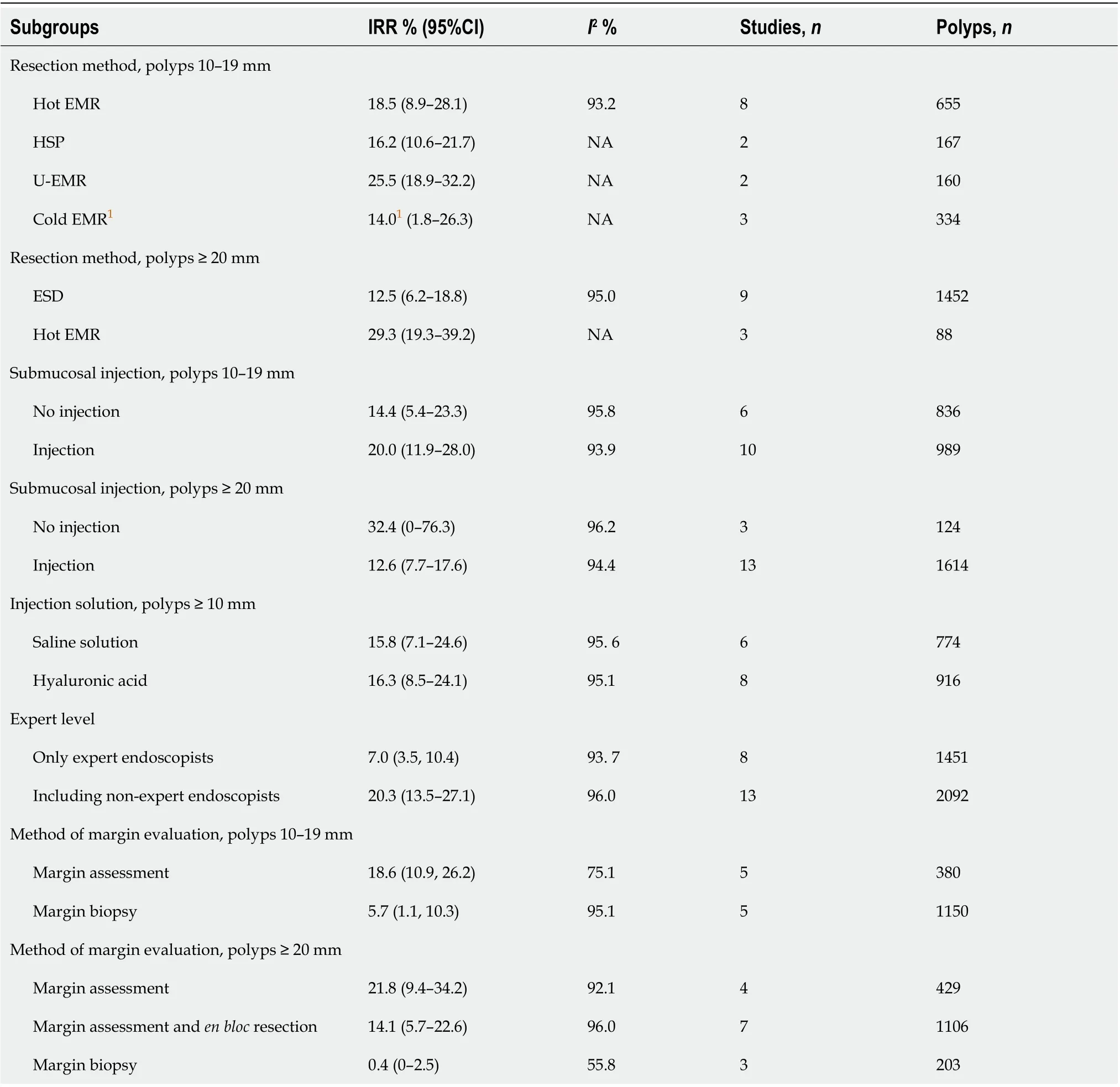
Table 2 Factors influencing incomplete resection
There was a strong trend toward lower IRR when considering endoscopist experience (Table 2,Supplementary Figure 7). The mean IRR was 7.0% (95%Cl, 3.5%-10.4%; 8 studies) when only expert endoscopists were involved in the study, and 20.3% (95%Cl, 13.5%-27.1%; 13 studies) when non-experts were included.
Insufficient data were available for analysis of the influence of polyp morphology or histology on IRR. Three studies included around 50% or more pedunculated polyps; two analyzed hot EMR[15,16] ,and the third analyzed hot and cold EMR and CSP[17]. Three further studies included smaller numbers of pedunculated polyps, using cold EMR[18], ESD[19], and underwater EMR[20]. Most studies included 10% or less SSA/Ps, while two studies investigating CSP and cold EMR evaluated results from SSA/Ps only[21,22]. The latter two studies reported exceptionally low IRR of less than 1.5%.
DlSCUSSlON

Figure 2 Local recurrence rate at < 12 mo’ follow-up. A: For polyps ≥ 10 mm; B: For polyps ≥ 10 mm, stratified by resection method.
This meta-analysis confirms the high risk for recurrence after standard EMR resection of large colonic polyps. When standard EMR without routine margin ablation is used, we found a 12-month recurrence rate of 15.2%. This is comparable to the results found in the two available meta-analyses published in 2014 and 2021, which reported recurrence rates of 15%[6] and 10%[23], respectively. However, since then, many new or modified endoscopic removal techniques have been developed. These novel developments include cold EMR, hot snare with margin ablation, and an increasing body of literature on ESD for colorectal polyps coming from Asian, European and North American centers. We found that two of these modalities resulted in significantly lower LRRs compared with standard EMR. ESD was associated with an LRR of only 1.7%, and the LRR after EMR with routine ablation of the complete margin was 3.3%. However, ESD requires advanced endoscopy skills, adequate training, and the technique is associated with an increased risk for complications[24-26]. Furthermore, significant differences in safety and efficacy of ESD have been shown between Asian and non-Asian countries[27],so that EMR has remained the standard for large polyp resection in Western countries to date.
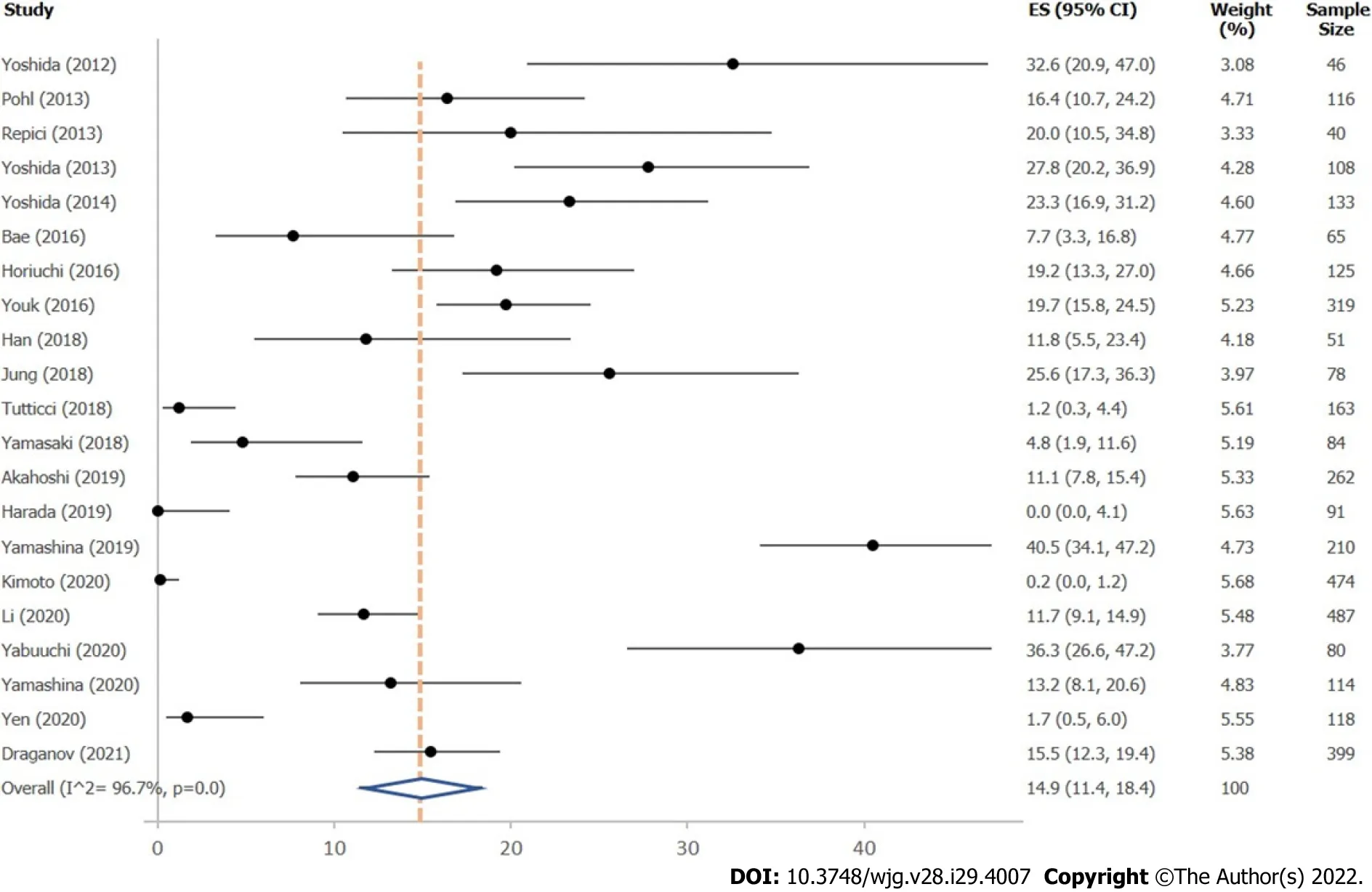
Figure 3 lncomplete resection rate for polyps ≥ 10 mm, independent of resection method.
The other modality that shows significantly reduced recurrence rates is the combination of hot EMR with routine margin ablation[9,28]. Thus, ESD or EMR with routine margin ablation currently seem to be the best approaches for endoscopic removal of large colorectal polyps in order to avoid recurrence.We found that systematic margin ablation after EMR can reduce the LRR to rates similar to those of ESD. These results originate from two recent Australian prospective studies, in which snare tip soft coagulation (STSC) was routinely performed after EMR[9,28]. As these studies included only polyps ≥20 mm further studies evaluating the effect of margin ablation on polyps sized 10-19 mm may be of additional value. The positive effect of margin ablation has also been shown in a retrospective US study,evaluating systematic application of argon plasma coagulation (APC) after EMR in 246 patients[29]. The authors found an LRR of 5% at < 12 mo FU, which is comparable to the rates found by Klein (5%) [9]and Sidhu (3%)[28]. However, the results for using APC margin ablation still need to be confirmed by prospective studies. A recently completed prospective, multicenter study evaluating resection of large colonic lesions ≥ 20 mm in 76 patients using EMR and hybrid APC for margin and base ablation found a LRR of 2.2%[30]. This indicates that APC ablation can reduce local recurrence comparable to ESD and EMR with STSC.
Importantly, margin ablation should be performed systematically and completely, as visual margin assessment may underestimate incomplete resection[4]. This is confirmed by our analysis, which showed that studies using unsystematic or incomplete margin ablation were not able to reduce the LRR[9,14,31].
Notably, even though use of cold snare resection techniques for large colonic polyps is increasingly reported, at present no prospective studies have been published reporting LRR for CSP or cold EMR for large colorectal polyps. Furthermore, recent retrospective studies have indicated that these techniques might potentially increase the risk for local recurrence. In the largest retrospective series published to date, Sureshet al[32] reported an LRR of 34.8% after cold EMR. Therefore, caution is warranted for routine use of cold EMR outside of clinical studies until data from ongoing RCTs comparing hot with cold EMR become available.
For polyps 10-19 mm, follow-up examination is often performed years after the index colonoscopy.Therefore, data on LRR for 10-19 mm colorectal polyps are sparse, and we used IRR to estimate the risk of local recurrence for this subgroup. In our analysis, overall IRR for polyps sized 10-19 mm was 16.0%.This rate was similar to the IRR found in a previous meta-analysis (20.8%)[5] and in one of the landmark studies on IRR (CARE study)[4]. The CARE study reported that even though endoscopists rated resection as complete by visual assessment, 10.1% of cases showed residual tissue on margin biopsy.Compared with the previous meta-analysis, our analysis included more data, especially regarding cold snare resection techniques[5]. However, adding the recently published data on cold snare resection did not significantly alter overall IRR of polyps 10-19 mm. Furthermore, IRR of EMR, cold EMR, HSP, and underwater EMR were similar[17,18,21]. Only two prospective studies evaluated IRR for large colonic polyps after CSP resection[17,21]. These studies showed high variability in IRR, and while one study found rates comparable to those obtained with other techniques[17], rates reported in the second were extremely low[21]. This is likely based on the fact that in this study only expert endoscopists were involved and only SSA/Ps were removed by wide-field style cold snare resection. A previous metaanalysis has already demonstrated that expert endoscopists achieve lower IRRs[5], and this was confirmed in our analysis, with an IRR of 7.0% for expert endoscopists and 20.3% for those studies in which less experienced endoscopists were included. Furthermore, the exclusive inclusion of SSA/Ps introduced a further bias into the study, as removal of SSA/Ps generally yields better results[14]. This renders the generalizability of CSP to general clinical practice difficult, and more prospective studies are needed to establish IRR, and especially LRR risk, after CPS and cold EMR removal of large colorectal polyps including all pathology types.
For polyps ≥ 20 mm, the mean IRR was 11.7% in this analysis. Interestingly, this rate is lower than the results obtained for polyps sized 10-19 mm (16.0%). This effect was based on the good results obtained with ESD, and is most likely also associated with the fact that 10-19 mm polyps are usually resected in general endoscopic practice, whereas polyps ≥ 20 mm are often referred for expert resection.
Recent guidelines recommend HSP, EMR [European Society of Gastrointestinal Endoscopy, American Gastroenterological Association (AGA)][33,34] and CSP (AGA)[34] for resection of 10-19 mm polyps.Our data show that EMR with margin ablation is an important new development that warrants further study. For lesions ≥ 20 mm, guidelines recommend ESD in specific cases, and the need for a skilled endoscopist to perform the procedure is highlighted[25,26,35]. The importance of endoscopist skill level is also supported by our data. Furthermore, our data suggest that EMR with systematic and complete margin ablation may be an appropriate alternative to ESD, especially considering the low complication rates reported in the available studies[9,28,29].
However, safety profiles should also be taken into account when evaluating different polypectomy techniques. Known complications occurring during and after polypectomy are immediate and delayed bleeding as well as perforation and post-coagulation syndrome[33,34]. A meta-analysis from 2016 evaluating endoscopic resection of polyps ≥ 20 mm found perforation occurring in 1.5% and bleeding in 6.5% of polyps. Mortality was indicated as 0.08%[36]. Yet, an up-to-date analysis comparing safety profiles of CSP, HSP, EMR with and without margin ablation, underwater EMR, and ESD still has to be performed.
Our analysis has several strengths, including the robustness of the literature search with a large number of publications screened (6928 publications). Of these, 34 prospective studies with a total of 10268 polyp resections were included. As only prospective data were evaluated, we were able to perform a high-quality analysis, as retrospective studies reporting on LRR and IRR are unsystematic in the ascertainment of the main outcomes, thus having a high likelihood of bias. Furthermore, the retrieval of granular data allowed us to perform multiple analyses.
The main limitation of the study is that by exclusion of retrospective studies, the data set was reduced. Furthermore, publications were excluded in which IRR was determined by visual assessment or in which appointments for follow-up examinations for LRR assessment exceeded 12 mo. While this reduced the amount of studies included into the analysis, it ensured a better overview of the highquality data available in the literature. Additionally, it shows that for some techniques data of sufficient quality is sparse and that there is a need for further studies. Second, expert endoscopist status was difficult to determine, as there is no published consensus definition, and some studies do not clarify the expertise of the involved endoscopists. However, expert and non-expert status were systematically assessed and discussed for this meta-analysis. Third, as assessment for IRR is not standardized, different methods, including margin assessment and margin biopsy, are used for its estimation. However, margin assessment is likely to overestimate IRR, as lesions resected in piecemeal fashion may be resected completely, but will appear with positive resection margins. Margin biopsy, on the other hand, is likely to underestimate IRR, as only sample parts of the margins are examined[37]. Therefore, true IRR will be located somewhere in between the values found with margin biopsy and margin assessment. Another limitation is the elevated heterogeneity in some reported outcomes. For LRR, most of the observed heterogeneity was due to combining different resection techniques into the same analysis. When stratifying for resection technique and use of margin ablation, we found very low heterogeneity in the reported outcomes. For IRR, the differing use of wide field resection before biopsies and the number of margin biopsies taken could explain some of the heterogeneity reported.
CONCLUSlON
In conclusion, we found that local recurrence after resection of large colonic polyps occurs frequently when standard EMR is used. Local polyp recurrence can be reduced by performing ESD or EMR with routine and complete margin ablation. Other techniques, such as CSP, cold EMR, and underwater EMR require further evaluation in prospective studies before their routine implementation in clinical practice can be recommended.
ARTlCLE HlGHLlGHTS

FOOTNOTES
Author contributions:von Renteln D designed the research study; von Renteln D, Rotermund C, Djinbachian R,Taghiakbari M, Enderle MD, and Eickhoff A performed the research; von Renteln D, Rotermund C, Djinbachian R,and Taghiakbari M analyzed the data; and von Renteln D, Rotermund C, and Djinbachian R wrote the manuscript;and All authors have read and approve the final manuscript.
Conflict-of-interest statement:All authors report no relevant conflicts of interest for this article.
PRlSMA 2009 Checklist statement:The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Canada
ORClD number:Daniel von Renteln 0000-0002-6125-0068.
S-Editor:Ma YJ
L-Editor:A
P-Editor:Ma YJ
 World Journal of Gastroenterology2022年29期
World Journal of Gastroenterology2022年29期
- World Journal of Gastroenterology的其它文章
- Mechanistic and functional extrapolation of SET and MYND domain-containing protein 2 to pancreatic cancer
- Clinical challenge for gastroenterologists-Gastrointestinal manifestations of systemic mastocytosis: A comprehensive review
- Structural changes of proteins in liver cirrhosis and consequential changes in their function
- Epidemiologic and socioeconomic factors impacting hepatitis B virus and related hepatocellular carcinoma
- Enhanced endoscopic ultrasound imaging for pancreatic lesions: The road to artificial intelligence
- Qingyi decoction attenuates intestinal epithelial cell injury via the calcineurin/nuclear factor of activated T-cells pathway
