Which psychosocial factors are associated with return to sport following concussion?A systematic review
Jcqueline vn Ierssel,Kleigh Ferdinnd Pennock,Mrgret Smpson,Roger Zemek,c,Jeffrey G.Cron
a Children’s Hospital of Eastern Ontario Research Institute,Ottawa,ON K1H 8L1,Canada
b Faculty of Kinesiology and Physical Education,University of Toronto,Toronto,ON M5S 2W6,Canada
c Department of Pediatrics,Faculty of Medicine,University of Ottawa,Ottawa,ON K1H 8M5,Canada
d Faculty of Medicine,University of Montreal,Montreal,QC H3T 1J4,Canada
e Center for Interdisciplinary Research in Rehabilitation,Montreal,QC H3S 1M9,Canada
Abstract Background:Psychosocial factors predict recurrent injury and return to preinjury level of performance following orthopedic injury but are poorly understood following concussion.Current management protocols prioritize physical measures of recovery.Therefore,the objective of this study was to describe the psychosocial factors associated with return to sport(RTS)and how they are measured in athletes who sustained a concussion.Methods:MEDLINE,Embase,APA PsycINFO,CINAHL,and SPORTDiscus were searched through February 2,2021.Eligible studies included original peer-reviewed publications describing psychosocial factors associated with RTS following a diagnosed concussion. The primary outcome was scales or measures employed and/or key thematic concepts.Results:Of the 3615 studies identified,10 quantitative cohort studies(Oxford Centre for Evidence-Based Medicine Level-3)representing 2032 athletes(85%male;high-school and collegiate collision/contact athletes)and 4 qualitative studies representing 66 athletes(74%male;70%American football;aged 9-28 years)were included.We identified 3 overarching themes and 10 outcome measures related to psychosocial factors associated with RTS following concussion:(a)fear(e.g,of recurrent concussion,of RTS,of losing playing status);(b)emotional factors(e.g,depression,anxiety,perceived stress,mental health, disturbance mood);and(c)contextual factors(e.g,social support,pressure,sense of identity).Conclusion:Although current medical clearance decisions prioritize physical measures of recovery,evidence suggests diverse psychosocial factors influence RTS following concussion.It remains unclear which psychosocial factors contribute to a successful RTS,including the influence of sex/gender and age.Future studies should evaluate the association of psychological readiness with physical measures of recovery at medical clearance,preinjury level of performance,and risk of recurrent concussion to support RTS clinical decision-making.
Keywords: Concussion;Recovery;Rehabilitation;Sport psychology;Sporting injuries
1. Introduction
Return to sport (RTS) is considered the pinnacle of clinical recovery following concussion in athletes.1International consensus guidelines currently rely on the assessment of physical readiness to determine when an athlete is medically cleared to RTS following concussion, based on the resolution of postconcussion symptoms and clinically normal measures of balance and cognitive function.2This approach tacitly assumes that physical and psychosocial recovery occur in parallel and that physical recovery is sufficient to mitigate risk of recurrent concussion.
However,growing evidence suggests that psychosocial factors are an important predictor of recurrent injury and determinant of return to preinjury level of performance among athletes with orthopedic injuries.3-9Athletes with a previous history of concussion are nearly 4 times more likely to sustain a recurrent concussion than those without,10yet clinicians have received little guidance on how to measure or mitigate the impact of psychosocial factors on RTS medical clearance following a concussion despite the known existence of psychosocial sequelae.11
Psychosocial factors associated with RTS include related yet distinct concepts such as fear of recurrent injury,4,6-8,12-15anxiety,7,16self-efficacy,7,8loss of confidence,6-8,17hesitancy,6motivation,8,17,18coping strategies,6,18social support,7,8,16,18and performance expectations.7,16-18Injuryrelated biases in this area limit generalizability,19and a concussion-specific understanding of psychosocial factors associated with RTS is critical due to key differences in recovery from concussion compared with orthopedic injuries including the fact that:(a)objective diagnostic and recovery biomarkers are lacking for concussion; (b) symptoms are multidimensional with wide-ranging functional impacts;(c)prognosis and recovery trajectories are unclear; (d) treatment options are poorly understood; (e) few concussion studies use clearly defined RTS criteria despite recommendations for a multimodal evaluation;2,20and(f)RTS before recovery is complete is a risk factor for recurrent concussion with possible serious consequences,including death.10,21
The first step in standardizing clinical recommendations for medical clearance criteria is to understand the impact of psychosocial factors on RTS following concussion. Integrating quantitative and qualitative research provides a deeper understanding of the lived experiences underlying statistical associations that can help inform clinical decision-making.19A previous systematic review9identified 18 different outcome measures used to assess 15 different psychological factors associated with successful RTS following orthopedic injury,including fear, confidence, and motivation. The relevance of these findings to concussion requires further study since (a)qualitative studies were not included; (b) studies did not include athletes with concussion; (c) the search strategy did not include studies published after March 2012,the year international concussion consensus guidelines included confidence as a stated goal within the graded RTS strategy;and(d)analyses implemented a predetermined framework (self-determination theory) that may have shaped conclusions. The current review builds upon important previous research and reflects an update to a growing body of literature with a streamlined focus on RTS following concussion.
The objective of this systematic review was to describe the psychosocial factors associated with RTS and how they are measured in athletes who have sustained a concussion. These findings may inform future research and RTS decision-making following concussion beyond currently used physical measures.
2. Methods
A priori,we registered a scoping review designed to synthesize concepts and themes across all sports and injuries into an operational definition of psychological readiness(Registration number:osf.io/6xq3a).For this systematic review,we included concussion-specific studies that were identified in the larger scoping review search strategy to answer our specific research question. Results are reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses(PRISMA) guidelines to increase methodological clarity and adoption of research findings.22
2.1. Study identification:Data sources and search strategy
The following research question, developed in collaboration with clinical and research partners, guided this review:Which psychosocial factors are associated with RTS following concussion?We defined RTS according to the combined definitions of the 2016 Consensus Statement on Return to Sport and the 5th Consensus Statement on Concussion in Sport as the return to an athlete’s predefined sport following resolution of symptoms at rest and with a graduated, stepwise exercise strategy.2,23Thus, in the context of this review, RTS refers to the phase of recovery following medical clearance when the athlete is considered clinically recovered and able to resume unrestricted at-risk activity.
We conducted a search of 5 electronic databases: MEDLINE, Embase, American Psychological Association (APA)PsycINFO, CINAHL, and SPORTDiscus. The search included studies published in English or French in peer-reviewed journals from database inception until February 2, 2021. A research librarian who is experienced in systematic reviews (MS)designed and conducted the search strategy based on RTS recommendations following concussion,2as well as previously published systematic reviews on concussion,10psychological readiness to RTS following sports injury,9and psychosocial factors associated with outcomes of sports injury rehabilitation19(Supplementary Table 1).We also manually searched reference lists of included studies and relevant systematic reviews to ensure all relevant studies were captured and included into the set for screening. We used a combination of database-specific search terms and keywords and uploaded all citations into the Web-based citation manager insightScope.24
2.2. Study selection criteria
We included studies that met the following criteria: (a)quantitative or qualitative studies that examined psychosocial factors associated with RTS as a primary or secondary outcome;(b)at least 1 athlete in the study sample must have sustained a diagnosed concussion (any mechanism of injury); (c)data were reported by an athlete,coach,or healthcare provider;and(d)the athlete had to have returned to their preinjury level of sport. We placed no restrictions on age, sex/gender, or sporting level of participants. We excluded: (a) studies that only reported non-concussion-related injuries (e.g., moderate or severe traumatic brain injury, orthopedic injury, general health conditions such as cardiac pathology); (b) systematic reviews,position statements,commentaries,editorials,opinion pieces,letters to the editor, abstracts, conference proceedings;and (c) studies that examined outcomes other than RTS, such as return to cognitive activity(e.g.,school)or functional activity(e.g.,activities of daily living).
We appraised records against pre-established eligibility criteria using a 3-step approach. Two reviewers (JvI and KFP)independently screened titles and abstracts of identified citations to decide whether the study should be retained for further consideration or rejected, or whether the relevance was unclear. Two reviewers (JvI and JGC) then assessed the full text of retained studies for eligibility. If no abstract was available or eligibility was not clear from the abstract, we reviewed the full text.When consensus could not be obtained,a third reviewer(KFP)independently reviewed the full text to resolve the disagreement. We calculated inter-rater reliability(ICC) for abstract/title selection using the kappa statistic with 95% confidence interval (95%CI) for level of agreement between the 2 reviewers(JvI and KFP).
2.3. Level of evidence
Two reviewers (JvI and JGC) independently assessed level of evidence using the Oxford Centre for Evidence-Based Medicine criteria to enhance interpretation of findings.25Discrepancies were resolved by discussion between Jvl, KFP, and JGC until consensus was reached.
2.4. Quality assessment
We used the Mixed Methods Appraisal Tool (MMAT)26to assess the methodological quality and potential for bias within the included studies. The MMAT applies 5 specific sets of criteria according to methodological design: (a)qualitative; (b) quantitative randomized controlled trials;(c) quantitative non-randomized; (d) quantitative descriptive; and (e) mixed methods. Each study was judged within the corresponding methodological domain and presented as a percentage-based quality score. ICC of the MMAT quality score is high (0.72-0.94).26
2.5. Data extraction
Two reviewers (JvI and JGC) independently extracted the following information from retained studies using a standardized data collection form developed for this review: (a) study characteristics such as study authorship, year of publication,study design (e.g., cohort, cross-sectional), country, data source (e.g., athlete, coach, or healthcare provider), sample size,definition of construct(e.g.,fear of recurrent injury,confidence),and outcome measure(s)used;(b)participant characteristics such as age, sex and/or gender, previous history of concussion, pre-existing psychiatric history (e.g., depression,anxiety), sport played, and level of performance; (c) concussion-specific information such as definition used(e.g.,Concussion in Sport Group, physician diagnosis) and time of assessment relative to date of concussion (e.g., at medical clearance, number of weeks post-concussion); (d) mean (SD)and median (interquartile range) quantitative findings where appropriate; and (e) narrative themes identified in qualitative studies. We compared data collection forms and resolved discrepancies by discussion and mutual agreement.
2.6. Data synthesis
We used thematic analysis to synthesize key concepts based on each study’s definition of factors being assessed, the purpose of each outcome measure, and narrative themes expressed.27We inductively classified and organized those key concepts into overarching themes with the associated outcome measures. We held team meetings to discuss identified themes and agree on interpretation until consensus was reached.Due to the heterogeneity of study designs,differences in psychosocial constructs, outcome measures used, and unreported medical clearance decision-making criteria, a metaanalysis was not appropriate, thus we presented the key findings through a narrative summary.
3. Results
3.1. Literature search(study identification)
The search identified a total of 3615 records(Fig.1).After duplicates were removed, 1995 unique records were assessed based on title and abstract and, of these, 295 full texts were assessed for eligibility. Fourteen studies28-41met our inclusion criteria. There was substantial agreement between reviewers for abstract/title selection(κ=0.70).
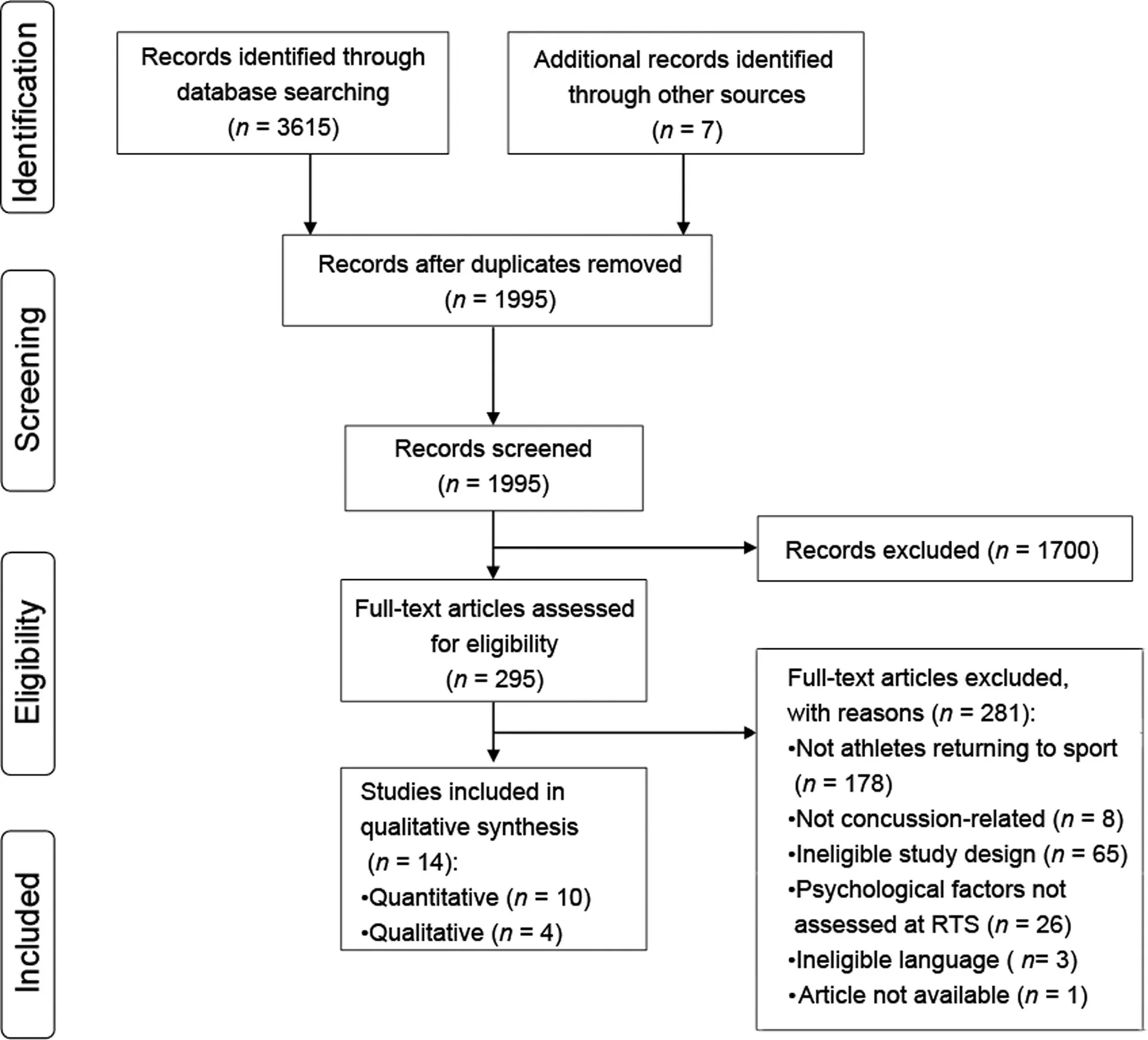
Fig. 1. PRISMA flow diagram of literature search and selection process. PRISMA=Preferred Reporting Items for Systematic Reviews and Meta-Analyses;RTS=return to sport.
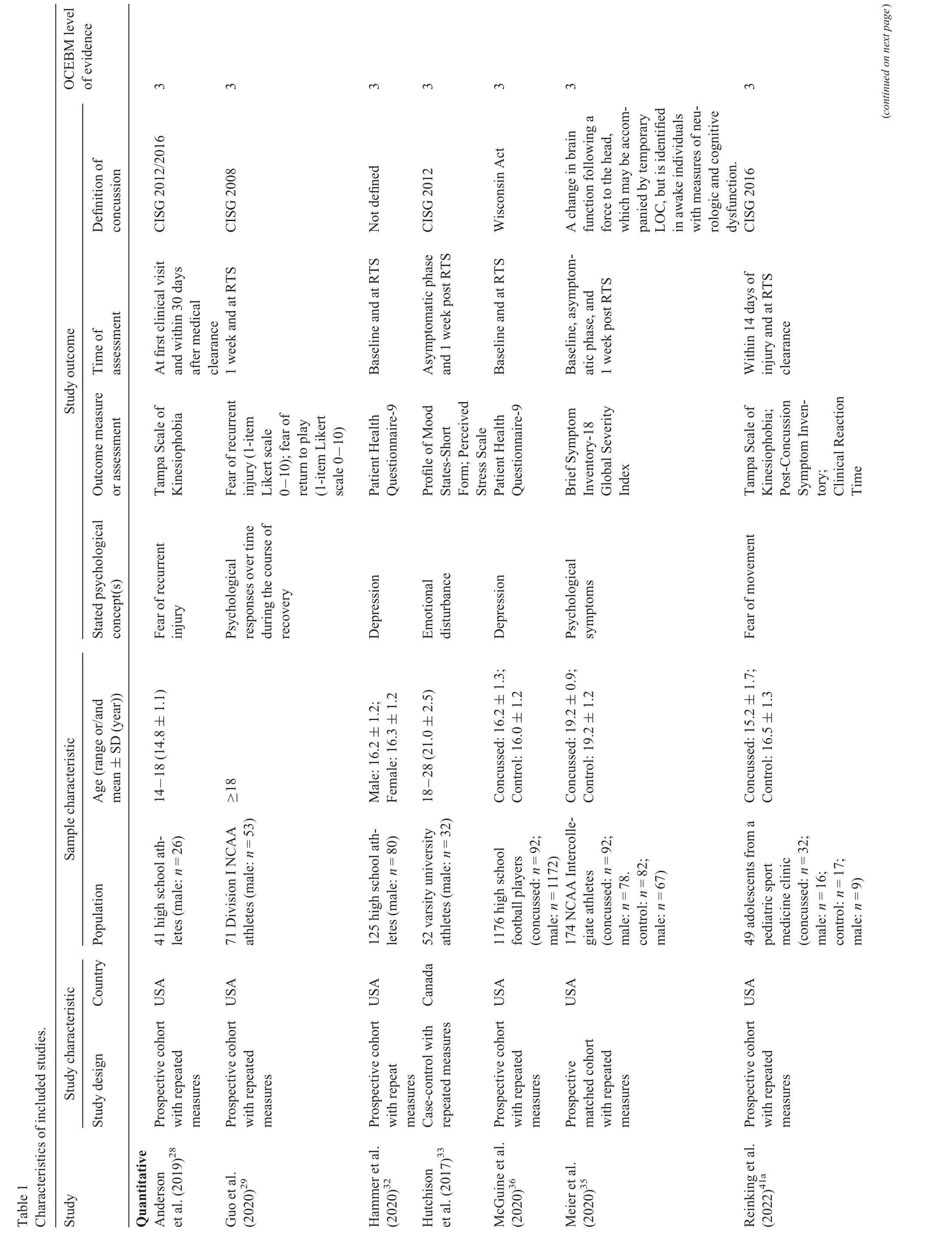
3.2. Study characteristics
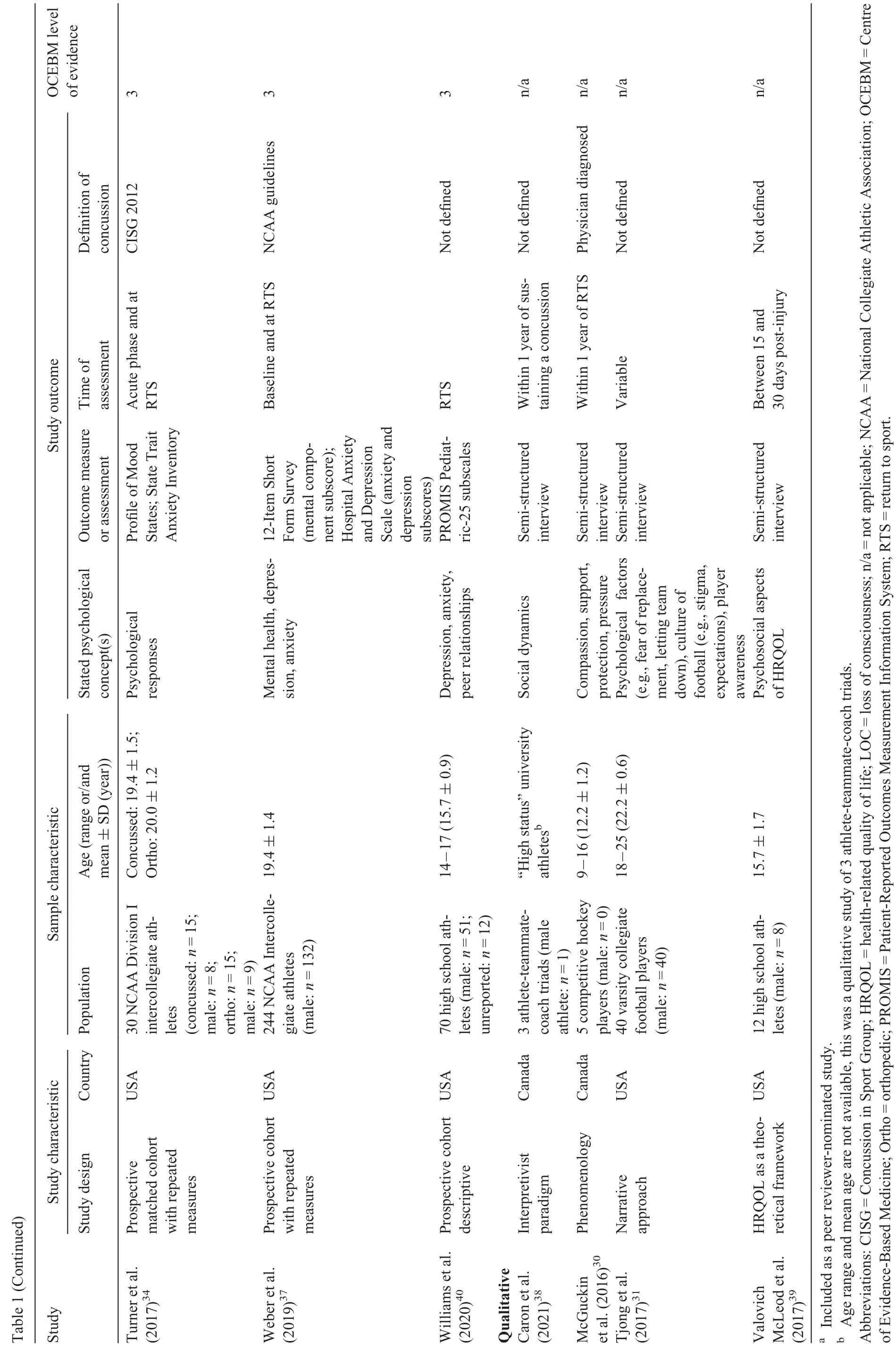
All studies were published between 2016 and 2021, inclusively,and none were included in previously published reviews in this field.9,42,43Of the 14 included studies, 10 (71%) were quantitative cohort studies,28,29,32-37,40,41involving 1 case-control33(n=52)and 9 studies28,29,32,34-37,40,41(n=1980)prospective cohort studies with repeated measures; 4 (29%) were qualitative studies30,31,38,39consisting of mixed epistemological and methodological approaches(n=66)(Table 1).Eight out of the 10 outcome measures used had not been identified in 3 previous systematic reviews in this area.9,19,43No studies examined the association of psychosocial factors with physical measures of recovery commonly used to determine medical clearance or risk of recurrent concussion.
Data represent 2098 participants (male, n=1782; 85%)from across the United States and Canada. Seven studies focused on adolescents28,30,32,36,39-41(age range:9-18 years),and 7 studies focused on collegiate athletes29,31,33-35,37,38(age range:18-28 years),all of whom had sustained a sport-related concussion. In all studies, the data extracted were reported by the athletes themselves.Athletes were recruited from a variety of sports, primarily American football (70%). In the quantitative studies (2032 athletes; 85% male; high-school and collegiate collision/contact athletes), psychosocial factors were assessed at baseline or shortly after injury and again around RTS; in the qualitative studies (66 athletes; 74% male; 70%American football; aged 9-28 years), they were assessed at varying time points within the first year following injury.Eight studies28-30,33-35,40,41defined concussion according to current international consensus criteria2,44or a physician diagnosis.
3.3. Level of evidence and quality assessment
The level of evidence for all quantitative studies was moderate (Oxford Centre of Evidence-Based Medicine level-3).Most studies were of high quality;the median score for quantitative studies28,29was 80%(range:40%-100%),and all qualitative studies30,31scored 100%(Table 2).
3.4. Overarching themes and outcome measures
There were 3 overarching themes: (a) fear; (b) emotional factors; and (c) contextual factors influencing RTS decisions(Table 3). Psychosocial factors related to RTS were assessed using 10 different standardized outcome measures (in their entirety or with one or more subscales), 2 Likert scale questions,and semi-structured interviews.
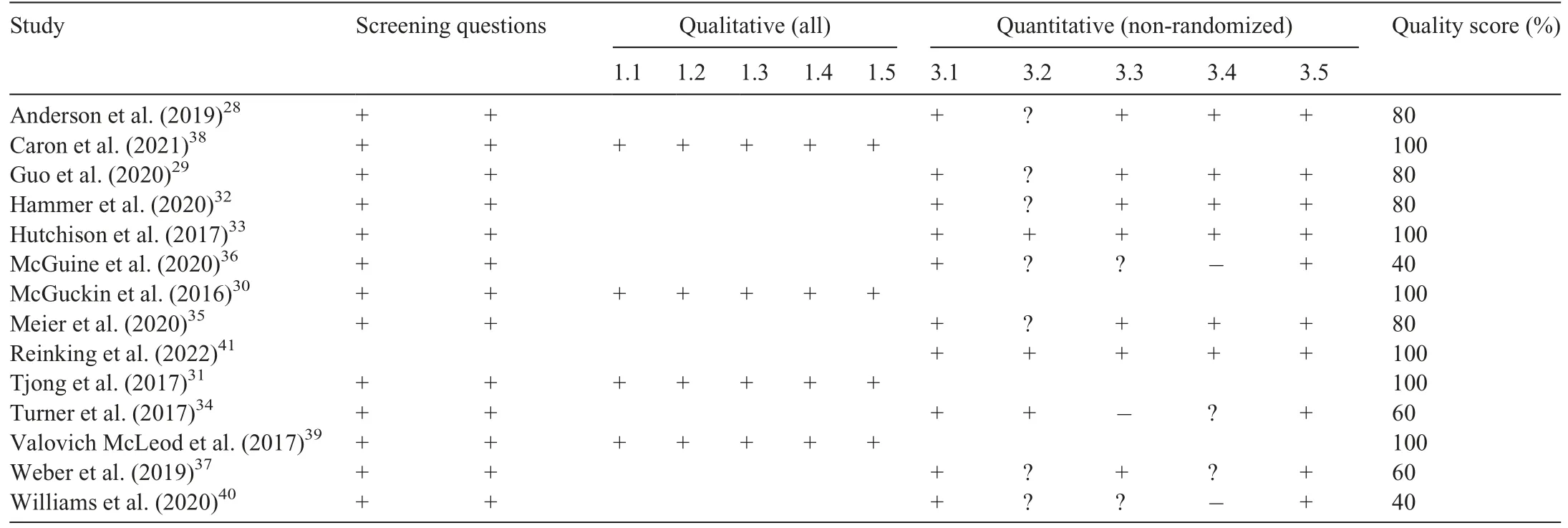
Table 2 Study quality assessment using the Mixed Methods Appraisal Tool(MMAT)Version 2018.
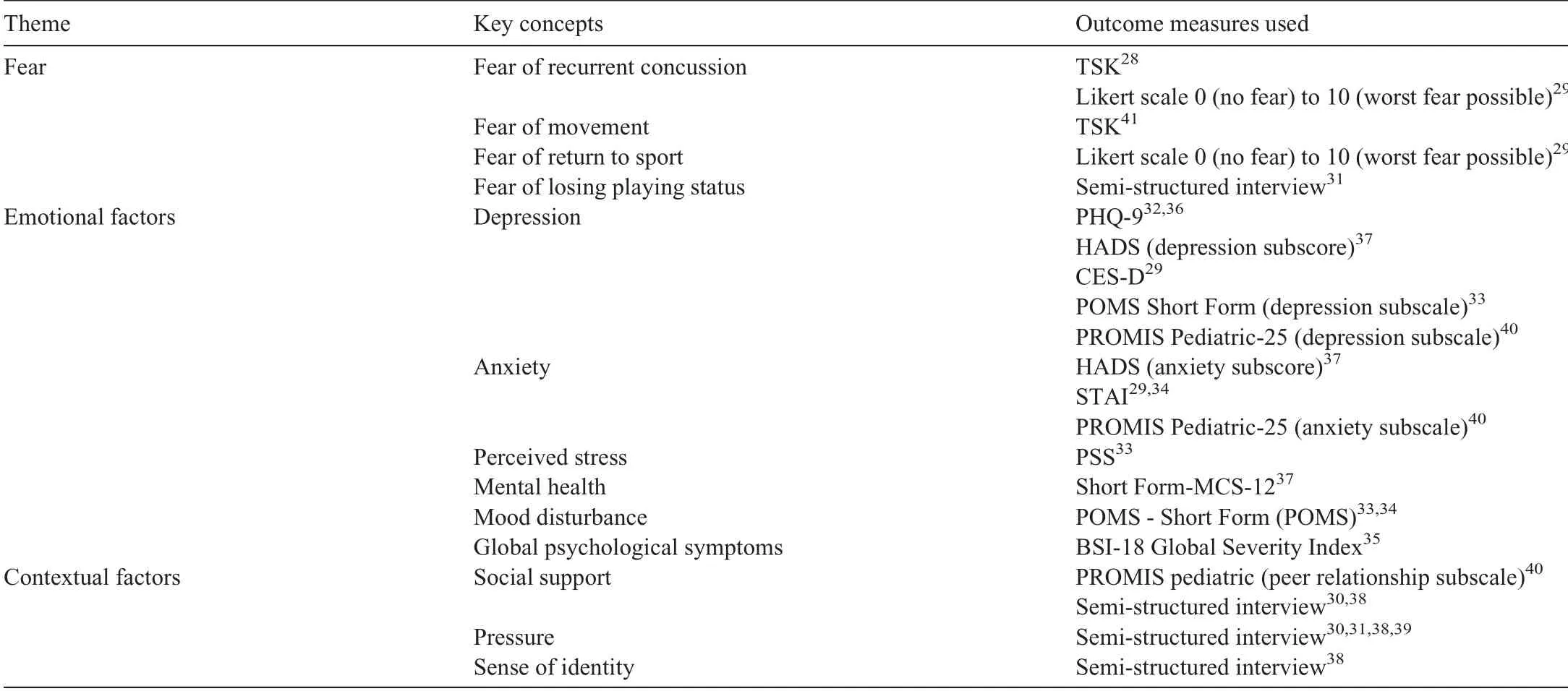
Table 3 Themes,key concepts,and outcome measures used.
3.5. Fear
Five studies (36%) examined the association of fear with RTS, specifically fear of recurrent concussion, fear of movement, fear of RTS, and fear of losing playing status, with diverse findings.28,29,31,38,41Compared with a control group,no significant difference in fear of movement has been reported amongst adolescents with a concussion(Tampa Scale of Kinesiophobia: 33.3 ± 6.5 vs. 30.8 ± 7.4; p=0.23;d=0.36).41Fear of movement was moderately correlated with clinical reaction time in those concussed adolescents at RTS(r=0.50; p=0.01).41Preliminary evidence suggests fear of recurrent concussion, however, is a concern among university athletes38as well as in 10%of high school athletes at medical clearance for RTS,with higher levels of fear in those without a previous concussion history (Tampa Scale of Kinesiophobia:t39=-2.80;p=0.008).28High school athletes with high levels of fear were more likely to exhibit vestibular/ocular symptoms above clinical cutoffs at RTS (OR=5.19; 95%CI:1.33-20.28),but showed no difference in neurocognitive outcomes or recovery time compared with low fear groups.28Compared with collegiate athletes with an orthopedic injury,concussed athletes demonstrated significantly lower Likert scores for both fear of recurrent concussion/injury(B=-1.11;p=0.0152) and fear of returning to play (B=-0.94;p=0.0278) at the time of RTS.29No effect measures were reported for either fear of recurrent concussion or fear of RTS,thus we could not quantify their association with measures of physical recovery in determining medical clearance to RTS.Fear of losing playing status motivated varsity football players to intentionally underreport concussion symptoms and purposefully score low on baseline testing in order to obtain medical clearance and avoid jeopardizing their spot on the team.31
3.6. Emotional factors
?
?
Six studies examined the association between depression and RTS following concussion.29,32,33,36,37,40A history of previous concussion was associated with higher depression scores in intercollegiate athletes (Hospital Anxiety and Depression Scale: F(1,179)=5.43; p=0.021)37but not in high school athletes at RTS (Patient-Reported Outcomes Measurement Information System (PROMIS): p >0.05).40Concussed athletes had higher levels of depression compared with athletes with orthopedic injuries (Center for Epidemiological Studies-Depression: p=0.0264)29but lower depression scores than uninjured athletes following RTS (Profile of Mood States:False Discovery Rate <0.05).33Five studies suggested depression improved throughout recovery,with lower(better)scores at RTS than at baseline32,33,36,37,40and no significant differences between sexes (Patient Health Questionnaire-9:p=1.00).32Changes in depression were not associated with time to RTS(PROMIS:p >0.05).40
3.6.2. Anxiety and perceived stress
Five studies examining anxiety and stress at RTS following concussion had conflicting results.29,33,34,37,40Two studies reported no association between history of previous concussion and anxiety at RTS.37,40Anxiety did not differ between concussed athletes and those with orthopedic injuries at RTS.29,34Anxiety improved throughout recovery in concussed athletes,with lower levels at RTS than at baseline,40although changes in anxiety were not associated with time to RTS.40In contrast,Turner et al.34reported no significant change in anxiety over time (State-Trait Anxiety Inventory: F(2,86)=2.14;p=0.099; η2=0.054), with more than half of athletes (60%)reaching clinical levels of anxiety at RTS. There were no differences in perceived stress between concussed and uninjured university athletes at RTS.33
3.6.3. Mental health and mood
Three studies explicitly examined mental health or mood disturbance at RTS following concussion.33,34,37Previous concussion history had no significant effect on mental health in concussed athletes at RTS (Mental Health Component Scale-12: F(1,188)=3.00; p=0.085).37Concussed athletes demonstrated lower total mood disturbances compared with both uninjured controls33and athletes with orthopedic injuries34as well as similar global psychological symptoms (Brief Symptom Inventory-18:F(1,165)=1.70;p=0.19)35as uninjured controls at RTS. Two studies showed total mood disturbance(negative mood subscale score minus positive mood subscale score) improved significantly over time, with concussed athletes reporting lower (better) scores on the Profile of Mood States at RTS than at baseline.33,34In contrast, Weber et al.37found no significant differences in mental health scores between baseline and RTS concussion(Mental Health Component Scale-12:F(4,450)=2.23;p=0.065).
3.7. Contextual factors
3.7.1. Social support
Three studies examined the influence of social support and peer relationships on RTS following concussion.30,38,40In 1 study, peer relationships significantly improved between 3 days post-injury and RTS but were not associated with time to RTS or previous concussion history(PROMIS:p >0.05).40In a qualitative study, female youth hockey players perceived positive social support from coaches, teammates, and parents as concern for their well-being.30Caron et al.38described qualitative evidence of differences in perceived social support between what an athlete wanted and what teammates felt was needed.
At one moment it was so pitch dark that she could not see a single object, but a flash of lightning revealed the whole scene; she could see every one who had been on board excepting the prince; when the ship parted, she had seen him sink into the deep waves, and she was glad, for she thought he would now be with her; and then she remembered that human beings could not live in the water, so that when he got down to her father’s palace he would be quite dead
3.7.2. Pressure
Four qualitative studies found athletes experienced both external and internal pressure to RTS before they had fully recovered.30,31,38,39Athletes’ perceptions of the sporting culture of collegiate football created expectations for athletes to be tough and promoted non-reporting of symptoms and premature RTS following concussion.31Female athletes in contact sports also felt subtle pressure from teammates, coaches, and parents to RTS as quickly as possible to minimize the adverse impact on the team.30,38Medical professionals were seen as informative and not perceived to exert any external influence on an athlete’s decision to RTS.30Three studies found athletes placed internal pressure on themselves to RTS prematurely based on personal goals,not wanting to let the team down,and not wanting to be withheld from participating.31,38,39Internal pressure led athletes to minimize or mask concussion symptoms in order to keep playing.31,39
3.7.3. Sense of identity
A single study described the loss of identity associated with losing one’s status as a star player and the perceived need to re-establish their identity on a team as a reserve player after a significant absence from sport due to concussion.38
4. Discussion
Our systematic review of the evidence suggests a broad spectrum of psychosocial factors influence RTS following concussion. This evidence can be used as a starting point to advance clinical decision-making and research priorities.Overall,our findings align with reviews in the orthopedic literature indicating that psychosocial factors are an important but understudied consideration in RTS following concussion.9,19,45At RTS, some athletes continue to experience clinically relevant levels of fear, anxiety, and pressure.The role of depression, mood, and perceived stress, however,is unclear, as they appear to improve throughout recovery without influencing time to RTS. Social support may play a positive role in RTS,although athletes’needs may differ from support provided. Given the limited body of concussion-specific evidence and diversity of outcome measures used,what is not known is: (a) which psychosocial factors are associated with pre-injury level of performance or risk of recurrent concussion;(b)which outcome measures best measure those concepts; and (c) established threshold criteria to inform clinical decision-making.
Consistent with previous reviews on psychosocial factors associated with RTS following orthopedic injury,9,19we found fear and emotional factors to be the most commonly explored concepts in predominantly male contact athletes. Our findings suggest that fear is a multidimensional construct that plays a prominent role at the time of RTS and has the potential to either accelerate (e.g., fear of losing playing status) or hinder(e.g., fear of recurrent concussion) returning to sport. This extends previous orthopedic research that indicates fear of reinjury is associated with lower rates of return to preinjury level of sport and higher rates of subsequent injury.12,13In the context of concussion,it is important for the clinician to distinguish between 2 fear-related psychological constructs:kinesiophobia and fear of recurrent concussion. Kinesiophobia is a fear-avoidance behavior caused by concern that movementinduced pain is dangerous or harmful and should thus be avoided.46,47This behavior aligns with clinical recommendations regarding symptom-limited activity during the early stages following concussion when recovery is incomplete and physical activity exacerbates symptoms; thus, kinesiophobia more aptly describes fear of an exacerbation.Fear of recurrent concussion is conceptually different in that it pertains to the consequences of a subsequent concussion that may occur after the initial injury has fully healed and the athlete is medically cleared to RTS.48The use of the same outcome measure(Tampa Scale of Kinesiophobia) to assess both fear of movement and fear of recurrent concussion in different studies underscores the need to better define fear-related psychological constructs.
According to our findings, concussed athletes experience high levels of anxiety at RTS.This presents unique challenges in terms of disentangling a primary trauma-related biological cause of anxiety from a secondary psychological response following concussion, since anxiety is a common symptom of concussion and athletes with pre-existing anxiety are more likely to experience higher levels of anxiety following concussion.49A previous systematic review suggests athletes with orthopedic injury may also experience performance-related anxiety related to a loss of confidence in their ability to meet performance expectations.19Performance-related anxiety plays a role in successful RTS following orthopedic injury19but has not yet been studied in relation to concussion.
Internal and external pressure to keep playing,as identified in the review, contributes to high rates of underreporting concussion symptoms, which is associated with protracted recovery.50The invisible nature of concussion poses unique psychosocial challenges compared with orthopedic injuries that have objective markers of recovery to inform RTS clinical decisions. Positive social support from role models with similar injuries is important in reducing pressure by helping athletes develop confidence that they can overcome their injuryand attain performance-related goals,18which can mitigate fear and anxiety.51Clinicians need to be able to recognize these factors and address them throughout recovery to promote psychosocial wellbeing.
4.1. How does existing research align with current RTS recommendations following concussion?
International consensus2and national professional position statements52on concussion in sport recommend symptom-free progression through a 6-step graduated exercise strategy to determine physical readiness for when it is safe for an athlete to RTS. A stated goal of the final step before return to unrestricted competition is the restoration of athlete confidence—a psychological concept. The 2016 Consensus Statement on Return to Sport echoes the importance of considering a biopsychosocial model to guide RTS following injury.23Importantly,however, consensus guidelines do not provide recommendations on how confidence is defined(either injury-related or performance-related),how to restore confidence,how to establish when an athlete is psychologically ready to RTS,or which outcome measures to use. These are meaningful considerations,given that higher levels of confidence are associated with increased rates of RTS following orthopedic injury.53,54Confidence has also been demonstrated to become more positive throughout recovery following orthopedic injury,9suggesting that psychological readiness may also play a role in measuring recovery following concussion.Preliminary evidence suggests the 6-item Injury-Psychological Readiness to Return to Sport Scale is a valid and reliable measure of confidence in returning to sport among athletes with orthopedic injuries,55but it has not yet been validated in athletes with concussion. It is noteworthy that none of the studies included in this review discussed the concept of confidence following concussion despite the fact that it is identified in the 6-step RTS strategy and is critical in both successful athletic participation2,56,57and RTS following orthopedic injury.9,19Absent empirical evidence, it is currently unknown whether physical and psychological recovery occurs at the same pace throughout the 6-step RTS strategy.
Ardern et al.9and Paterno et al.13have previously argued that measures of psychological readiness should be included in RTS algorithms. Psychological readiness has been described as“the degree to which athletes feel that they are ready—from a psychological standpoint—to return to sport”.58Yet, concussed athletes are rarely kept out of sport because they are not psychologically ready40despite growing evidence of the impact of psychological factors(i.e.,fear,anxiety,confidence,and motivation) on recurrent injury rates and return to preinjury performance levels following orthopedic injury.3-5,13Despite evidence that youth athletes with lower psychological readiness are at a significantly higher risk for 2nd anterior cruciate ligament injury following primary reconstruction,5no standardized outcome measures have been validated to assess psychological readiness to RTS in athletes following a concussion. Based on the combined findings of this review and the recommended 6-step RTS strategy, the most promising outcome measure that could be adapted for concussion may be the Anterior Cruciate Ligament—RTS after Injury scale that was developed to address 3 psychological responses(emotions, confidence in performance, and risk appraisal)identified in the literature as associated with successful RTS after anterior cruciate ligament reconstruction.54Use of this measure in a concussion population needs to be validated before it is widely adopted in clinical practice to identify athletes who might be at risk of an adverse outcome and who might benefit from education or psychological intervention.23,59,60
4.2. Clinical implications
Experts acknowledge that biologic recovery may extend beyond symptomatic recovery.61Likewise, it is plausible that psychological readiness may not occur in parallel with either of these 2 processes and would need to be measured separately and directly rather than assumed.Currently,measures of physical readiness are prioritized in making RTS medical clearance decisions following concussion. Clinicians need to be aware of and consider additional psychosocial factors in determining whether an athlete has recovered following concussion. Sport medicine specialists such as team physicians,physiotherapists, and athletic therapists are ideally positioned to evaluate an athlete’s psychological readiness given their role in monitoring symptoms and progressing an athlete through the recommended 6-step graded exercise strategy to RTS.2,62While RTS is often considered proof of successful recovery, evidence that psychosocial factors are associated with rehabilitation outcomes throughout recovery following orthopedic injury suggests that clinicians may want to consider screening concussed athletes throughout the recovery process to monitor post-traumatic growth and proactively mitigate negative psychological responses.9,19Research into whether maladaptive psychological responses are associated with persistent postconcussion symptoms has the potential to profoundly alter the clinical management of athletes unable to RTS.19Ultimately, it remains to be seen whether psychological interventions can improve RTS outcomes.
4.3. Knowledge gaps and future research
It is essential to adopt a standardized definition of psychological readiness in general (i.e., what we are measuring) and to determine which concepts are relevant to concussion specifically, by integrating the broader literature base with qualitative research obtained from key informant groups such as athletes, coaches, and sport medicine clinicians. Further research is needed to identify whether additional psychosocial factors,such as scholarships or financial incentives,play a role in RTS decision-making. Evidence of a prognostic effect for return to preinjury level of performance or risk of recurrent injury is needed from high quality prospective studies of sufficient power to guide RTS medical clearance decisions and inform future consensus guidelines.23These studies should examine sex and gender-specific differences since males and females respond differently to concussion.63Similarly,studies should take into account age-specific differences given that children appear to take longer to recover than adults.64
4.4. Strengths and limitations
A strength of this systematic review is the inclusion of qualitative research, which is traditionally excluded,65with the quantitative research. This allowed for a clinically relevant framework that integrated the in-depth description of the lived experience of athletes with statistical insight, which is especially important given the nascent body of literature.The limitations of this systematic review extend to athletes, clinicians,and researchers. First, although we used previously published search strategies from the broader literature to inform our study design, the lack of a standardized definition of psychological recovery/readiness could result in missed relevant studies using unfamiliar terminology.Nonetheless,14 studies28-41were included in this review, all of which had small sample sizes; only one32did a sub-analysis for sex, and all28-41were published within the past 5 years, which highlights a significant knowledge gap. Second, our findings are drawn from a relatively homogenous sample of male youth athletes in American football and ice hockey and may not be generalizable to other populations. Furthermore, differences in psychosocial factors based on mechanism of injury need to be clearly delineated, as litigation and/or compensation have the potential to influence recovery following non-sport-related concussion(e.g., motor vehicle collisions).66Our review, which included only participants with sport-related concussion, did not identify these and potentially other relevant psychosocial factors.Third, none of the included studies measured the association between psychosocial factors at the time of medical clearance and commonly used measures of clinical recovery such as symptom assessment, neurocognitive function, or balance,which precluded meta-analysis. Although it was outside the scope of this review, it is possible that psychosocial factors may vary depending on age,gender,or sporting level.Fourth,the lack of an accepted standardized definition of sport-related concussion within the field renders comparisons between studies problematic.67This is magnified by the lack of objective measures of recovery following concussion.
5. Conclusion
Although current medical clearance decisions prioritize physical measures of recovery,evidence suggests diverse psychosocial factors influence RTS following concussion. It remains unclear which factors contribute to psychological readiness and successful RTS.In order to support RTS clinical decision-making,future studies should evaluate the association of psychological factors with physical measures of recovery at medical clearance, preinjury level of performance, and risk of recurrent concussion. The influence of sex/gender and age on psychological readiness to RTS has not been studied.
Acknowledgment
We thank Katie O’Hearn (Children’s Hospital of Eastern Ontario Research Institute), for methodological assistance with developing the electronic search strategies.
Authors’contributions
JvI contributed to the conception,design,analysis and interpretation of the work and drafted the manuscript; KFP and JGC contributed to the design, analysis and interpretation of the work,collected the data,and critically reviewed the manuscript for important intellectual content;MS contributed to the design of the work, developed the search strategies, and critically reviewed the manuscript for important intellectual content; RZ contributed to the conception and design of the work, and critically reviewed the manuscript for important intellectual content. All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
JvI reported receiving speaking honoraria and travel expenses for presentations at scientific meetings and is the founder of and an instructor for R2P Concussion Management.RZ reported being a co-applicant on a competitively funded grant administered by the National Football League through the independent scientific advisory board to fund a prospective concussion study with the goal of preventing concussions; he does not personally receive any funding for this work;his institution receives the operating funds to conduct the research;He has received honoraria from Parachute Canada (a Canadian non-profit for injury prevention)for his role on the Concussion Expert Advisory committee; He is also the co-founder, Scientific Director, and a minority shareholder in 360 Concussion Care, which is an interdisciplinary concussion clinic. All the support had no involvement in the study design and writing of the manuscript or the decision to submit it for publication.The other authors declare that they have no competing interests.
Supplementary materials
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jshs.2022.01.001.
 Journal of Sport and Health Science2022年4期
Journal of Sport and Health Science2022年4期
- Journal of Sport and Health Science的其它文章
- The Journal of Sport and Health Science:Commemorating a decade of publishing milestones and impact
- Prevalence of meeting 24-Hour Movement Guidelines from pre-school to adolescence:A systematic review and meta-analysis including 387,437 participants and 23 countries
- Do people with low back pain walk differently?A systematic review and meta-analysis
- Lymphangiogenesis contributes to exercise-induced physiological cardiac growth
- Influence of biological sex and exercise on murine cardiac metabolism
- Exercise promotes angiogenesis by enhancing endothelial cell fatty acid utilization via liver-derived extracellular vesicle miR-122-5p
