A retrospective study of unfavorable fractures during sagittal split osteotomy:A single surgeon’s experience
Haoshu Chi,Ming Cai
Department of Oral and Craniomaxillofacial Surgery,Shanghai Ninth People’s Hospital,College of Stomatology,Shanghai Jiao Tong University School of Medicine,National Clinical Research Center for Oral Diseases,Shanghai Key Laboratory of Stomatology &Shanghai Research Institute of Stomatology,Shanghai 200011,China
Keywords:Unfavorable fracture Sagittal split ramus osteotomy Classification Surgeon’s experience
ABSTRACT Background: Unfavorable fractures are among the most common complications of bilateral sagittal split ramus osteotomy (BSSRO).This study aimed to evaluate unfavorable fracture patterns during BSSRO and assess the related risk factors and treatment measures.Methods: The clinical records and radiographs of 679 patients (1 358 sides) who underwent BSSRO at Shanghai Ninth People’s Hospital between September 2013 and December 2021 were examined.Results: Patients with unfavorable fractures who underwent surgical restoration were studied.The incidence of unfavorable fractures was 0.8% (n=11),with the highest rate in the third year.The unfavorable fractures were divided into three types by location and clinical treatment:(1)SSRO could still be completed after buccal/lingual plate unfavorable fracture (0.6%, n=8);(2) condylar/coronoid process fractures/intermaxillary fixation needed(0.1%, n=2);(3) additional osteotomy required (0.07%, n=1).Conclusion: These results suggest that as a surgeon’s experience increases,the rate of unfavorable fractures may decrease.The novel classification of unfavorable fractures for SSRO might be useful for surgeons to make appropriate treatment choices during orthognathic surgery.
1.Introduction
Unfavorable fractures are among the most serious complications of sagittal split ramus osteotomies (SSROs) to correct mandibular deformities.1Unfavorable fractures reportedly occur in 0.21%-22.72% of cases.2-5These fractures can cause infections,delayed bone healing,and malfunction and decrease postoperative stability.6-8
Many scholars have systematically discussed unfavorable fracture patterns during SSRO.Most studies have classified unfavorable fracture patterns into several categories according to fracture lines or anatomic locations.9-11Nevertheless,no study has divided unfavorable fracture patterns,which correspond to practical clinical treatment measures,or examined the relationship between the incidence of bad splits and a single surgeon’s experience.
Thus,the medical records of a series of patients treated by the same surgeon over nine years were retrospectively assessed to determine the relationship between unfavorable fractures and surgeon experience.During SSRO,a novel classification of unfavorable fracture patterns was established based on different corrective treatments.
2.Materials and methods
2.1.Clinical materials
The medical records and radiographs of consecutive patients who underwent SSRO between September 2013 and December 2021 were retrospectively examined.Sex,age,diagnosis,SSRO type (unilateral or bilateral),and the presence of a third molar were screened from the patients’medical records.Various mandibular dentoskeletal deformities were included in this study.All patients were discharged from the hospital within a week postoperatively and were asked to return for evaluation at 2 weeks and 1,6,and 12 months after discharge.The study complied with the Code of Ethics of the World Medical Association(Declaration of Helsinki).The protocol of this study was reviewed and supported by the Shanghai Ninth People’s Hospital,Shanghai Jiao Tong University School of Medicine.
2.2.Osteotomy technique
All included patients underwent SSRO by a single surgeon in Shanghai Ninth People’s Hospital.Just above the mandibular foramen,a horizontal lingual bone cut was made.The sagittal osteotomy was continued along the anterior mandibular ramus and the external oblique ridge to the mesial edge of the second molar.A vertical cut line was made on the buccal surface between the first and second molars.All split lines were created using a reciprocating saw and two 8-mm-wide osteotomy blades to split the proximal and distal bone segments.
3.Results
The patients comprised 389 women and 290 men with a mean age of 25.5 (range,18-55) years (Table 1).Eleven of the 1 358 sides had unfavorable fractures(n=11,0.8%).All 8 cases of class I fractures were on the buccal plate,2 cases of class II fractures extended to the coronoid process,and 1 case of class III fractures was on the buccal plate(Table 2).As the surgeon’s experience increased,the number of adverse fractures significantly decreased (Fig.1).The highest incidence of unfavorable fractures occurred in the third year(n=5,0.4%).
Although BSSRO was planned in all cases,the procedure was converted to intraoral vertical ramus osteotomy on the left side in one patient (Fig.2).All unfavorable fractures were immediately stabilized through plate osteosynthesis with rigid internal maxillary fixation or cortical screws.After six months,all instances appeared fine.
The unfavorable fracture line patterns were classified into three groups by clinical treatment (Table 3,Figs.2-4):(1) sagittal split still completed after the buccal or lingual plate fracture,which could be fixed by monocortical screws and a titanium or reconstructed plate (n=8,0.6%);(2) coronoid process or condylar neck fracture (n=2,0.1%) for which internal maxillary fixation(IMF)was sometimes needed to stabilize the occlusion;(3) other osteotomy and extra fixation,such as posterior vertical body osteotomy(PVBO)and long-term IMF were necessary for unfavorable fractures(n=1,0.07%).

Table 1.Review of patients treated with BSSRO (n=679).
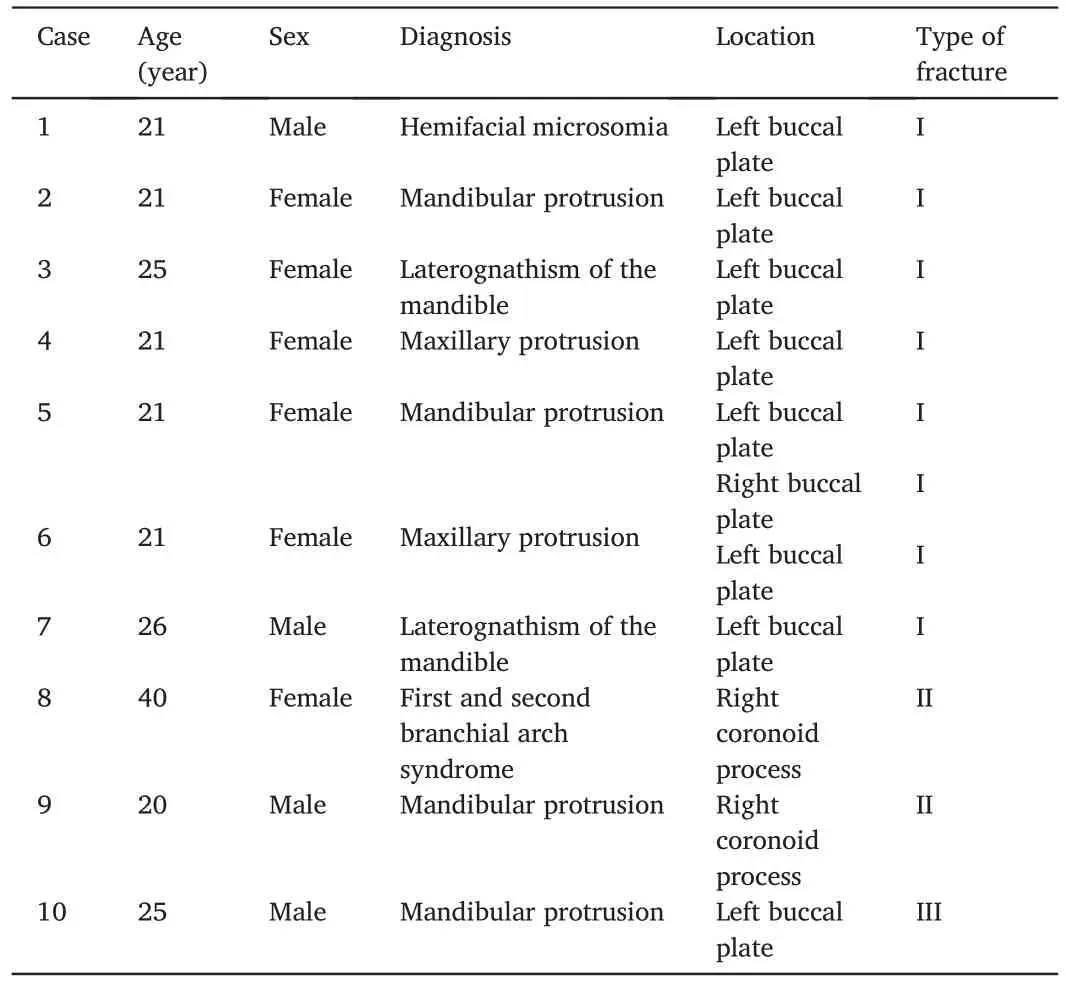
Table 2.Characteristics of the fracture cases.
4.Discussion
BSSRO is among the most common orthognathic procedures for correcting mandibular deformities.12Since it was first described by Trauner and Obwegeser,13a number of troublesome complications have been reported.There exists a certain degree of technical difficulty related to several potential complications.During SSRO,the incidence of unfavorable fractures is 0.21%-22.72%.3,4,14In our study,the incidence was 0.8%,lower than that reported in other studies.We speculate that this may be related to the increased experience of the surgeon over time.
Surgeon experience was identified in this study as an important factorinfluencing the occurrence of unfavorable fractures.Other studies have not reported the impact of the experience.9,15In our study,unfavorable fractures were closely associated with the surgeon’s technology and capabilities.In our study,the overall incidence of unfavorable fractures continued to decline with the rich practical accumulation of experience during the 9-year period (Fig.1).In the first three years,there was an increasing number of unfavorable fractures:1 (5.6%),2 (5%),and 5 (5.1%).The highest number (n=5) was observed in the third year.There have been a few unfavorable fractures in the most recent five years(n=2).The promotion of technology and the abundant experience of the same surgeon were both significant reasons for the decreased incidence.It is difficult for inexperienced surgeons to align and fix fractured segments.Thus,summarizing the experience and lessons immediately could guide residents and reduce unfavorable fracture rates.
Various researchers have classified unfavorable fractures during SSRO.Mensink et al.9divided unfavorable fractures into four patterns:buccal plate,lingual plate,coronoid process,and condylar neck.Steenen et al.11also reviewed unfavorable split pattern types that had been reported in 33 studies and presented appropriate salvage procedures for unfavorable fractures.In 2022,Wang et al.16used 3D reconstruction to assess the fracture patterns of the 2 008 sides and divided unfavorable fractures into several patterns based on anatomical location.It is advantageous for surgeons to summarize their experience to decrease the risk of postoperative functional deficits.However,existing classifications of unfavorable fracture patterns focus only on fracture lines and ignore the appropriate salvage procedures used during SSRO.Thus,we subdivided each fracture into categories (types I-III) by specific treatment(Table 3),which might provide more useful guidance for younger surgeons.
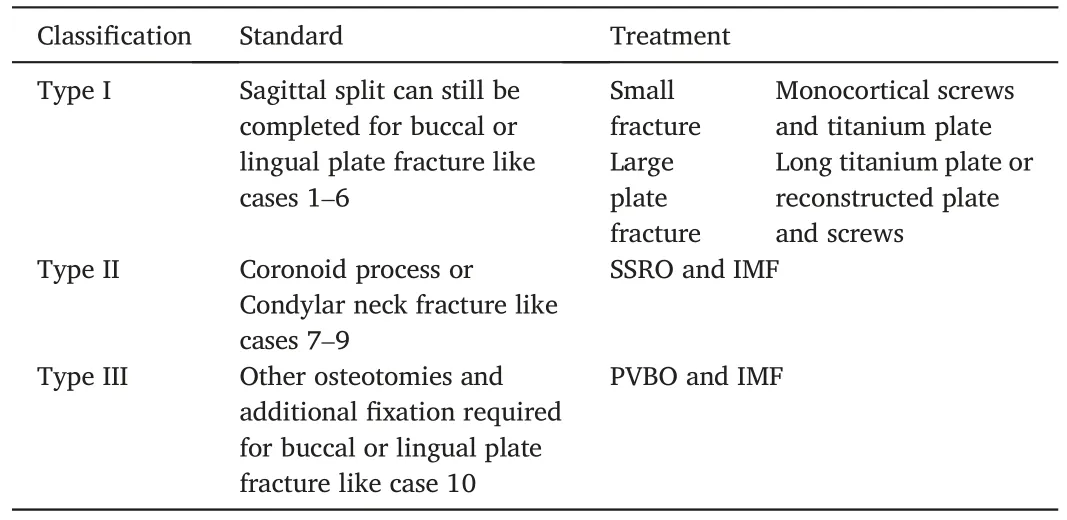
Table 3.Unfavorable split line pattern types and treatments.
Type I splits include all fracture patterns in which sagittal split can still be completed without requiring other additional treatments,including small fractures posterior to the second molars or large fractures on the mandibular ramus.The highest incidence of type I fractures was observed in this study (n=8,0.6%).It was feasible that the fractured segments could be reconsolidated using a titanium plate and monocortical screws.Muto et al.17suggested that these mandibles were larger and thinner than others and that the region of the mandibular angle contained less cancellous bone and more cortical bone.When the distance from the mandibular canal to the buccal cortex is closer,the bone is much thinner.18In our study,five unfavorable type I splits occurred in class III malocclusion patients,including two mandibular laterognathis.At the early stage of independent surgery,considering the longer mandible and thinner mandibular ramus of class III patients,surgeons often did not advance the saw blade sufficiently;thus,they could not grasp the thickness of the medial and lateral bone plates,which usually results in incomplete osteotomy.Therefore,a complete osteotomy was needed to be performed from the medial oblique line to the mandibular angle.
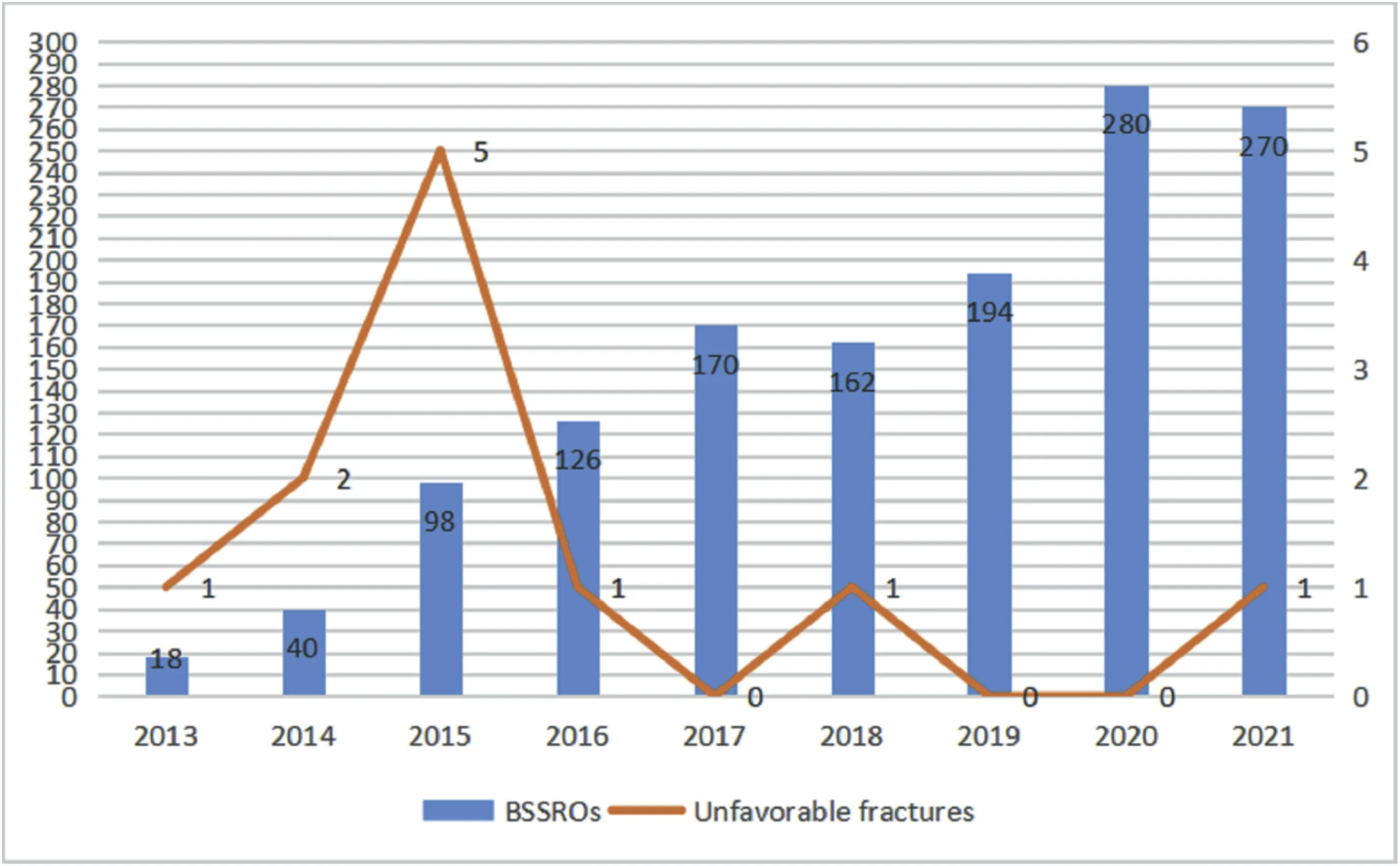
Fig.1.Number of unfavorable fractures relative to number of sagittal split osteotomies per year.BSSRO,bilateral sagittal split ramus osteotomy.

Fig.2.Case 1,type III fracture.A patient with mandibular hyperplasia who underwent SSRO on the right mandible and PVBO on the left mandible.(A)The osteotomy line of the PVBO on the radiograph.(B)Postoperative panoramic view.Titanium plates with four holes were fixed on the bilateral mandible.IMF was maintained for 1 month postoperatively to stabilize the occlusion.
Type II splits include unfavorable fractures extending to the condyle or coronoid process in which SSRO can still be completed.To stabilize the fracture segments,rigid internal fixation can be completed using long reconstructed plates,monocortical screws,or extra titanium plates.When type II fracture occurs,proper positioning of the mandibular condyle in the fossa is important,and IMF must then be performed.Temporomandibular joint disturbance syndrome and delayed bone healing are foci of postoperative attention.Unfavorable fractures of the distracted bone of the right mandible occurred in a typical patient with first and second branch arch syndrome.Implementing the osteotomy was difficult because of the narrow surgical field and severely deformed mandible after mandibular distraction osteogenesis and repair of the facial transversal cleft.The area is vulnerable to injury during BSSRO.A long mini-plate was used to connect the proximal and distal bone segments,and IMF was performed 4 weeks postoperatively to stabilize the occlusion(Fig.3).Therefore,we speculate that this may be related to the abnormal mandibular anatomy.

Fig.3.Case 2,Type II fracture.A patient with first and second branchial arch syndrome who underwent right-sided distraction osteogenesis and a right facial lipoinjection 3 years before the bimaxillary surgery.(A) An extensive buccal plate fracture and long mini-plate was used.(B) Postoperative panoramic view.IMF was maintained for 1 month postoperative to stabilize the occlusion.

Fig.4.Case 3,Type I fracture.(A)A horizontal fracture line on the left buccal plate.(B)A titanium plate with a long bridge on the left mandible was placed directly to connect the fractured segments.One cortical screw was fixed on the ramus to increase its stability.
Type III splits include those in which sagittal split or rigid fixation fails.Sometimes,other surgeries (such as PVBO) can be helpful for treating these difficult cases.It had the lowest incidence in the present study (n=1).Case 1 was the surgeon’s first unfavorable fracture patient(Fig.1).It seems likely that the unfavorable fractures were caused by surgeon’s inexperience and lack of skill.The osteotomy line was too shallow to reach the lower mandibular margin.The fracture occurs in the buccal plate and extends along the oblique line to the lower edge of the mandible,causing a wide range of unfavorable fractures.If sagittal splitting continues,there would not be sufficient space to fix the fracture.The surgery was successfully completed under the guidance of a supervising doctor.Rigid internal fixation could not be performed as a scar would be left after the osteotomy position had been reached using transbuccal retention screws;therefore,long-term intermaxillary fixation was performed.Stable occlusion and favorable bone healing were established at 3 months after recovery.Tomomatsu19suggested that the location of the medial horizontal osteotomy must be at or just above the tip of the lingual fossa and extended medially only as far posteriorly as the lingual fossa.The extension of medial osteotomy should be properly positioned.
Falteret al.20also pointed out that,in addition to operator experience and skill,complications are associated with osteotomy design and attention to detail.Careful analysis of the mandibular anatomy of each case before orthognathic surgery and sufficient attention to details to prevent intraoperative trauma can effectively reduce the incidence of unfavorable fractures.
5.Conclusion
This study demonstrates that as the specialist expertise of a single surgeon increases,the rate of unfavorable fractures decreases.Abundant clinical experience might be useful for surgeons to reduce the incidence of unfavorable fractures.Unfavorable fracture patterns are classified into three types according to the immediate treatments.This may provide a set of guidelines for young surgeons to follow when managing unfavorable fractures.When unfavorable fractures are adequately treated,the chances of functional success are high.
Ethics approval and consent to participate
The need for ethical approval and consent to participate was waived due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Chi H:Data collection,Writing-Original draft.Cai M:Writing-Review and Editing.
Acknowledgments
This study was supported by the University-Industry Collaborative Education Program of the Ministry of Education of China (grant no.201801301030).
 Chinese Journal of Plastic and Reconstructive Surgery2022年2期
Chinese Journal of Plastic and Reconstructive Surgery2022年2期
- Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Foreword from Professor Yu-Ray Chen
- Analyzing the correlation among the five indications of the regenerative effectiveness of expanded skin:A retrospective study of 277 expansion cases
- Major and minor risk factors for postoperative abdominoplasty complications:A case series
- Anesthetic injection pain and hematoma occurrence during upper blepharoplasty:Comparison between thin needles and thick needles
- Assessment and management of immature facial scars by non-surgical methods
- Minimally invasive method to treat a rare wrist injury with simultaneous fractures of the scaphoid and hook of hamate:A case report and literature review
