Assessment and management of immature facial scars by non-surgical methods
Riwina Adel El-Orabi,Mohamed Radwan El-Hadidy,Ahmed Hassan El-Sabbagh
Plastic Surgery Center,Faculty of Medicine,Mansoura University,Mansoura 35516,Egypt
Keywords:Facial scar Immature scar Non-surgical methods
ABSTRACT Background: Scar quality is affected by patients’ wound healing conditions,trauma type,and skin features that differ due to ethnicity.Despite tremendous improvements in scar remodeling techniques,conspicuous scars can still remain postoperatively.Non-surgical methods used for handling scars include the use of topical corticosteroids,pressure therapy,lasers,and platelet-rich plasma (PRP).This study aimed to assess and evaluate different non-surgical modalities for treating immature facial scars.Methods:Fifteen patients with scars were included for non-surgical management.They received one or more of 5 treatments:corticosteroid injection,topical silicone gel application with or without bandage,pressure therapy,lasers,or PRP injection.Scars were assessed using the Patient and Observer Scar Assessment Scale (POSAS) and serial photographs.Results:There were no significant differences in the results obtained using POSAS.None of the patients required a secondary intervention or sought a second opinion.The rate of complications associated with the treatments were very minor.Conclusion: Good assessment of patient characteristics,proper planning,and appropriate treatment lead to favorable outcomes.
1.Introduction
A scar can be defined as a fault or blemish due to former conditions such as a wound,sore,or burn.This scarred tissue lacks the characteristics of normal uninjured skin.1Scars can be classified into many types,such as immature linear,wide,smooth,uneven,trapdoor,depressed,and hypertrophic scars.In plastic surgery,obtaining an inconspicuous scar is the ideal goal.2Some factors can affect the quality and outcome of scars,such as wound healing conditions,the nature of the trauma,and the patient’s skin characteristics (this varies based on patient ethnicity).3
Despite great progress in the scar remodeling techniques,conspicuous scars still form postoperatively.Different non-invasive modalities have been used to treat scars.These therapies have shown some degree of success in improving scar outcomes.The therapies include topical application of silicone gel or vitamin E cream,corticosteroid injection,pressure therapy,dermabrasion,chemical peeling,cryosurgery,use of 5-fluorouracil,lasers,and platelet-rich plasma (PRP).These methods can be used individually or combined.4
The most important criterion for determining the treatment outcome of a scar is its aesthetic appearance.In this study,an attempt was made to assess and evaluate different non-surgical modalities for treating facial scars for less than 6 months.
2.Patients and methods
2.1.Patient data
The patients were admitted to our Plastic Surgery Center between December 2018 and June 2021.Approval for the study was obtained from the university’s ethical committee (no.R/17.01.62).All patients with a facial scar that had been present for less than 6 months were included,with no restrictions regarding age and sex.Patients with unrealistic expectations,mental disorders,or communication and hearing disorders and those unwilling to participate were excluded from the study.Patients who underwent multiple scar revision procedures earlier were also excluded.
All patients were subjected to history-taking,including previous and current medical conditions,medication history,especially antipsychotic drugs,previous surgeries,trauma mechanism,scar duration,and smoking habits.
Finally,15 patients were treated using non-invasive techniques for scar management.They received one or more of the following therapies:topical silicone gel application,corticosteroid injection,with or without bandage,pressure therapy,fractional CO2laser (FCL),or PRP injection.
2.2.Techniques
2.2.1.Silicone gel application
This was the preferred choice for recent scars.Treatment was initiated within a few days of wound closure.Patients were asked to apply a thin film of silicone gel twice daily in a unidirectional manner and rub it with their fingertips for 2-3 min.5
2.2.2.Compression therapy
Pressure was used to prevent,control,and correct hypertrophic scars.Mechanical compression was shown to reduce collagen synthesis.The pressure was applied continuously for at least 12 h per day to ensure effective results.6
2.2.3.Corticosteroid injection
Triamcinolone acetonide 40 mg/mL was injected intralesionally into hypertrophic or keloid scars,and the procedure was repeated at 1-month intervals 4 times until the scars flattened.The corticosteroid injection was limited to the scar itself.This is because extravasation outside of the scar may cause atrophy of the underlying skin.7
2.2.4.Laser therapy
The treated areas were cleansed using a mild cleanser and 70% isopropyl alcohol.Anesthetic cream containing lidocaine,2.5%,and prilocaine,2.5%,(EMLA cream)was applied 1 h before laser therapy.We used a FCL (wavelength:10 600 nm,Deka;FDA approved Unit:Dermatology and Laser Department,Mansoura University).The lowest energy level was used for the first treatment and was increased in the subsequent sessions.
The laser procedure was performed with a pulse duration of 4 ms,12-14 W laser power,and microbeam energy of 48-56 mJ/pulse.The fluence ranged from 24 J/cm2to 28 J/cm2,and the density reached 200 MTZ/cm2.FCL treatment was then applied to the entire scar area.A double-pass was used for each treatment session.A topical antibiotic cream was prescribed after the procedure for 5 days.Laser sessions were repeated at 4-6 week intervals,and 4 sessions were performed for each patient.Response to treatment was assessed at the last follow-up visit (3 months after the final laser session).8,9
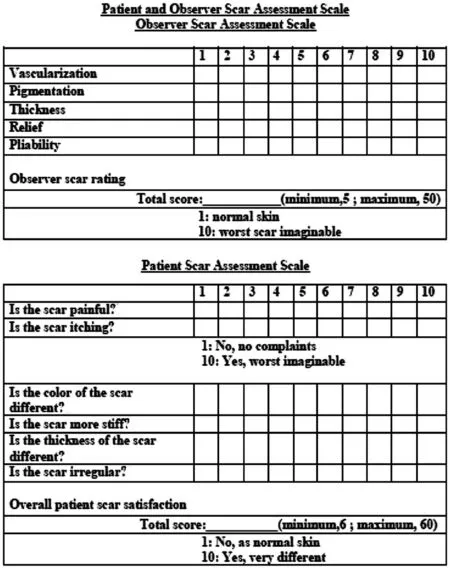
Fig.1.Patient and observer scar assessment scale.
2.2.5.Platelet-rich plasma
It was preferred for recent scars.Blood samples (10 mL) were collected from the patient’s peripheral vein into tubes containing sodium citrate anticoagulant.PRP was obtained after 2 centrifugations.Under aseptic conditions,the first centrifugation was performed at 1 500 rpm for 10 min.Three components were obtained(PRP and a few red blood cells).PRP was aspirated into a new tube for a second centrifugation at 3 000 rpm for 20 min.The middle layer consisting of PRP was aspirated for application.Multiple tiny punctures were made into the dermis using a 30 G needle (1.5-2.0 mm deep).Approximately 2 mL of the collected PRP was then injected into the facial dermis.10
2.3.Questionnaire assessment
Scars were assessed using the Patient and Observer Scar Assessment Scale (POSAS).Patient satisfaction was assessed after 6 months of treatment(Fig.1).11
The scale has two components:the observer and patient parts comprising 5 and 6 numerical items,respectively.Eachitem has a 10-degree score,with 10 indicating the worst imaginable scar or sensation.The total score of the observer part is obtained by adding each of the 5 items(ranging from 5 to50).The total score for the patient parts is obtained by adding each of the 6items(ranging from 6 to 60).The lowest score indicates normal skin,whereas the highest score indicates the worst scar.An overall opinion on scar quality is expressed based on both the observer and patient point rating scale.In this study,paramedical staff with no prior experience in scar assessment completed the observer part.They were allowed to read the instructions before seeing the patient.
2.4.Photographic assessment
Follow-up was done by collecting serial photographs for up to one year.
2.5.Statistical analysis
The collected data are summarized as mean ± standard deviation(SD) and range.Statistical significance was set at P<0.05.A P value<0.001 was considered highly significant,while a P value >0.05 was considered non-significant.All statistical analyses were performed with STATA/SE version 11.2 for Windows (STATA Corporation,College Station,Texas).
3.Results
3.1.Demographic results
The mean age was 18.73±12.72 years(2-38 years).Eleven(73.33%)and 4(26.67%)patients were males and females,respectively.
3.2.Clinical results
No hyperemia,burning sensation,itching sensation,or hyperpigmentation was noted after treatment.None of our patients needed a secondary intervention or sought a second opinion(Figs.2-5).

Fig.2.(A) A 24-year-old male with traumatic scar (3 months duration) on the left side of the face.(B) The same scar 12 months after treatment with silicone gel.

Fig.3.(A)A 34-year-old male with multiple scars(4 months duration)on the right side of the angle of mouth.(B)The scars at 6 months after corticosteroid injection.

Fig.4.(A)Lateral view of the left side of the face in a 45-year-old female with a post-burn scar on the left cheek(4.5 months duration),lower lip area,and neck before treatment.(B) Lateral view of the right side of the face also shows a scar (4.5 months duration) on the right cheek and neck before treatment.(C) Anterior view shows a scar (4.5 months duration) on the mental area before treatment.(D) Lateral view of the left side of the face,12 months after treatment with laser.(E) Lateral view of the right side of the face,12 months after treatment with laser.(F) Anterior view,12 months after treatment with laser.

Fig.5.(A) Anterior view showing post-burn scar of the face of a 29-year-old female (3 months duration) before treatment.(B) Anterior view,12 months after treatment with laser and PRP.
3.3.Analysis of the patient and POSAS
The observer scar scale measures regarding vascularity (P=0.82),pigmentation (P=0.08),thickness (P=0.24),pliability (P=0.64),and relief (P=0.06) were statistically insignificant between patients due to the strict selection of treatment methods according to the scar characteristics.Also,the evaluation was done 6 months after treatment.This allowed a reasonable time for the maturation of scars.(Table 1).For the patient scar scale,itching(mean±SD,1.2±0.41;range,1-2)and other measures,such as pain,color,stiffness,irregularity,scar thickness,and the total score,were insignificant between patients regardless of the method of treatment (Table 2).The results of the scar evaluation based on observer rating,patient satisfaction,and total scores are provided in Table 3.
Silicone gel was used primarily for short hypertrophic scars in 46.67%of cases.For those who did not respond well to topical corticosteroids,intralesional injections were used in 13.33%of cases.Laser was used in 1(6.67%)case.Similarly,laser was used as the main treatment and PRP as adjuvant therapy in 1 case(diffuse scar),combined with silicone gel in 4 cases of multiple,diffuse,and hypertrophic scars in 33.33%of cases.
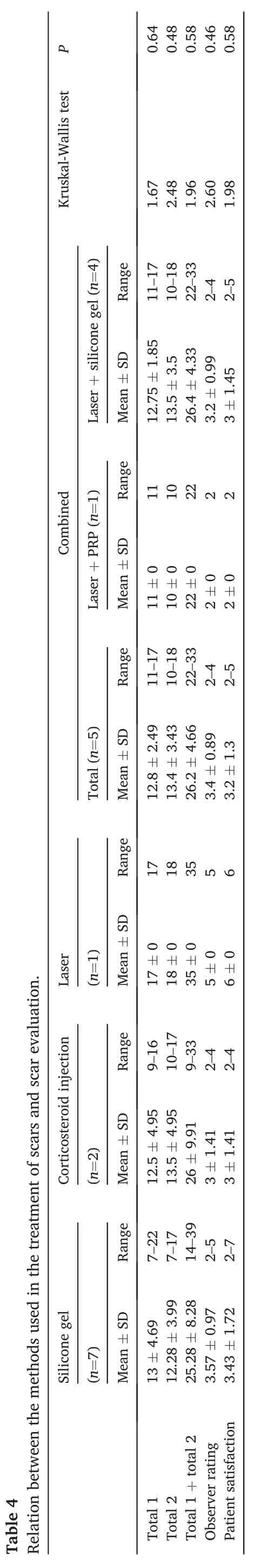
The method used to treat scars showed no significant difference concerning scar evaluation regarding the total score of the observer scar scale (T1),the total score of the patient scar scale (T2),the toal score(sum of T1 and T2),observer rating,and patient satisfaction(Table 4).
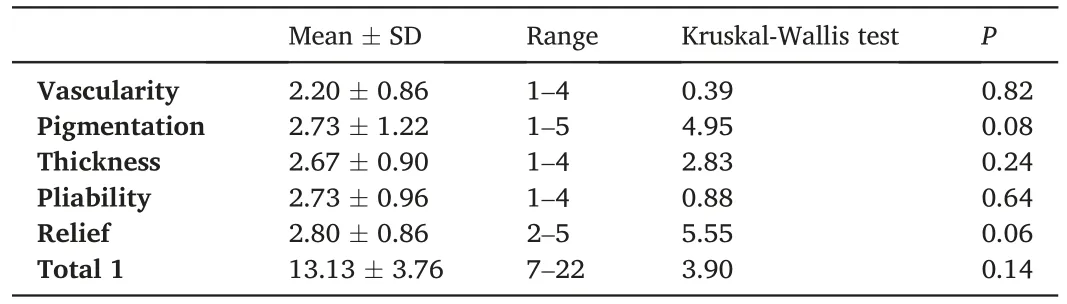
Table 1.Observer scar scale measures.
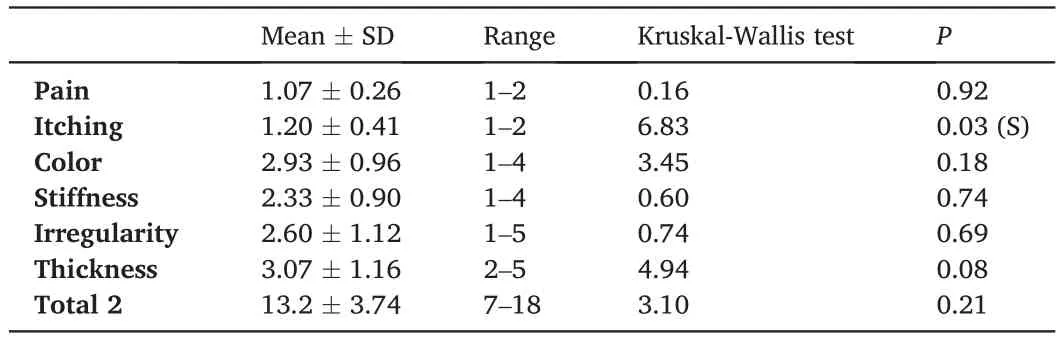
Table 2.Patient scar scale measures.
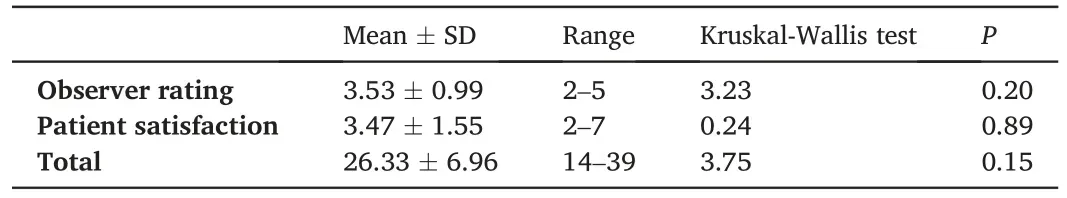
Table 3.Scar evaluation as regards observer rating,patient satisfaction,and total score.
4.Discussion
Scarring is a very distressing phenomenon and is most undesirable when it occurs on the face.12The facial plastic surgeon must be aware of the management modalities,either invasive or non-invasive,to obtain the best result.13An ideal technique should be free of allergic reaction or irritation,cost-effective,less time-consuming,and easily available.In addition,it should provide permanent results,with no rejection or resorption.
Aging tends to decrease skin tension and sebaceous gland activity.Hypertrophic scars are observed at a lower frequency in the elderly.This is in contrast to scars in children,among whom hypertrophic scars are common because of increased cellular activity and increased skin elasticity.14
A study on healthy volunteers during 1-12 months after injury revealed a shorter maturation time and better scar quality in older people than in young individuals.15Although aging could adversely affect the speed of wound healing during early phases,it might accelerate scar maturation and improve scar quality with optimal wound care.16In our study,there was nearly no difference in the scar outcome concerning the age of patients,regardless of the method used.This could be because most of our patients were adults.
Females reported better results following scar correction than males.17Androgens are negative regulators of repair,while estrogens and dehydroepiandrosterone accelerate wound healing by attenuating inflammation and promoting extracellular matrix deposition.A microarray-based study emphasized the importance of estrogen as a regulator of wound healing,18in which the majority of patients were males,as they are the major working power of our society.In the current study,there was almost no significant difference in scar quality outcomes between males and females.However,females were more satisfied with their scar outcomes and got better total scores (mean ± SD=26.25 ± 3.77) than males(mean±SD=26.36±7.98).
We used silicone gel in 7 patients and silicone gel in combination with other methods in 4 patients.This was applied to promote healing and prevent pathological scars early in the postoperative period or for immature scars.Treatment was started as soon as possible to minimize the risk of hypertrophic scars.19We intralesionally injected corticosteroids into keloids in 2 patients to flatten the scar,improve its pliability,and reduce scar-related itching and pain.6The advantage of the intralesional treatment is that it is performed in the outpatient department without requiring surgery and hospitalization.20,21
In our study,we applied FCL alone in 1 patient and FCL in combination with silicone gel in 4 patients.In addition,FCL was combined with PRP in 1 patient.We applied laser therapy to the immature scars 3 months after the injury.For FCL to effectively improve facial scars,4 sessions were conducted for each patient.FCL is relatively expensive;however,one of the advantages of this type of laser is that it has fewer side effects and less downtime after sessions.
Hedelund et al.8showed a statistically significant improvement in atrophic post-acne scars compared to that noted after placebo after 3 monthly laser sessions with an FCL device in 13 patients.In addition,others reported that FCL,when used for the scar treatment,had a total efficacy rate of 96%and a significant efficacy rate in 62%of cases.22
Galal et al.23performed a split-face study on 30 patients with FCL:intradermal saline was used on one side and intradermal PRP was used on the other.They were applied on day 5 after the laser session.They reported significant improvement on both sides of the face;however,blinded observers and patients noted better improvement on the PRP-treated site.Zhu et al.24used a fractional laser with topical PRP in 22 patients with acne scars and reported excellent clinical improvement and patient satisfaction in the PRP-treated patients.
In a study from India,all patients showed statistically significant improvement in the quantitative scoring of scars on both the FCL-only treated side and the FCL+PRP-treated side.However,the difference between the right side(FCL only)and the left side(FCL+PRP)was not statistically significant at the end of the study.Thus,the authors considered both FCL and FCL plus topical PRP to improve the quality of the acne scars significantly.The addition of topical PRP did not significantly alter the final scar outcome compared to that using only FCL.However,PRP in combination with FCL could be recommended as it significantly improves the downtime of FCL.25In this study,we used PRP as an adjuvant therapy with other methods.Our method was in line that of Lee et al.,26as their results confirmed that adjuvant PRP treatment might promote the recovery of laser-damaged skin and decrease downtime.
For the assessment of the results,we used POSAS.The scale has both observer and patient opinions.POSAS is considered a reliable,valid,and comprehensive tool for assessing facial scars.In addition,the scale allows the rating of three important items:itching,pain,and surface area,which are not included in other scales such as the Vancouver Scar Scale.27
Our results did not show any significant difference in the postoperative outcomes of patients managed with different methods of treatment.This might be because various facial scars were present,enabling us to select a suitable mehod based on the scar.Additionally,the second part of the PSOAS(the patient scar assessment scale)depended on the patients’ subjective evaluation.As the evaluation was performed after 6 months,this duration was considered long enough for maturation of the scar and relief of pain (70%).At this time,redness and pigmentation also decreased in most cases.
A limitation of this study was the lack of histological examinations to evaluate wound healing after treatment objectively.In addition,our sample size was small.However,none of our patients required a secondary intervention or sought a second opinion.
5.Conclusion
Facial scars are frustrating for both patients and surgeons.Non-surgical methods are the best to treat immature facial scars.These techniques do not completely erase the scar but make it less noticeable and,hence,more acceptable.A good understanding of the anatomy and wound healing augmented by surgeon experience and careful planning could improve surgical outcomes and greatly reduce unwanted complications.
Ethics approval and consent to participate
This study received ethical approval from the ethical committee of the Mansoura University (approval no.R/17.01.62).The study conformed with the ethical standards set forth in the 1964 Declaration of Helsinki and its later amendments.All participants provided written informed consent prior to study enrollment.
Consent for publication
Informed consent was obtained from all patients for publication of the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
El-Orabi RA:Conceptualization,Methodology.El-Sabbagh AH:Methodology,Writing-Review and editing.El-Hadidy MR:Data curation.
 Chinese Journal of Plastic and Reconstructive Surgery2022年2期
Chinese Journal of Plastic and Reconstructive Surgery2022年2期
- Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Foreword from Professor Yu-Ray Chen
- Analyzing the correlation among the five indications of the regenerative effectiveness of expanded skin:A retrospective study of 277 expansion cases
- Major and minor risk factors for postoperative abdominoplasty complications:A case series
- Anesthetic injection pain and hematoma occurrence during upper blepharoplasty:Comparison between thin needles and thick needles
- Minimally invasive method to treat a rare wrist injury with simultaneous fractures of the scaphoid and hook of hamate:A case report and literature review
- Bowen’s disease with multiple lesions of the penis and scrotum:A case report
