Primary signet-ring cell carcinoma of the extrahepatic bile duct:A case report
INTRODUCTION
Cholangiocarcinoma (CCA) is a common malignant tumor of the biliary system, and 90%-95% of the pathologic types of CCA are adenocarcinomas[1]. Signet ring cell carcinoma (SRCC) is a subtype of poorly differentiated adenocarcinoma with strong invasion and poor prognosis[2]. Although it can occur in various organs, including the stomach, colon, esophagus, bladder, prostate, pancreas, and breast[2], it mainly arises in the stomach[3], where > 96% of SRCCs occur[4]. However, the occurrence of the extrahepatic bile duct is extremely rare.
It was only then that I realized I did not teach my father. He taught me. It was he who had engaged me in the conquest of language. It was he who told me to be direct, to be watchful25, to listen with my eyes and to ask with my mouth. From his silence, my father taught me the true power of speech.
Previously, only a few studies have reported cases of primary SRCC of the extrahepatic bile duct due to the rarity this disease . Herein, we report that a case of primary SRCC of the extrahepatic bile duct diagnosed
a biopsy of the biliary tree. Additionally, we conducted a literature review to describe the epidemiology and explore the treatment and prognosis of the disease.
CASE PRESENTATION
Chief complaints
Abdominal pain, jaundice, and skin pruritus for 2 mo.
History of present illness
The patient was admitted with abdominal pain, jaundice, and skin pruritus for 2 mo.
History of past illness
The patient was previously healthy and had no specific medical history.
You did not know, any better! Ignorance upon ignorance indeed! The poor swineherd took these words to heart, for they wereaddressed to him; he knew not that there were others who wereequally ignorant. Not even a leaf of the plant could be found. Therewas one, but it lay in the coffin of the dead; no one knew anythingabout it.
Personal and family history
However, despite active treatment, the disease progressed rapidly, and the patient died after 1 mo due to liver failure. Therefore, we concluded that primary SRCC of the extrahepatic bile duct is not prone to distant organ metastasis, and if accompanied by distant organ metastasis, it grows rapidly and has a strong invasion and poor prognosis.
Physical examination
Physical examination presented normal vital signs, icteric sclera, visible jaundice, and mild tenderness in the upper right abdominal quadrant.
Laboratory examinations
Tumor-related cell markers were as follows:carbohydrate antigen 19-9, > 2 044 U/mL (reference range:< 35 U/mL); cancer antigen 125, 146 U/mL (reference range:< 35 U/mL); human chorionic gonadotropin, 23.38 IU/L (reference range:< 5 IU/L); alpha-fetoprotein and carcinoembryonic antigen (CEA),within normal range. Laboratory tests:total bilirubin, 446 μmol/L (reference range:5-21 μmol/L); direct bilirubin, 232.9 μmol/L (reference range:0-3.4 μmol/L); indirect bilirubin, 213.1 μmol/L (reference range:1.7-13.6 μmol/L).
Imaging examinations
Primary SRCC of the extrahepatic bile duct is an extremely rare subtype of bile duct adenocarcinoma of unknown origin. Presently, there are two theories regarding its origin. One is that the tumors may arise from ectopic gastric mucosa, while the other is that SRCCs may develop from gastric-type epithelial metaplasia[6]. In our case, no ectopic gastric mucosa and epithelial metaplasia were detected in the biliary biopsy. Thus, the origin of primary SRCC in the extrahepatic bile duct needs to be evaluated in future studies[14].
Diagnostic work-up
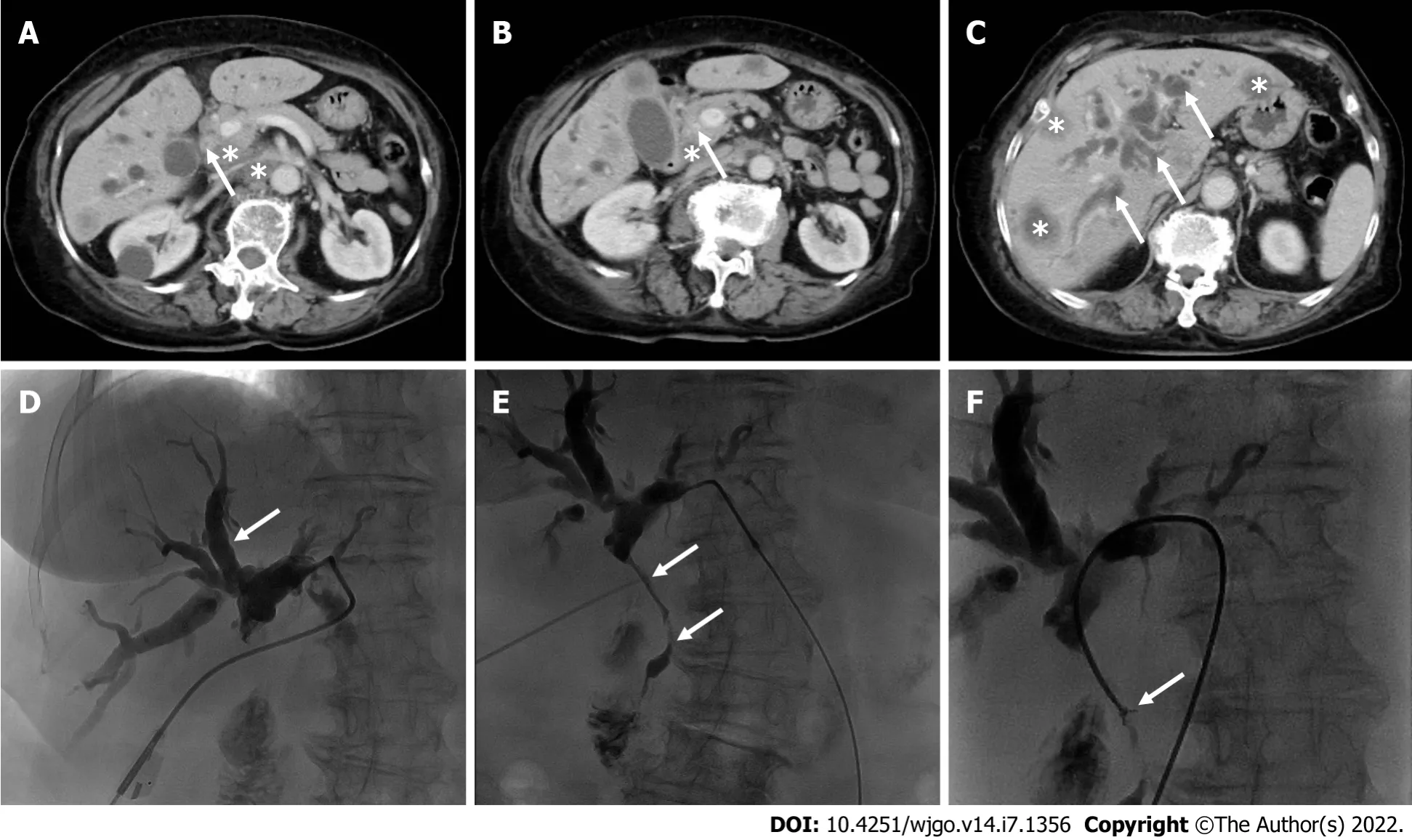
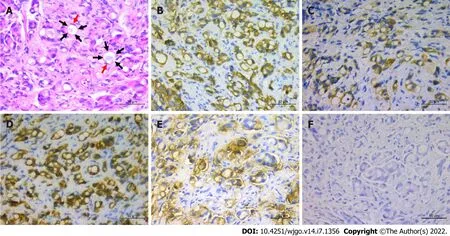
To alleviate jaundice and prolong the overall survival, percutaneous transhepatic cholangiopancreatic drainage (PTCD) was performed. During the operation, segmental stenosis of the extrahepatic bile duct(Figure 1E, arrows) and a vine-like expansion of the intrahepatic bile duct (Figure 1D, arrows) were observed. To determine the nature and origin of the lesion, a biliary biopsy was performed under fluoroscopy (Figure 1F, arrows). Hematoxylin and eosin (H&E) staining revealed abundant mucin in the cytoplasm pushed the nuclei aside, giving the cells the characteristic signet ring morphology(Figure 2A). The pathological diagnosis of the biopsy was SRCC. Immunohistochemistry (IHC) showed the following indicators:CK19 (++), CAM5.2 (+), CK7 (++), CK broad-spectrum (++), CEA (++), Ki-67(10%), CK20 (-), CDX2 (-), glypican-3 (-), hepatocyte (-), vimentin (-), and special staining for PAS (+)(Figure 2B-F). The IHC of biopsy materials showed that the tumor cells were positive for CK19(Figure 2B) and CK7 (Figure 2D) but negative for both CK20 and CDX2, suggesting the biliary tract origin of carcinoma. In addition, the gastroscopy and colonoscopy of the common primary site of SRCC did not show any abnormality.
The Snow Queen might come home now when she pleased, for there stood his certainty of freedom, in the word she wanted, written in shining letters of ice
FINAL DIAGNOSIS
Finally, a diagnosis of primary SRCC of extrahepatic bile duct with distant lymph node metastasis and multiple liver metastases was made based on the radiographic, PTCD, and pathological characteristics.The tumor was diagnosed as T3N1M1 stage IV according to the 8
edition of the American Joint Committee on Cancer (AJCC) cancer staging system[5]. Further imaging, such as positron emission tomography-computed tomography (PET-CT), was essential to determine any other sites of distant metastasis. Nonetheless, due to rapidly deteriorating condition in a short period, the patient died before the PET-CT was completed.
TREATMENT
This patient was treated with S-adenosylmethionine (intravenous infusion, 1.5 g once a day) to protect the liver and relieve jaundice. PTCD was performed simultaneously to alleviate obstructive jaundice.
OUTCOME AND FOLLOW-UP
We have no conflict of interest.
DISCUSSION
"hurt them" in English or "attack them" in Hebrew. The Israeli Defense Force uses Facebook's automated translation to monitor the accounts of Palestinian users for possible threats. In this case, they trusted Facebook's AI enough not to have the post checked by an Arabic-speaking officer before making the arrest.
She had no specific family history.
Contrast-enhanced computed tomography revealed that the wall of the common bile duct was thickened and strengthened (Figure 1A and B, arrows) with intrahepatic bile duct dilation (Figure 1C,arrows), and numerous hypodense lesions in the liver showed slight annular enhancement (Figure 1C,asterisks). In addition, the lymph nodes in the hepatic hilum area, the pancreatic head area, and around the abdominal aorta were enlarged (diameter 1.5-2.5 cm) with mild enhancement (Figure 1A and B,asterisks).
Jorinde sang: My little bird with throat so red Sings sorrow, sorrow, sorrow; He sings to the little dove that s dead, Sings sorrow, sor--jug8, jug, jug
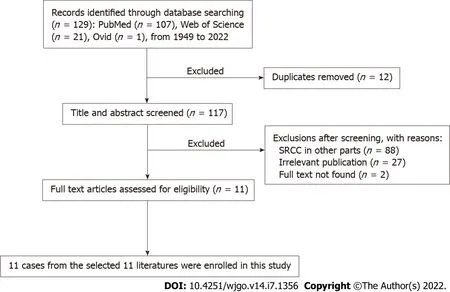
For the literature review, relevant articles in English were retrieved from the PubMed, Ovid database,and Web of Science from 1949 to January 10, 2022. The keywords used for the search were “signet ring cell cholangiocarcinoma” OR “signet ring cell carcinoma of bile duct”. These words were used individually or with the Boolean operator “AND”. A total of 129 articles were analyzed from 1949 to 2022. The flow chart of the literature screening process is illustrated in Figure 4. Finally, 11 cases were included in this meta-analysis. The following data were collected:the name of the first author, year of publication, patient’s age, sex, location, TNM staging, treatment, and follow-up results (Table 1).
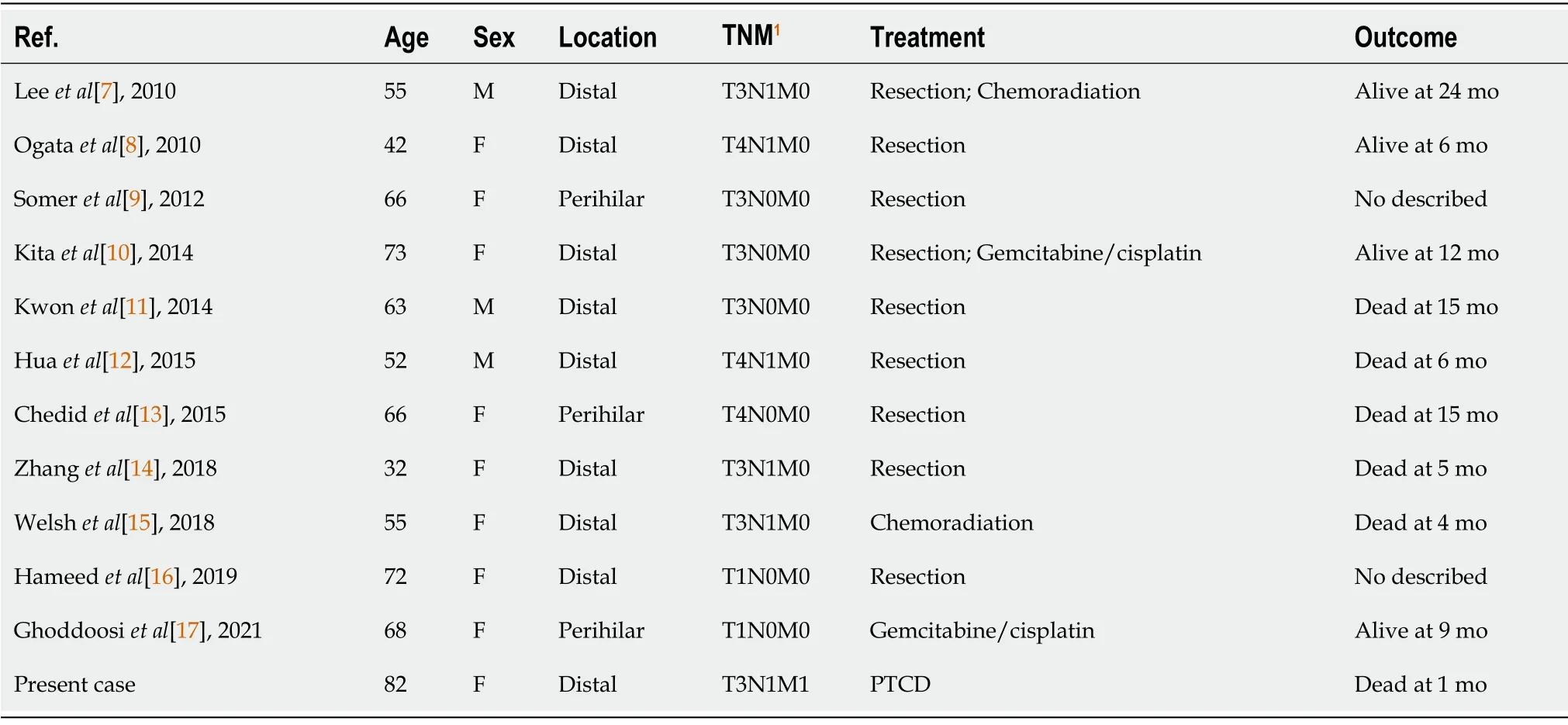
In the current study, we included 3 males[7,10,12] and 8 females[8,9,11,13-17] with an average age of 58.5 years (range:32-73 years). This phenomenon suggested that primary SRCC of the extrahepatic bile duct occurs in elderly patients, which was similar to previous reports[9]. However, due to the small number of patients, the correlation between the incidence of primary SRCC of the extrahepatic bile duct and gender needs to be investigated further. The analysis of 11 patients revealed that primary SRCC of the extrahepatic bile duct occurred in the distal bile duct in 8 cases[7,8,10-12,14-16] and the perihilar bile duct in only 3 cases[9,13,17]. This showed that primary SRCC of the extrahepatic bile duct occurs in the distal bile duct compared to the perihilar bile duct. The mechanism of occurrence may be that the distal bile duct is prone to the ectopic gastric mucosa and gastric-type epithelial metaplasia; however, it needs to be evaluated further[14]. According to the 8
edition of the AJCC cancer staging system, 9 cases[7-15]had an obvious invasion of the extrahepatic bile duct, of which 3[8,12,13] showed infiltration of the adjacent tissue structures. Peritoneum and retroperitoneal lymph node metastasis were observed in 5 cases[7,8,12,14,15] without distant metastasis. This phenomenon indicated that primary SRCC of the extrahepatic bile duct mainly grows along the wall, often with lymph node metastasis, but distant organ metastasis is extremely rare. The treatment for primary SRCC of extrahepatic bile duct includes resection, such as pancreaticoduodenectomy or resection of the biliary tree, followed by radiotherapy and chemotherapy. Also, integrative treatments that combine two or three have been applied[7-17].7/11 cases[8-10,12-14,16] received only surgical resection, 1/11 case[17] received chemotherapy alone,1/11 case[11] received surgical resection followed by chemotherapy, 1/11 case[15] received chemoradiotherapy, and 1/11 case[7] received combined treatment of surgical resection, radiotherapy, and chemotherapy. Currently, surgical treatment is the gold standard for patients with cancer without distant metastasis. However, no standardized protocol and guidelines for treating primary SRCC of the extrahepatic bile duct are currently available because of the limited number of cases and studies. Yang
[2] proposed that the primary SRCC location can be used as an independent prognostic factor of survival and that compared to stomach SRCC, the primary gallbladder, the ampulla of Vater, and pancreatic SRCCs have a worse prognosis. Therefore, an optimal treatment strategy is essential. Based on the results of this study, active surgical treatment may improve the prognosis in the event of surgical conditions in patients. Nonetheless, cases with poor prognosis even after radical resection are apparent.However, a standard recommendation of whether to perform adjuvant radiotherapy or chemotherapy cannot be established because of the small number of patients who received radiotherapy or chemotherapy in this study. Thus, to improve the survival and quality of life of patients, a multidisciplinary treatment such as concomitant use of chemotherapy is necessary.
CONCLUSION
Overall, primary SRCC of the extrahepatic bile duct is extremely rare, and cases with distant organ metastases have never been reported. Currently, surgical treatment is the gold standard for patientswith primary SRCC of the extrahepatic bile duct without distant metastasis. However, aggressive multidisciplinary treatment is essential when surgical resection is not feasible or metastasis is observed.
Xie CB, Wu Y, Li F, and Zhao KF reviewed the literature and contributed to manuscript drafting; Shi RS analyzed and interpreted the patient data; Huang Q provided pathological images; Ao J and Ke D managed the patient; all authors read and approved the final manuscript.
Herein, we present a rare case of primary SRCC of extrahepatic bile duct with distant lymph node metastasis and multiple intrahepatic metastases. To the best of our knowledge, this is the second case confirmed by direct forceps biopsy under fluoroscopy and the first case of primary SRCC of the extrahepatic bile duct with distant organ metastasis. Distant organ metastasis is a critical factor influencing prognosis. Therefore, our case had a worse prognosis compared to those reported previously. Moreover, surgical resection was not a reasonable treatment due to the patient’s old age and poor liver function; hence, she received only palliative treatment, including liver protection and PTCD.
the Zunyi City Science and Technology Department, No. HZ-2021-44.
When I was doing hill sprints6 to prepare for my ski racing7 - my heart and lungs and leg muscles all on fire - I d often be hit by the sensation that there were no resources left inside me with which to keep going. Then I d think about the races ahead - my dream of pushing my potential as far as it could go, the satisfaction of breaking through my own barriers - and that would get me through the sprints. The same tenacity8 that served me so well in ski racing helped me survive my second bout1 with cancer.
Informed consent was obtained from the patient’ family for the publication of this case as the patient has deceased.
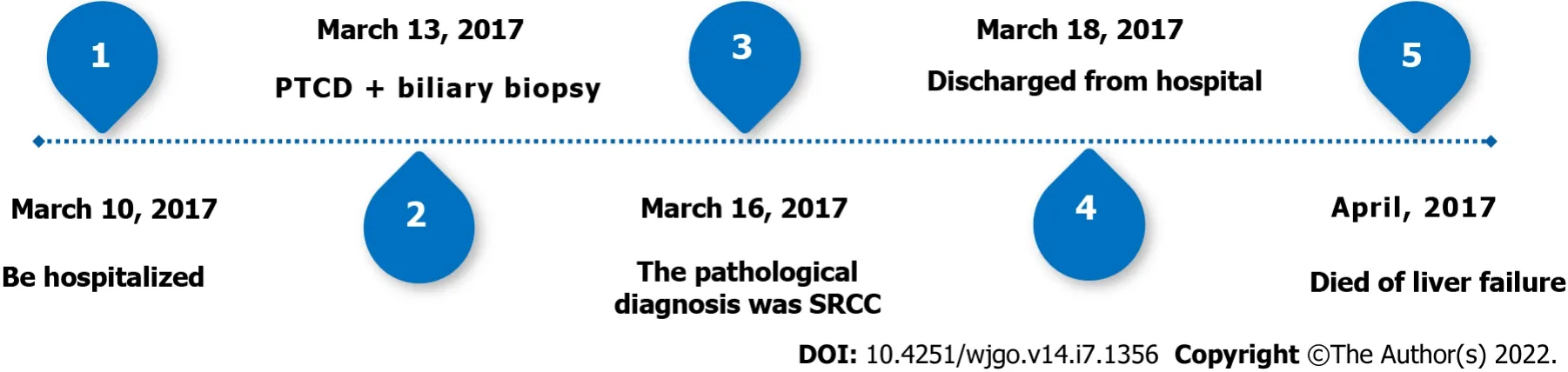
The patient died after 1 mo due to liver failure. The timeline can be seen in Figure 3.
The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See:https://creativecommons.org/Licenses/by-nc/4.0/
China
Chao-Bang Xie 0000-0001-6976-4357; Yang Wu 0000-0003-1976-7968; Feng Li 0000-0001-5350-4040; Kai-Fei Zhao 0000-0002-8274-2600; Rong-Shu Shi 0000-0002-4052-1308; Qiong Huang 0000-0001-7178-9027; Jin Ao 0000-0003-2774-8812.
7 No, wife, said her husband, that I won t do; how could I find it in my heart to leave my children alone in the wood?8 The wild beasts would soon come and tear them to pieces
Yan JP
With his huge club he aimed a terrific blow at Narcissus, which must certainly have killed him but for the adroitness58 of the Fairy Melinette, who arrived upon the scene just in time to snatch him up and carry him off at lightning speed to her castle in the air
Filipodia
Yan JP
1 Brindley PJ, Bachini M, Ilyas SI, Khan SA, Loukas A, Sirica AE, Teh BT, Wongkham S, Gores GJ. Cholangiocarcinoma.
2021; 7:65 [PMID:34504109 DOI:10.1038/s41572-021-00300-2]
2 Yang M, Yang Y, Chen J, Stella GM, Um SW, Tandon YK, Liu H. A case report of primary signet ring cell carcinoma of the lung:imaging study and literature review.
2021; 10:3840-3849 [PMID:34733632 DOI:10.21037/tlcr-21-654]
3 el-Zimaity HM, Itani K, Graham DY. Early diagnosis of signet ring cell carcinoma of the stomach:role of the Genta stain.
1997; 50:867-868 [PMID:9462273 DOI:10.1136/jcp.50.10.867]
4 Wang S, Li J, You J, Zhou Y. Clinicopathological characteristics and prognosis of signet ring cell carcinoma of the gallbladder.
2021; 21:248 [PMID:34090347 DOI:10.1186/s12876-021-01831-4]
5 Amin M. AJCC Cancer Staging Manual. 8th ed. American Joint Committee on Cancer; 2017 [DOI:10.1007/978-0-387-88441-7]
6 Hoedemaeker PJ. Heterotopic gastric mucosa in the duodenum.
1970; 3:165-173 [PMID:4915587 DOI:10.1159/000197027]
7 Lee EY, Kim C, Kim MJ, Park JY, Park SW, Song SY, Chung JB, Kim H, Bang S. Signet ring cell carcinoma of the extrahepatic bile- duct.
2010; 4:402-406 [PMID:20981222 DOI:10.5009/gnl.2010.4.3.402]
8 Ogata S, Kimura A, Hatsuse K, Yamamoto J, Shimazaki H, Nakanishi K, Kawai T. Poorly differentiated adenocarcinoma with signet-ring cell carcinoma of the extrahepatic bile duct in a 42-year-old Japanese female:a case report.
2010; 64:63-65 [PMID:20200586 DOI:10.18926/AMO/32860]
9 Somer L, Andrejić B, Milošević P. Origin and pathological characteristics of Klatskin tumor:a case report and literature review.
2012; 63:65-70 [PMID:22535609]
10 Kita E, Tsujimoto A, Nakamura K, Sudo K, Hara T, Kainuma O, Yamamoto H, Itami M, Yamaguchi Y. Signet ring cell carcinoma of the extrahepatic bile duct diagnosed by preoperative biopsy:a case report.
2014; 8:353-357 [PMID:25520605 DOI:10.1159/000369249]
11 Kwon HJ, Yoon GS, Kwon YC, Kim SG, Jeong JY. Signet-ring cell carcinoma of the distal common bile duct:report of a case.
2014; 48:315-318 [PMID:25214866 DOI:10.4132/KoreanJPathol.2014.48.4.315]
12 Hua R, Zhang JF, Liu W, Huo YM, Sun YW. Signet-ring cell carcinoma coexisting with adenocarcinoma arising in a choledochal cyst:report of a case.
2015; 45:1049-1052 [PMID:25352010 DOI:10.1007/s00595-014-1049-3]
13 Chedid MF, Lucas ET, Cerski CT, Lopes MF, Amaral OB, Chedid AD. Signet-ring cell hilar cholangiocarcinoma:case report.
2015; 28:148-149 [PMID:26176256 DOI:10.1590/S0102-67202015000200016]
14 Zhang C, Zhou J, Kou K, Liu S, We F, Wang G. Occurrence of signet-ring cell carcinoma with cholangiocarcinoma 25 years after choledochal cyst excision:A case report.
2018; 97:e9956 [PMID:29465585 DOI:10.1097/MD.0000000000009956]
15 Welsh JL, Jaber O, Ivanovic M, Johlin FC, El Abiad RG, Clamon GH, Smith MC, Chan CHF. Rapidly Progressing Primary Extrahepatic Bile Duct Signet-Ring Cell Carcinoma in a Caucasian Woman.
2018; 49:63-66 [PMID:27270710 DOI:10.1007/s12029-016-9843-3]
16 Hameed N, Stephen M. Signet Ring Cell Carcinoma of the Extrahepatic Bile Duct:A Case Report.
2019; 152:S68-S69 [DOI:10.1093/ajcp/aqz113.077]
17 Ghoddoosi M, Hormati A, Ouladdameshghi D, Ahmadpour S. Signet ring cell hilar cholangiocarcinoma diagnosed
direct transpapillary cold forceps biopsy under fluoroscopy.
2021 [PMID:33647345 DOI:10.1016/j.gastrohep.2021.01.005]
 World Journal of Gastrointestinal Oncology2022年7期
World Journal of Gastrointestinal Oncology2022年7期
- World Journal of Gastrointestinal Oncology的其它文章
- Gut microbiome and pancreatic cancer cachexia:An evolving relationship
- Prospects and applications of enucleation in solid pseudopapillary neoplasms of the pancreas
- Claudin 18.2 is a potential therapeutic target for zolbetuximab in pancreatic ductal adenocarcinoma
- KIFC3 promotes proliferation, migration and invasion of esophageal squamous cell carcinoma cells by activating EMT and β-catenin signaling
- Differences of core genes in liver fibrosis and hepatocellular carcinoma:Evidence from integrated bioinformatics and immunohistochemical analysis
- Efficacy of neoadjuvant chemotherapy for initially resectable colorectal liver metastases:A retrospective cohort study
