Epidemiology and region-specific risk factors for low Apgar scores in China: a nationwide study
Yi-Wen Wang · Yan Chen · Yan-Hong Ming · Jin-Wen Zhang · Kun Sun · Jun Zhang · Yong-Jun Zhang
Abstract
Keywords Apgar score · China · Epidemiology · Risk factor
lntroduction
Neonatal asphyxia is a major cause of neonatal mortality and disability worldwide. Neonatal asphyxia accounts for 23%of global neonatal deaths [ 1]. In China, the infant mortality rate averaged 13.0 deaths per 1000 live births in 2013 [ 2]. Of all infant deaths, 17.1% resulted from intrapartum hypoxicischemic events (asphyxia) [ 3]. To achieve the national goal of infant and < 5-year mortality rates of five and six per 1000 live births, respectively, by 2030 [ 4], it is essential to know the preventable causes of neonatal asphyxia and take appropriate measures.
A low Apgar score has been widely used as a proxy for asphyxia. Initially, the score was measured at 1 minute.However, the Apgar score at 5 minutes later showed a better predictive value for not only neonatal death but also infant death and poor neurological outcomes, of both very preterm,preterm and term infants in the post-neonatal period [ 5– 8].The incidence of low 5-minute Apgar scores varies widely in the literature [ 5, 9, 10]. A study from the UK showed a rate of 15.4/1000 live births for a 5-minute Apgar score under 7[ 5], while a study including 23 countries or regions participating in the Euro-Peristat project reported that scores < 7 ranged from 3 to 24 per 1000 live births [ 11]. However, the epidemiology of low Apgar scores in China remains unclear.
This study used data from the China Labor and Delivery Survey to estimate a low 5-minute Apgar score rate, to describe the region-specific risk factors related to low Apgar score, and to explore potentially preventable risk factors in China.
Methods
Study setting and design
The China Labor and Delivery Survey was a multicenter cross-sectional study conducted throughout the country,between March 1, 2015, and December 31, 2016. The participating hospitals were approached through obstetric networks. Hospitals with 1000 or more deliveries per year were eligible for inclusion. A total of 96 hospitals distributed in 24 (out of 34) provinces, municipalities, and autonomous regions in China were included in the analysis. The standard partition for geographical regions in China was used(Central, North, South, East, Southwest, Northwest, and Northeast) [ 12]. Hospital levels were officially determined by local governments [ 13].
Study variable
A low 5-minute Apgar score or very low 5-minute Apgar score was defined as < 7 or < 4 at 5 minutes after birth,respectively. Gestational age was ascertained on the basis of the last menstrual period or ultrasound dating in the first trimester when the date of the last menstrual period was uncertain.
Maternal pre-pregnancy body mass index [BMI, defined as weight in kilograms divided by the square of height in meters (kg/m 2 )] was categorized as follows: underweight(< 18.5 kg/m 2 ), normal (18.5–24.9 kg/m 2 ), and overweight or obesity (≥ 25 kg/m 2 ) according to the World Health Organization (WHO) BMI classification [ 14]. We categorized maternal education level as low (illiterate, primary school, and junior school), middle (high school, technical school, and junior college), and high (college or higher)[ 15]. We grouped maternal age into younger than 20 years,20–35 years, and ≥ 36 years. Sexually transmitted diseases included syphilis, human immunodeficiency virus,Chlamydia trachomatis
, and gonorrhea. Post-term pregnancy was defined as pregnancy lasting longer than 42 gestational weeks. Preterm pregnancy was defined as pregnancy lasting less than 37 gestational weeks. Maternal medical conditions included maternal diseases (diabetes mellitus, heart and renal disease, thyroid disease, and gestational diabetes mellitus), hypertensive disorders in pregnancy (including gestational hypertension, preeclampsia/eclampsia, chronic hypertension, and chronic hypertension superimposed by preeclampsia/eclampsia), sexually transmitted disease, history of miscarriage or stillbirth, and conception by assisted reproductive technology. Placental or cord abnormalities included placenta previa, placenta abruption, and prolapse of cord. Fetal conditions included preterm and low birth weight.Data extraction and management
Depending on the annual delivery volume, 5–10 consecutive weeks were randomly chosen in a 12-month period as the study window. Within the chosen weeks, all births delivered at 24 completed weeks of gestation or more or a birth weight of ≥ 500 g were included. Additionally, medical records and extracted information on maternal sociodemographic characteristics, pregnancy and labor complications, pregnancy and medical histories, and perinatal outcomes were retrieved by trained staff . A data extraction protocol and a manual of operation were developed to guide data extraction. The staff ,mostly midwives and nurses at the labor and delivery unit,were trained by senior professionals. A data coordination center was established, which was responsible for establishment, maintenance, and management of the database, investigators’ training, coordination among hospitals, and quality control of the data. The data manager reviewed the completed data extraction forms for completeness before they were entered into the database. The data management system was programmed with built-in logic checks to validate the consistency of the related variables and plausible values. A detailed description on sampling and data management has been published elsewhere [ 15].
Ethical approval
This study was approved by the Ethics Review Board of the Xinhua Hospital Affiliated to the Shanghai Jiao Tong University School of Medicine (XHEC-C-2015-006), the WHO Research Ethics Review Committee (HRP Study A65899),and participating hospitals. Because only anonymous clinical information was collected, no individual informed consent was obtained.
Statistical analysis
The 2016 China Statistical Year book provided the number of deliveries in each province [ 12]. The annual number of births in each province was stratified by hospital levels. Each birth was assigned a weight based on the inverse probability weighting, taking into account the number of births in the province with the same hospital level and the number of records reviewed in the hospital with the same hospital level[ 14]. We used multivariable logistic regression to examine the relationships between low Apgar scores and maternal,fetal, and placental conditions. We reported the crude odds ratio (OR) with 95% confidence interval (CI) and adjusted OR controlling for maternal age, race, education, parity, prepregnancy BMI, previous miscarriage or stillbirth, hospital type (maternity hospital and general hospital), and hospital levels (secondary hospital and tertiary hospital). Multiple births were included in the sample.
We further performed correspondence analyses among neonates with Apgar scores < 7 to explore the relationship between risk factors and geographical regions. The population attributable risk percentage (PAR%) [ 16] was calculated for each region-specific risk factor to assess the proportion of low Apgar scores that could be potentially prevented if risk factors were removed. The PAR% was interpreted in this study as the percent incidence of Apgar score < 7 in the population that would be removed if the disease conditions(e.g., hypertensive disorders in pregnancy) were eliminated.We used SPSS version 22.0 (IBM, Somers, NY) for all the analyses.
Results
The overall incidence of low Apgar score in China
A total of 75,132 births were included in the Survey. We excluded 1440 births with unknown fetal outcomes, 1007 births with missing Apgar scores at 5 minutes, and 612 stillbirths, leaving 72,073 live births for the final analysis(Fig. 1). There were 320 neonates who had a 5-minute Apgar score below 7, giving a weighted rate of 3.9/1000 live births.A total of 116 neonates had 5-minute Apgar scores below 4,giving a weighted rate of 0.8/1000 live births.
The incidence of low Apgar scores differed by geographic region
There was a substantial difference in the incidence of Apgar score < 7 by geographic region (Fig. 2). The highest incidence of low Apgar score was found to be in Northeast China (10.9/1000 live births), followed by Northwest China (6.9/1000 live births), Southwest China (6.5/1000 live births), North China (4.7/1000 live births), Central China(3.7/1000 live births), South China (3.6/1000 live births),and East China (2.3/1000 live births).
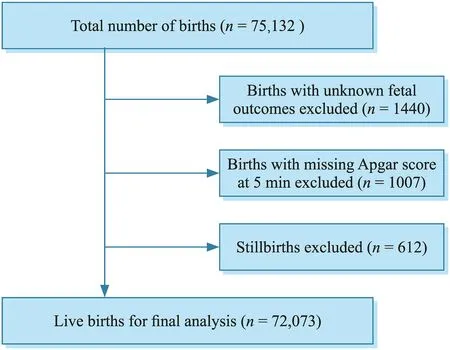
Fig. 1 Flow chart of this study
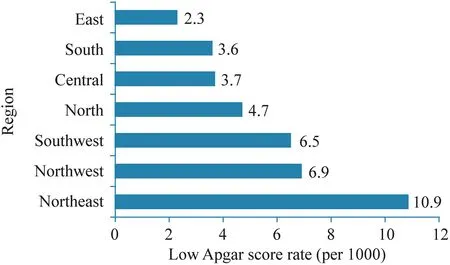
Fig. 2 Incidence of low Apgar scores (weighted) by region for all live births in China from 2015 to 2016
The correspondence analysis of low Apgar score between risk factors and geographical regions in China
Several risk factors were associated with low Apgar scores(shown in Supplementary Table 1); there was a substantial difference in the incidence of risk factors by geographic region (shown in Supplementary Table 2), indicating that the variation in the incidence of low Apgar scores among Chinese regions may be associated with the variation in the incidence of risk factors by geographic region. Hence, we performed correspondence analyses among neonates with Apgar scores < 7 to explore the relationship between risk factors and geographical regions. Fetal, placental, and cord factors related to low Apgar scores do not seem to show regional specificity. However, maternal and obstetric factors related to low Apgar scores show regional specificity, such as Bishop score < 7, premature rupture of membranes (PROM), pre-pregnancy underweight, hypertensive disorders in pregnancy, advanced maternal age, infants born on holidays, and infants born between 0:00 a.m. and 7:59 a.m.. Bishop score < 7 and PROM were major contributors to the low Apgar score in Central and Northeast China;pre-pregnancy underweight was a key risk factor in North and Northwest China; hypertensive disorders in pregnancy,advanced maternal age, and infants born on holidays were major contributors in Southwest China; infants born between 0:00 a.m. and 7:59 a.m. were a significant risk factor in East China (Fig. 3, Supplementary Table 3). The PAR% for each region-specific risk factor was shown in Fig. 4.
Discussion
In this nationwide study, we found that the incidence of 5-minute Apgar score < 7 was 3.9/1000 live births in China;the highest incidence of low Apgar score was found to be 10.9/1000 live births in Northeast China. The correspondence analyses indicated that maternal and obstetric factors were the major region-specific risk factors.
As a developing country, China appears to have a low incidence of 5-minute Apgar score < 7, even lower than some developed countries for which national data are available [ 11]. In the United States, the overall proportion of Apgar score < 7 was 19 per 1000 live births [ 9]. Twentythree countries or regions provided data on Apgar at 5 minutes in Europe, covering 2,183,472 live births, and Apgar scores < 7 ranged from 3 to 24 per 1000 live births across countries [ 11]. This may be attributable to the country’s health policy. To effectively reduce child disability and mortality, China placed a high priority on strengthening the neonatal resuscitation capability of healthcare providers and transferring the majority of high-risk women to tertiary hospitals for better perinatal care. For example, the Chinese Ministry of Health launched the first phase of national implementation of the Neonatal Resuscitation Program, in collaboration with the American Academy of Pediatrics and the Johnson and Johnson Pediatric Institute, in 2004 [ 17].In 2007, the China–Australia Health and HIV/AIDS Facility provided training to provincial, prefecture, and county hospitals, and achieved high levels of coverage for perinatal staff , including obstetricians, pediatricians, and midwives[ 18]. Thus, the Neonatal Resuscitation Program may have prevented many depressed neonates from asphyxia, thus decreasing the incidence of asphyxia.

Fig. 3 Correspondence analysis of low Apgar scores between risk factors and geographical regions in China. PROM premature rupture of membranes

Fig. 4 The population attributable risk percentage for each regionspecific risk factor. a A population attributable risk percentage for low Apgar scores according to risk factors in Central and Northeast China; b population attributable risk percentage for low Apgar scores according to risk factors in North and Northwest China; c population attributable risk percentage for low Apgar scores according to risk factors in Southwest China; d population attributable risk percentage for low Apgar scores according to risk factors in East China. PROM premature rupture of membranes
Despite the low incidence of low Apgar scores, a significant variation among Chinese regions was observed, from 2.3/1000 live births in East China to 6.9/1000 live births in Northwest China and 10.9/1000 live births in Northeast China. Although we acknowledge the considerable reach and effectiveness of the resuscitation training intervention, the quality of instruction and availability of equipment and supplies varied among the facilities, which may hamper the possibility of putting education into practice [ 19]. Differences in training quality might have resulted in the variation of the incidence of low Apgar scores among the Chinese regions.
Moreover, the risk factors for low Apgar scores, especially maternal and obstetric factors, varied by geographic region, which might partly explain the variation in the incidence of low Apgar scores. Thus, targeted strategies are needed to tackle the low Apgar score problem at the local level. In addition to resuscitation training, region-specific strategies, such as changing lifestyle patterns, controlling for underlying conditions, and improving allocation of medical resources, may control region-specific risk factors, thereby reducing the incidence of low Apgar scores in specific regions. For example, in Central and Northeast China, reducing the incidence of Bishop score less than 7 would lead to a reduction of incidence of low Apgar scores by 50.65%; reducing the incidence of PROM would lead to a reduction in the incidence of low Apgar scores by 16.86%. In North and Northwest China, reducing the incidence of prepregnancy underweight would lead to a reduction in the incidence of low Apgar scores by 62.92%. Thus, preventing prepregnancy underweight during preparation for pregnancy in North and Northwest China, such as changing lifestyle patterns, deserves more attention to decrease the incidence of low Apgar scores. In Southwest China, reducing the incidence of advanced maternal age would lead to a reduction in the incidence of low Apgar scores by 51.77%; reducing the incidence of hypertensive disorders in pregnancy would lead to a reduction in the incidence of low Apgar scores by 74.47%. Hence, more attention should be paid to highrisk factors for hypertensive disorders in pregnancy to be screened, predicted, and prevented in pre-pregnancy, early pregnancy and at any stage of first visit in Southwest China.The care of woman at risk for preeclampsia starts with preconception counseling followed by prevention, and treatment to reduce the incidence of poor pregnancy outcomes. In East China, reducing the incidence of infants born between 0:00 a.m. and 7:59 a.m. would lead to a reduction in the incidence of low Apgar scores by 80.44%. The population was lager in East China than other regions. Thus, personnel resources might be short between 0:00 a.m. and 7:59 a.m.in East China. This may suggest that personnel resources(qualitatively or quantitatively) may be a factor of importance. Additionally, monitoring of pregnant women during this period in East China may be enhanced to prevent low Apgar scores.
Thus, strengthening the neonatal resuscitation capacity is critical to decreasing the incidence of asphyxia, and focusing on region-specific maternal and obstetric factors during pregnancy can provide a new strategy to reduce the burden of low Apgar scores.
Limitations
Our study had some limitations. First, a low Apgar score may not be adopted alone to diagnose asphyxia because there may be other causes of this depression at birth, such as drugs, trauma, infections, and hypovolemia. Acidemia can provide more specific evidence of intrauterine hypoxia.However, the information on gasometry tests was not recorded in patients with low Apgar score in some hospitals;thus, it cannot be used in the study. In addition, we did not have data on the Apgar score at 1 minute. However, evidence shows that a low Apgar score at 1 minute is often caused by a temporary depression, whereas low 5-minute Apgar scores usually imply complications of clinical importance and have greater predictive performance than the Apgar score at 1 minute [ 20, 21]. Thus, investigating the 5-minute Apgar score may be as close as we can come to “asphyxia”in the study. Second, since we did not have the individual components of each Apgar score, we were unable to determine what risk factor was strongly associated with which individual component of the resultant Apgar score.In conclusion, to the best of our knowledge, our study is the first nationwide study of Apgar scores in China. We found that there was a substantial difference in the incidence of low Apgar scores by geographic region. We also identified region-specific risk factors for low 5-minute Apgar scores. Strategies based on regional characteristics and risk factors should be considered to further reduce the burden of low Apgar scores in China.
Supplementary Information
The online version contains supplementary material available at https:// doi. org/ 10. 1007/ s12519- 021- 00497-y.Author contributions
WYW and CY contributed equally to the study.They prepared an analytical plan, analyzed and interpreted data, and drafted the initial manuscript. MYH and ZJW involved in data collection. SK conceived and designed the study. ZYJ and ZJ conceived and designed the study, interpreted the data and results, and revised the manuscript. All authors commented on the manuscript, approved the final manuscript as submitted and agree to be accountable for all aspects of the work.Funding
This study was supported by the Shanghai Municipal Health Commission (GWIII-26, GWV-10.1-XK07, 2020QXJQ01).Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.Declarations
Ethical approval
This study was approved by the Ethics Review Board of the Xinhua Hospital Affiliated to the Shanghai Jiao Tong University School of Medicine (XHEC-C-2015-006), the World Health Organization (WHO) Research Ethics Review Committee (HRP Study A65899),and participating hospitals. Because only anonymous clinical information was collected, no individual informed consent was obtained.Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conflict of interest to declare. World Journal of Pediatrics2022年2期
World Journal of Pediatrics2022年2期
- World Journal of Pediatrics的其它文章
- Jacobsen syndrome with bilateral periventricular white matter lesions
- Diagnostic performance of serum interleukin-6 in pediatric acute appendicitis: a systematic review
- Association between HLA alleles and sub-phenotype of childhood steroid-sensitive nephrotic syndrome
- Variations in length of stay among survived very preterm infants admitted to Chinese neonatal intensive care units
- Ursodeoxycholic acid prevention on cholestasis associated with total parenteral nutrition in preterm infants: a randomized trial
