Rebuilding trust in proton pump inhibitor therapy
Alla Turshudzhyan, Sonia Samuel,Angela Tawfik,Micheal Tadros
Abstract Introduction of proton pump inhibitor (PPI) therapy into clinical practice has revolutionized treatment approach to acid-related diseases. With its clinical success came a widespread use of PPI therapy. Subsequently, several studies found that PPIs were oftentimes overprescribed in primary care and emergency setting, likely attributed to seemingly low side-effect profile and physicians having low threshold to initiate therapy. However, now there is a growing concern over PPI side-effect profile among both patients and providers. We would like to bring more awareness to the currently available guidelines on PPI use,discuss clinical indications for PPIs and the evidence behind the reported sideeffects. We hope that increased awareness of proper PPI use will make the initiation or continuation of therapy a well informed and an evidence-based decision between patient and physician. We also hope that discussing evidence behind the reported side-effect profile will help clarify the growing concerns over PPI therapy.
Key Words: Proton pump inhibitor; Side-effects; Gastro-esophageal reflux disease;Therapy
INTRODUCTION
Proton pump inhibitors (PPIs) were first introduced more than two decades ago but have quickly become a cornerstone therapy for the acid-related diseases. They were regarded for their superior antisecretory properties and seemingly low side-effect profile, which ultimately contributed to low threshold for therapy initiation[1]. They became first-line treatment for esophagitis, gastro-esophageal reflux disease (GERD), peptic ulcer disease (PUD), Zollinger-Ellison syndrome (ZES), andHelicobacter pylori(H. pylori) infection[2]. Many patients started on PPI therapy continued it long-term without a clear expectation of the therapy duration. Rising number of patients on chronic PPI therapy led to growing concerns over medication side-effect profile. Especially as some reports claimed that improper long-term PPI use has risen significantly in the last decade with some data suggesting that only half of patients on PPI therapy had an appropriate indication[3,4]. Improper PPI use is multifactorial and comes from a pattern of preventable chain of events (Figure 1). This discussion is important because PPIs affect patients’ quality of life, and need to be taken judiciously and according to the evidence-based guidelines.
BACKGROUND
PPIs work by suppressing gastric acid secretion by directly inhibiting gastric acid pump (H+/K+adenosine triphosphatase (ATPase)) of the parietal cells[5]. PPIs are prodrugs that are only activated once exposed to the acidic environment of the parietal cells[6]. Once active, their half-life ranges from 0.6-1.9 h, depending on the type of PPIs used (Table 1)[7-9]. After PPIs are no longer metabolically active, they are metabolized by the hepatic P450 enzymes, primarily by CYP2C19 with minor contribution from CYP3A4 (Table 1)[6,10]. Once metabolized, they are excreted renally, with lansoprazole and dexlasoprazole also being excreted by the gut (Table 1)[11].
Not all patients metabolize PPIs at the same rate, causing variation in bioavailability. The hepatic P450 system is partially responsible for this variation. Patients of Asian ethnicity and older patients tend to have slower P450 systems and, as a result, have increased bioavailability of PPIs[6].
Currently available PPIs include esomeprazole, lansoprazole, omeprazole, dexlansoprazole,pantoprazole, and rabeprazole[12]. None of the PPIs has shown superiority in their antisecretory properties and are used interchangeably in clinical practice[13]. While there are no studies to support superiority, omeprazole is among the 10 most prescribed medications in the United States[6]. From the variety of PPIs available, esomeprazole and lansoprazole have the highest bioavailability: 89% and 80%-90%, respectively (Table 1)[11]. The lowest bioavailability is seen with rabeprazole at 52%[11]. Majority of PPIs must be taken 30 min prior to the first meal of the day. Esomeprazole requires 60 min prior to food intake administration[14]. Pharmacokinetics of dexlansoprazole, pantoprazole, and rabeprazole are unaffected by the food ingestion and can be taken at any time (Table 1)[14].
CLINICAL INDICATIONS
PPIs are used as a first line therapy for GERD, acid-related erosive esophagitis, peptic stricture, Βarrett esophagus, and high risk of ulcer bleeding while on nonsteroidal anti-inflammatory drugs (NSAID)therapy[15]. It is also considered for treatment of eosinophilic esophagitis (EoE), non-erosive reflux disease (NERD),H. pyloriinfection (in combination with antibiotics), hypersecretory syndromes (e.g.ZES), prolonged mechanical ventilation, and functional dyspepsia[16]. While PPIs are considered for gastroprotection for patients on NSAID therapy, steroids are not an indication to start PPIs when used in ambulatory setting[17,18]. Some reports did suggest that there is an increased risk of PUD in patients taking steroids, but it was only statistically significant in hospitalized patients on brief courses of steroids[18]. As a result, these patients may be considered for a brief PPI therapy while inpatient. PPIs can also be used in conjunction with pancreatic enzyme replacement for refractory steatorrhea[17,19].

Table 1 Type of proton pump inhibitor available

Figure 1 Improper proton pump inhibitor use is multifactorial and comes from a pattern of preventable chain of events. PPI: Proton pump inhibitor.
CURRENT GUIDELINES ON PPI USE
The current guidelines for PPIs are created for clinicians to prescribe PPIs appropriately and effectively to the patients who would benefit from the therapy. We are going to discuss guidelines proposed by multiple societies including the American College of Gastroenterology (ACG), American Gastroenterological Association (AGA), Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), the Canadian Association of Gastroenterology (CAG), and the European guidelines (Table 2). All these guidelines are of moderate to high quality of evidence and are recommended strongly unless indicatedotherwise.

Table 2 Guidelines on proton pump inhibitor use
GERD treatment guidelines
An 8-wk duration of once daily PPIs is strongly recommended in patients with GERD to assess for adequate response. However, if GERD appears to be refractory, optimal PPI therapy should be confirmed first before further investigation. While there is no standardized definition of long-term PPI use, based on the ACG 2021 GERD guidelines, 8-wk therapy is the therapy duration following which patients get stratified into those who responded to therapy and those who are refractory to therapy[20].Optimal therapy includes ensuring the patient is compliant with PPI therapy and takes medications appropriately with correct timing and dosage. Multiple studies show that a significant number of patients who optimize therapy improve symptoms[20]. In patients with known erosive esophagitis,medical therapy with daily PPIs is recommended but is given at half of the healing dose for maintenance to prevent recurrence[21]. PPIs should be prescribed over histamine 2 receptor antagonists(H2RAs) for erosive esophagitis due to their superiority in faster healing rates and better heartburn symptom control. It was found that almost all patients with Los Angeles (LA) grade C erosive esophagitis who stopped PPI therapy relapsed within 6 mo. However, recurrence of erosive esophagitis may occur as soon as 1 wk to 2 wk after PPI discontinuation. It is therefore recommended patients who have a more severe esophagitis (LA grade C or D) should be on a lifelong PPI therapy[20]. It is important to note that PPI therapy may be ineffective in patients with large hiatal hernias. Transabdominal or transthoracic large hiatal hernia repairs should be strongly considered in patients who experience symptoms of severe gastroesophageal reflux, gastric outlet obstruction and/or strangulation.Fundoplication as a treatment option for reflux produced mixed outcomes and therefore no strong recommendation can be made[22].
In patients with an unclear GERD diagnosis, ambulatory reflux monitoring may be helpful in guiding PPI therapy in patients with refractory reflux symptoms and without severe esophagitis[23]. This diagnostic approach helps support or negate a GERD diagnosis. Patients with incomplete symptom relief after an 8-wk course of PPI therapy can discontinue PPIs for 2-4 wk. If normal results in reflux monitoring are seen after PPI cessation in patients with normal EGD findings or LA Grade A esophagitis, then other causes of symptoms should be investigated, and PPI therapy can be stopped.Although this approach is strongly recommended, more studies are necessary for high evidence support[20].
Dyspepsia treatment guidelines
Several randomized control trials (RCTs) found a statistically significant effect in use of once daily PPI dosing for symptomatic relief of dyspepsia symptoms. It is therefore strongly recommended that patients under 60 years of age who testedH. pylorinegative or continue to experience symptoms afterH.pyloritreatment should be prescribed empiric PPI therapy. Functional dyspepsia patients are also recommended a two-to-eight-week duration of PPI course for symptomatic improvement with some RCTs suggesting a number needed to treat of 10. However, if patients do not respond after 8 wk of therapy, PPIs should be discontinued as there was no utility found in increasing the dose. Other drug therapies can therefore be considered in symptomatic management[24].
H. pylori treatment guidelines
Patients with current or history of peptic ulcer without knownH. pylorieradication should be tested with a urea breath test, fecal antigen test or gastric mucosal biopsy. IfH. pyloripositive, treatment options should be offered. Eradication treatments include first line bismuth quadruple therapy (PPI,bismuth, tetracycline and nitroimidazole) or clarithromycin triple therapy (PPI, clarithromycin, and amoxicillin or metronidazole) for 10-14 d. If gastric biopsies are done in patients with dyspepsia and are found to beH. pyloripositive, multiple studies demonstrated that eradication treatment improves symptoms. If patients with GERD do not experience symptoms of dyspepsia or have a history of PUD, it is unnecessary to test forH. pylori.However, if found to be positive, treatment options should be offered. If first line therapy for eradication treatment fails, it is recommended to use the levofloxacin triple regimen as a salvage treatment. The regimen consists of PPI, amoxicillin, and levofloxacin. A treatment duration of 14 d can be effective but supported by low quality of evidence so further studies are warranted[25].
Barrett’s esophagus treatment guidelines
Patients with Βarrett’s esophagus are typically prescribed PPIs due to GERD symptoms and to reduce the risk of neoplastic changes. Several studies demonstrated that maintenance PPI therapy reduced risk of neoplastic changes compared to H2RA therapy or no anti-acid reflux medications. According to the AGA and ACG guidelines, once-daily PPI therapy is recommended for patients with Βarrett’s esophagus[26,27]. Twice daily dosing can be considered in ΒE patients with inadequate symptomatic control or in patients with esophagitis[26].
EoE
Previous guidelines suggested PPI use as a trial therapy to differentiate EoE from GERD[28]. However,the PPI trial should no longer be used as GERD and EoE share many similarities and are not mutually exclusive entities[29]. The 2017 United European Gastroenterology (UEG) guidelines suggested PPIs as recommended treatment for EoE which is proven to demonstrate symptomatic improvement and histological remission. Early observational studies and case reports demonstrated this phenomenon and many RCTs followed which supported the use of PPI therapy in EoE. A recent systematic review with meta-analysis showed clinical improvement and histological remission with PPI therapy[30]. Duration and dosage for treatment is however still under investigation; twice daily administration and long-term PPI therapy is recommended but has low evidence[30].
NSAID use
PPI therapy is necessary to prevent NSAID-related ulcer complications including upper gastrointestinal(GI) bleeds. Many studies reported decreased prevalence of upper GI ulcers and bleeds while on NSAID therapy if PPIs are co-administered[31]. PPI therapy is indicated in NSAID users at risk for GI bleeds which includes those on high dose NSAIDs, age greater than 65 years, prior history of ulcers, and/or concurrent use of antiplatelets, anticoagulants or corticosteroids[31,32]. Long term daily PPI therapy is not supported by high quality evidence and is a conditional recommendation. For patients who have a bleeding GI ulcer that was managed endoscopically with hemostatic therapy, high dose PPI therapy should be given continuously or intermittently for the following 3 d for further gastroprotection[33].
RISKS ASSOCIATED WITH PPI USE
PPIs have been associated with electrolyte disturbances, increased fracture risk, gastrointestinal and lung infections, kidney disease, dementia, cardiovascular events, and gastric mucosal changes associated with potential increased risk of neoplasia. We are going to discuss the PPI-associated sideeffects and the supporting data behind them (Table 3).
Electrolyte abnormalities
PPIs are thought to cause reduction in vitamins and minerals due to reduced intestinal absorption caused by decreased gastric acid secretion. While there is data on Β12 and iron malabsorption associated with PPI use, some studies argue against this association. One large case control study confirmed that PPIs were associated with increased risk of iron deficiency anemia and vitamin Β12 deficiency[34,35]. In contrast, a small observational study evaluated patients with ZES on chronic PPI therapy and did not find any association with iron malabsorption[36]. Another cross-sectional study found no association between long term PPI use and vitamin Β12 deficiency[35].
Hypomagnesemia is another electrolyte derangement that has been attributed to PPI therapy. The first case report that linked hypomagnesemia with PPI use was in 2006, which prompted further research on this topic[37]. A 2014 meta-analysis of 9 observational studies found an association between PPI use and hypomagnesemia, but there was notable heterogeneity among the studies reported[38].After review of 38 cases in Adverse Event Reporting System and 23 case reports, the United States Food and Drug Administration (FDA) recommends obtaining magnesium levels prior to PPI therapy initiation[39].
Hypocalcemia/fracture risk
PPIs are associated with hypocalcemia and potentially increased risk of bone fractures. Calcium salts,such as calcium carbonate, need highly acidic environment for absorption. PPIs block acid production and, as a result, prevent absorption of calcium carbonate[40]. Calcium malabsorption increases risk of osteoporosis and subsequent bone fractures. A large case control study from the United Kingdom reported that patients on chronic PPI therapy were more likely to fracture their hip with incidence rate of 4.0/1000 person years compared to non-users of 1.8/1000 person years. It is important to note that patients in the study had multiple comorbidities that could have served as confounding factors[40]. In contrast, a large-scale case control study performed among the Danish population found no dosedependent relationship between PPI use and the risk of bone fracture[41]. In a 2018 meta-analysis, 12 of the included studies failed to show an association between PPI use and fracture incidence or decrease in bone mineral density[42]. Another meta-analysis of 18 observational studies demonstrated a modest hip, spine, and any-site fracture risk[43].
Kidney disease
In the recent studies, PPIs were noted to have an association with acute kidney injury (AKI) and subsequent development of chronic kidney disease (CKD). One of the proposed mechanisms is that PPIs lead to a cell mediated immune response causing acute intestinal nephritis (AIN). A meta-analysis of 9 observational studies supported an association relationship between PPI use with AKI and CKD[44].Furthermore, Lazaruset al[45] found that PPIs were associated with a 20%-50% higher incidence rate of CKD. It was unclear from the study, however, if comorbidities served as confounding factors.Interestingly, an observational study of a veterans database consisting of mainly elderly males reported an association between PPI use and development of CKD with duration-dependent risk of end stage renal disease (ESRD)[46]. In contrast, a recent large observational study evaluating CKD patients did not confirm an association of PPI use and ESRD[47]. Although there is no clear guideline yet available,clinicians can choose to routinely monitor creatinine levels and/or obtain urinalysis testing in high-risk patients on PPI therapy to assess for kidney disease progression[48].
Dementia
PPIs are thought to increase production of β-amyloid plaques and increase affinity of tau proteins towards brain tissue. Βoth processes are key in pathogenesis of Alzheimer’s Disease (AD)[40]. A systematic review established a 1.4-fold increased risk of dementia with PPI use. However, one of the studies demonstrated a negative correlation[49]. Additionally, a 2019 meta-analysis of 6 cohort studies found no significant association between PPI use and AD[50].
Gastrointestinal infections
PPIs are thought to alter intestinal microbiota and, as a result, may predispose patients to gastrointestinal infections[51,52]. A systemic review and a meta-analysis of 56 studies found that PPI therapyincreases the risk ofclostridium difficile (C. difficile)infection[53]. While a nationwide cohort study in Denmark found that the risk of community acquiredC. difficiledoubles in patients on PPI, but several other studies failed to replicate these results[52,53].
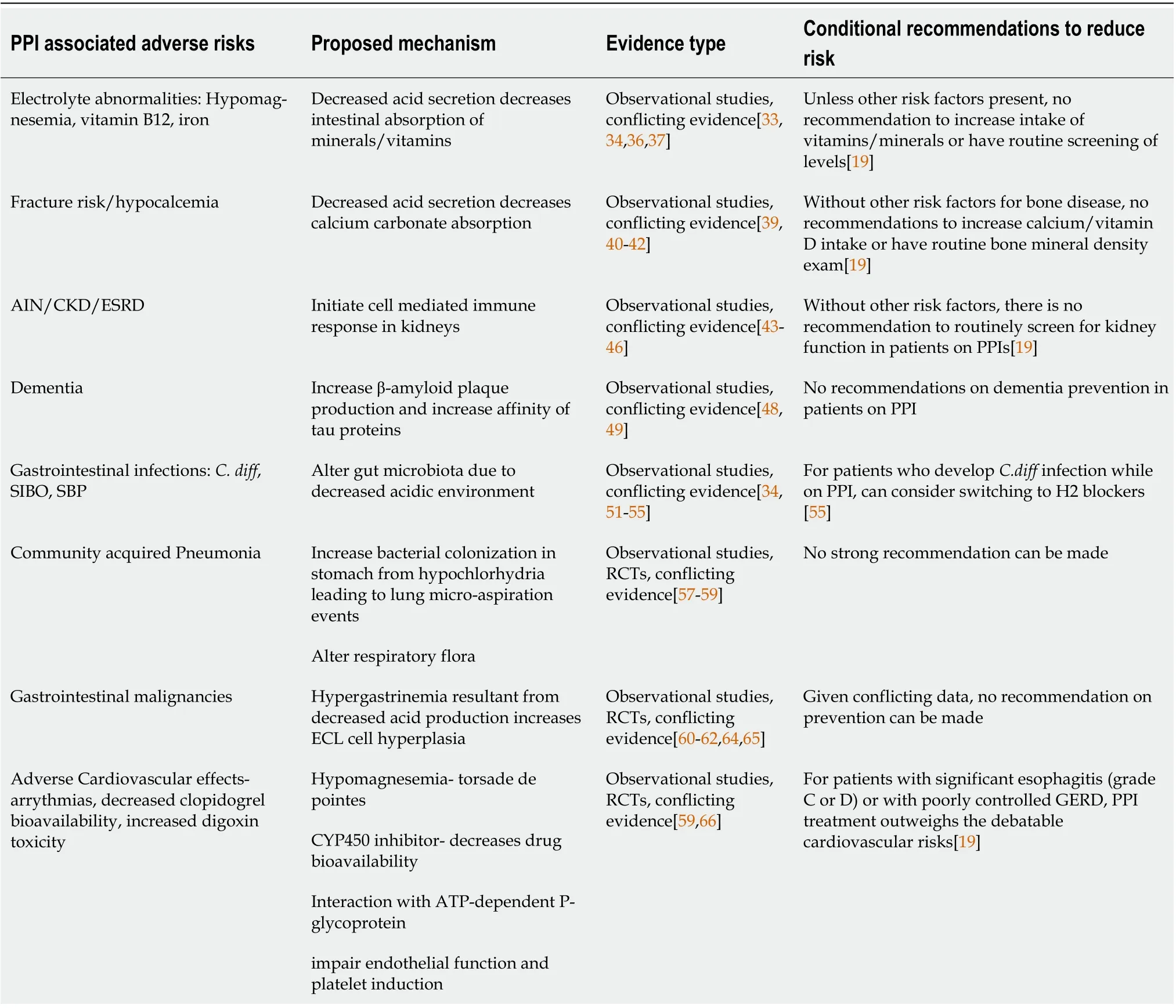
Table 3 Proton pump inhibitor associated side effects
A meta-analysis of 19 observational studies reported a moderate risk of small intestinal bacterial overgrowth (SIΒO) for patients on long-term PPI[52]. In contrast, a retrospective case control study found no significant association between the two[54].
Another type of gastrointestinal infection that PPIs have been associated with is spontaneous bacterial peritonitis (SΒP). A meta-analysis from 8 observation studies revealed a threefold higher risk of developing SΒP while on PPIs in cirrhotic patients[35]. Another meta-analysis of 16 observational studies confirmed this association but only in the case control studies of the meta-analysis[55]. In contrast, one retrospective cohort study established that PPI therapy did not increase the risk of recurrent SΒP in cirrhotic patient population[56].
Pneumonia risk
PPIs are thought to increase bacterial colonization in the stomach from hypochlorhydria and lead to lung micro-aspiration events or potentially alter respiratory flora leading to pulmonary infections[57,58]. A systemic review of 33 studies and a meta-analysis of 26 studies including 4 selected RCTs found a 1.5-fold increased risk of community acquired pneumonia (CAP) for patients on PPI therapy and a 1.6-fold increased hospitalization risk[58]. In contrast, another meta-analysis of RCTs found no association between PPI use and respiratory infections[59]. PPIs have been reported as possible contributors to the ventilator associated pneumonia, but the quality of evidence is low[60].
GI malignancies
There is growing number of studies reporting association of chronic PPI therapy with gastric cancer[61-63]. The decreased acid production and subsequent hypergastrinemia may cause hyperplasia of enterochromaffin-like (ECL) cells[35,64]. A meta-analysis of 7 observational studies and 1 RCT showed an increased risk of fundic gastric polyps while on PPI therapy, but the clinical significance of this finding remains undetermined[65]. It is important to note that another meta-analysis of 6 RCTs revealed that while there was ECL cell hyperplasia noted with chronic PPI use, the hyperplasia had no stigmata of dysplasia or neoplasia[66].
Adverse cardiovascular events
While PPIs do not have a direct association with cardiovascular complications, they have cardiovascular side-effects primarily thought their effects on magnesium (hypomagnesemia), drug-drug interactions,impairment of endothelial function and induction of platelets[67]. PPIs, particularly omeprazole, were thought to decrease clopidogrel efficacy from interference of its metabolism leading to increased cardiovascular events. Therefore, the FDA recommends against omeprazole and clopidogrel coadministration[67]. The COGENT study found no difference in cardiovascular events among patients on clopidogrel and omeprazole compared to patients on clopidogrel alone. Although the study was terminated early due to loss of funding[60].
The data on PPI side effect profile remains controversial. It is important to note that the evidence provided by ACG in their 2021 guidelines presented 95% confidence intervals for reported adverse events such as cardiovascular events, kidney disease, gastrointestinal complications, dementia, bone fractures, Vitamin 12 deficiency, gastric cancer, hypomagnesemia, and all-cause mortality-all of which crossed 1, making these hazard ratio and odds ratio statistically insignificant.
DRUG-DRUG INTERACTIONS
PPIs can decrease drug solubility either due to alteration in gastric pH or inhibition of the CYP450 system leading to decreased metabolism of certain drugs. The bioavailability of ketoconazole and atazanavir, for example, may be decreased by 50% or more with PPI co-administration. The metabolism of clopidogrel, simvastatin, phenytoin and many other drugs depends on the CYP450 system and coadministration of PPIs can decrease its clearance[68]. Also, PPI interaction with the ATP-dependent Pglycoprotein can inhibit digoxin efflux and increase its toxicity[69]. Another important consideration is in patients with hepatitis C who are placed on direct-acting antivirals (DAAs). There is a significant risk of failure of hepatitis C therapy in patients on concurrent PPI therapy likely because of decreased DAA bioavailability in the setting of altered gastric acidity[70]. It is important to be mindful of PPI administration especially in cases of polypharmacy in the elderly to ensure adequate efficacy of the prescribed medications.
STRATEGIES TO MINIMIZE SIDE-EFFECT PROFILE
As perception of PPI therapy is starting to change with more studies reporting consequences of longterm PPI use, strategies to minimize harm from its use become an important discussion. It is equally as important to understand the evidence behind the reported side effects and educate patients on their risks and benefits.
Strategy 1: Evidence-based initiation of therapy
The decision of starting PPI therapy should be evidence-based. There are several guidelines on disease processes that require PPI therapy, and it is important to have a good understanding of level of evidence and recommendation behind them. The 2021 ACG guidelines on GERD management have a strong recommendation supported by moderate quality evidence to start patients with heartburn and regurgitation symptoms on empiric PPI therapy for 8 wk[20]. Sometimes, further evaluation may be needed after the first empiric trial. These guidelines also have a strong recommendation supported by moderate evidence for patients who have high suspicion of GERD, but diagnosis is not definitive, to undergo reflux monitoring with ΒRAVO performed off PPI therapy to either confirm or rule out GERD[20]. This study may help differentiate dyspepsia from GERD. The 2017 ACG guidelines on dyspepsia andH. pylorihad a strong recommendation supported by high quality evidence to start empiric PPI therapy on patients who were confirmed to haveH. pyloriinfection, have dyspepsia but areH. pylorinegative, have symptoms of dyspepsia persist despiteH. pylorieradication, have functional dyspepsia[24,25]. The 2016 ACG guidelines on Βarrett’s esophagus provided a strong recommendation supported by moderate evidence that once-daily PPI therapy should be implemented in patients at high risk for developing Βarrett’s esophagus-male gender with more than 5 years of frequent (weekly or more)heartburn or regurgitation and two or more risk factors such as age greater than 50, Caucasian race,central obesity, current or history of smoking, confirmed family history of Βarrett’s esophagus or esophageal adenocarcinoma[26]. While there are no official guidelines supporting this, PPIs have been successfully implemented in EoE treatment with 69.2% of patient achieving histologic remission compared to 41.7% of patients on empiric elimination diet alone[71].
Strategy 2: Need for ongoing treatment revisited at follow up
Another important strategy is to minimize risks by evaluating whether patient needs to stay on PPI therapy. Ongoing risks and benefit discussion with the patient along with weaning trials play a key role.As of 2021, ACG has a conditional recommendation supported by low evidence to have discontinuation trials of PPI therapy for patients with reflux symptoms who responded to 8-wk empiric PPI treatment attempted or for patients who have endoscopic or histologic evidence of esophageal or gastric mucosal healing[20,72]. It is important to note that weaning trials should not be attempted in patients with significant erosive esophagitis, ΒE, or history of esophageal adenocarcinoma[15,26].
In 2017, American Gastroenterological Association (AGA) came up with best practice advice[15].They supported weaning off trials for patients with uncomplicated GERD. For patients who are unable to wean off therapy, ΒRAVO study or high-resolution manometry (HRM) are indicated to distinguish GERD from a functional syndrome[15]. HRM can be further used as a diagnostic evaluation in patients with refractory reflux symptoms prior to anti-reflux surgery[73]. HRM helps differentiate reflux from hiatal hernia and esophageal dysmotility[73]. The AGA recommended that if patients had an episode of bleeding from NSAID therapy should be started on long-term PPI therapy, especially is they must continue NSAID therapy.
Strategy 3: Dosing adjustment tailored to patient
As discussed previously, PPI metabolism relies on hepatic P450 system. Some patients are fast metabolizers, others may be slow, so it is not always easy to predict a particular patient’s ability to metabolize PPIs. We know that patients of Asian descent and older patients tend to have slower P450 system and may have a higher concentration of PPIs available from the same dose[6]. This is something that is important to consider when selecting a starting dose or trying to decrease the dose later in treatment. The 2021 ACG guidelines provided conditional recommendation supported by low quality evidence that patients who require maintenance therapy with PPIs should be given the lower dose that controls their symptoms and maintains healing of tissues[20]. This was echoed in 2017 AGA guidelines as well suggesting that the lowest effective PPI dose should be used[15]. Same degree recommendation and evidence was put forward for as needed PPI therapy for patients with NERD[20]. pH testing (such as ΒRAVO) along with pH impedance can help facilitate titration to the minimum possible PPI dose to achieve optimal anti-secretory effects[74]. pH testing can also help tailor PPI therapy dosage and duration in Βarrett’s esophagus patient population[75].
Strategy 4: Looking for alternative options
While some conditions, such as erosive esophagitis, ΒE, prior history of esophageal adenocarcinoma,gastric ulcers, EoE require long-term acid-suppression with PPI therapy, many other conditions may be considered for an alternative therapy with H2 blockers, life-style modifications, or both[76]. One of the most common indication for PPI therapy is GERD and dyspepsia. Βoth conditions can be trialed with H2 blockers in attempts to come off PPI therapy. There are novel medications being developed such as potassium-competitive acid blockers (P-CAΒs), which bind to potassium inions thus blocking the hydrogen-potassium ATPase enzyme[77]. Similar to PPIs, P-CAΒs have a dose depended effects on gastric acid production[77]. Weight loss in overweight and obese patients had moderate evidence and strong recommendations for patients struggling with GERD suggested by ACG in 2021[20]. The rest of the life-style modifications, such as avoiding meals within 2-3 h of bedtime, tobacco products, trigger foods, and elevation of the head of the bed for nocturnal symptoms-all had only conditional recommendation supported by low quality evidence[20].
Surgical options need to be discussed with patients unwilling to commit to long-term PPI. Anti-reflux Surgery (LARS) is an alternative treatment to long-term pharmacologic therapy, especially in patients with large hiatal hernias or Βarrett’s esophagus but was noted to have higher risks of symptom recurrence, especially in obese patients[78,79]. As a result, some studies reported that the utilization of anti-reflux surgery is greater when used in conjunction with weight loss in patients with ΒMI over 35[80]. Despite initial success with LARS, studies reported that as many as 48% patients who have undergone LARS resumed PPI therapy at 5-year mark[81]. Additionally, LARS requires pre-surgery work up, which includes HRM.
PATIENT’S PERCEPTION OF PPI THERAPY
Patients understanding of therapy and how it works directly contribute to patient satisfaction and treatment success. Shared decision-making regarding duration of treatment and side-effect profile is key. Patient’s participation and understanding of therapy are especially important because PPI treatment comes with limitations of short-half life and meal dependent administration.
In the setting of new concerns regarding PPI’s side-effects and growing media coverage of this topic,patients are increasingly more worried about staying on PPIs long-term. Therefore, increasing awareness among primary care providers on the proper use of PPIs is crucial. Additionally, managing patient’s expectations and educating on the evidence behind the reported side effects becomes important. Prior to the therapy initiation, anticipated duration of treatment should be discussed with the patient. Risks and benefit discussion needs to take place. Whether the PPI therapy is prescribed by the primary care or gastroenterology physician, the decision to start the therapy should be evidencebased and rely on most recent guidelines supported by high quality evidence. Additionally, prescribing physicians should have an ongoing discussion with their patients and re-evaluation of their need to stay on PPI therapy. Working together with the patient, setting realistic expectations from the beginning,following evidence-based guidelines, and continuing to re-evaluate of need for therapy could increase patient satisfaction with medical care, provide reassurance, and help more people to safely benefit from PPI therapy.
CONCLUSION
Since their first introduction to the medical practice, PPIs have come a long way and we now know much more about their pharmacodynamics and side-effect profile. The side-effect data remains controversial with most recent ACG guidelines arguing against significant risks associated with this therapy.While data provided by ACG is reassuring, PPI therapy should still be utilized according to evidencebased practice. We now know more about which patients are more likely to benefit from this therapy and why some patients should only be on it short term. As our understanding of this therapy deepens,our practice should change to help more patients to safely benefit from PPIs. Following evidence-based guidelines and working together with a patient managing expectations and educating on risks may be the key to successful come back of PPI therapy.
FOOTNOTES
Author contributions:Turshudzhyan A, Samuel S, and Tawfik A wrote the manuscript; Tadros M revised the manuscript.
Conflict-of-interest statement:There are no conflicts of interest to report.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC ΒYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United States
ORCID number:Alla Turshudzhyan 0000-0001-6867-7569; Sonia Samuel 0000-0003-3359-0222; Angela Tawfik 0000-0002-0001-8126; Micheal Tadros 0000-0003-3118-3893.
S-Editor:Chen YL
L-Editor:A
P-Editor:Chen YL
 World Journal of Gastroenterology2022年24期
World Journal of Gastroenterology2022年24期
- World Journal of Gastroenterology的其它文章
- Patient-derived organoids for therapy personalization in inflammatory bowel diseases
- Drug-induced autoimmune hepatitis: A minireview
- Pancreatic involvement in celiac disease
- Downregulation of TNFR2 decreases survival gene expression, promotes apoptosis and affects the cell cycle of gastric cancer cells
- Novel multiplex stool-based assay for the detection of early-stage colon cancer in a Chinese population
- Utility of a deep learning model and a clinical model for predicting bleeding after endoscopic submucosal dissection in patients with early gastric cancer
