Non-inclusion of certified herbal medicines in the National Health Insurance Scheme affects patient utilization of the integrated herbal medicine services in Ghana
Anthony Nketia,Emmanuel Nakua,Andrews William Tetteh,Kwesi P.Thomford,Kwame O.Boadu,Ama K.Thomford
1Department of Health Promotion, Education and Disability Studies, School of Public Health, Kwame Nkrumah University of Science and Technology, Kumasi,Ghana.2Department of Epidemiology and Biostatistics, School of Public Health, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana.3Department of Pharmacognosy and Herbal Medicine, University of Cape Coast, Kumasi, Ghana.4Department of Maternal and Child Health, Kumasi South Hospital,Kumasi,Ghana.5Department of Biomedical Sciences,University of Cape Coast,Kumasi,Ghana.
Abstract Background: In 2011, Ghana piloted the integration of herbal medicine services into mainstream health care delivery in selected government hospitals across the country.To date, however, no single certified herbal drug is generally covered by the national health insurance scheme.This study evaluated the implications of out-of-pocket payment for prescriptions on the patronage of herbal medicine units in 3 selected government hospitals within Kumasi Metropolis. Methods: A cross-sectional study on 413 participants was performed using a semi-structured questionnaire. Results: The majority of study respondents were female (54%), and the median age was 35 years.Most participants(83.1%) were aware that herbal medicine was integrated in the mainstream health care system of the country.Regarding the costs of certified herbal drugs, 51.5% of respondents considered them very expensive; 72.1% of the respondents believed that the costs of certified herbal drugs adversely affected the utilization of herbal units at government hospitals, which produced a positive correlation (r = 0.5498).A total of 99.5% of the respondents recommended the inclusion of certified herbal drugs on the national health insurance drug list. Conclusion: This study revealed that the costs of certified herbal medicines negatively affect utilization of herbal units at government hospitals.To improve the utilization of herbal units, certified herbal drugs dispensed at these units must thus be included in the national health insurance drug list.
Keywords:complementary and alternative medicines; herbal medicine; primary healthcare;universal health coverage
Background
Traditional medicine has been practiced for several centuries[1–4].In the past, rural African communities depended solely on the invaluable spiritual and practical skills of traditional medicine (TM) practitioners for healthcare [5, 6].Historically, ancient Pharaonic Egyptian medical practices constituted the oldest documented form of TM.From the beginning of civilization in about 3300 B.C.E.until the Persian invasion in 525 B.C.E.,Egyptian medical practices were comparatively highly advanced, including simple non-invasive surgery, bone setting,and an extensive set of pharmacopoeia in the form of papyri, notably theEbers Papyrus(1500 B.C.E.), which comprised approximately 700 formulas and remedies.Several others were documented around this period.In sub-Saharan Africa, for unknown reasons, little information on African TM practices was recorded until the 19thcentury [7].
The advocacy for the use of TMs by the World Health Organization dates back to 1977 when the World Health Assembly drew attention to the potential of the practice, urging its member countries to utilize healthcare systems to address the gap in access [8, 9].Moreover, theAlma Ata Declarationrecommended that the government prioritize TMs in national drug policies and regulations [8].
TM covers a myriad of health practices, approaches, beliefs, and knowledge on plant-, animal-, and/or mineral-based medicines,manual techniques, and exercises, in addition to spiritual therapies used singularly or in combination with other approaches to achieve well-being.TM practice is considered a socio-cultural heritage in African [10].Ghana is among the few countries in Africa which provide a relatively advanced environment for the practice of TM,with its most predominant form, herbal medicine practice, undergoing marked development.Herbal medicine practices in the country are regulated, a testing regime for products is available, specialized governmental institutions are mandated to support TM through research, and there is a framework for the training of practitioners[11].All these strategies are backed by a national policy directed at improving the quality of healthcare delivered by practitioners [12].The country achieved a significant milestone in 2010 with the establishment of herbal medicine clinics in selected districts and regional hospitals as pilot centers for the integration process.The impact and challenges of this integration model have been extensively examined in different studies [13, 14].
Universal health coverage, as reported by some studies, depends on national health insurance systems or some form of state-sponsored healthcare [15, 16].Utilization of health facilities significantly decreases with increasing out-of-pocket expenditure [17, 18].Thus,national health insurance is a tool for ensuring access to quality healthcare for all strata of society [19, 20].In Ghana, some aspects of conventional healthcare are covered by the National Health Insurance Scheme (NHIS) since 2003; however, this does not apply to herbal medicine services [21].
Under the current scheme of practice for herbal medicine, NHIS coverage is limited to clinics under the domain of the Ghana health service.However, coverage at such facilities is limited to consultancy and laboratory charges.Treatments prescribed at these facilities must be paid out of pocket by the patient.Although socio-cultural compatibility and the perceived safety and efficacy of herbal medicines are key drivers for continuous patronage, health insurance coverage of herbal medicines is essential for equitable access.
This study examined the implications the requirement for out-of-pocket payment of herbal medicines approved for use and how this affected utilization of herbal medicine services in 3 selected government hospitals within the Kumasi Metropolis.
Methods
Study design
A cross-sectional study design was used.The study period was from July to August 2019, and quantitative data collection was employed.
Study site
The study was conducted in the Kumasi Metropolis, specifically, in herbal units at government hospitals employing medical herbalists,i.e., at the following 3 hospitals: Tafo Government Hospital, Suntreso Government Hospital, and Kumasi South Government Hospital.
Study participants
Adult patients (≥18 years) attending the selected herbal units and medical herbalists in charge of the respective herbal units were recruited.
Sampling technique
Cochran’s formula was used to determine sample size [22], i.e., N =Z2P (1 - P)/d2
where N = required sample size; Z = confidence level of standard value (from statistical table); P = estimated proportion of patients with access to health care services at the herbal units of government hospital in Kumasi Metropolis; and d = margin of error (degree of accuracy).
A 95% confidence level with a standard value of 1.96 from statistical table and 5% (P< 0.05) margin of error (degree of accuracy) were used.A previous study showed among all patients who visit government hospitals with herbal medicine units, 42.2% used the services of herbal units [14].Using Cochran’s formula, the required sample size was calculated as follows:
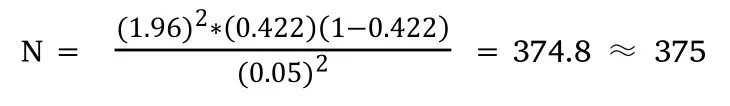
Accounting for 10% non-responders (i.e., 10% of 375 = 37.5 ≈38), 413 (375 + 38) participants were enrolled.The catchment sizes of Tafo Government Hospital, Suntreso Government Hospital, and Kumasi-South Government Hospital are 236,619, 357,886, and 448,097, respectively [14].These figures were used to calculate sample sizes for the respective study areas(Table 1).
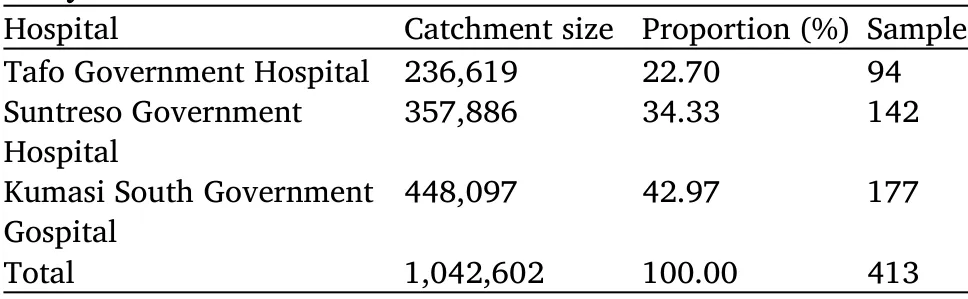
Table 1 Estimated sample size from selected hospitals within the study area
Purposive and convenience sampling were used to select participants meeting the inclusion criteria.Convenience sampling was used because few clients accessed the services of herbal unit per day.Therefore, clients who used the respective herbal unit at the time of the study were included in the study.The inclusion of only one medical herbalist per facility, despite the presence of other healthcare professionals at various hospitals, was a purposive sampling strategy.Medical herbalists were considered the best respondents based on their expertise thus they were able to provide appropriate data for this study, thus medical herbalists were included.Moreover, two sampling techniques were adopted owing to the relative advantages of time and costs inherent to this method of sampling [23].
Ethical approval
All study protocols were reviewed and approved by the Institutional Review Board of Kwame Nkrumah University of Science and Technology (KNUST) - The Committee on Human Research and Publication Ethics (CHRPE/AP/416/19).
Data collection
Primary data were obtained by administering a semi-structured questionnaire to participants.The questionnaire was designed by the principal investigator and was reviewed by the research team.It included variables useful for measuring factors such as socio-demographic characteristics of the respondent, level of knowledge on herbal medicine practice in Ghana, and the implication of the costs of certified herbal drugs on the utilization of herbal units at government hospitals.Respondents completed the questionnaire using a mixture of binary answers, short responses, and selections from a predefined list.
Prior to data collection, informed consent and permission to participate in the study were obtained from each participant.All participants were free to withdraw from the study at any time, and they were free to choose not to answer any particular question.Strict confidentiality of the respondents’ identities was achieved using unique numeric codes with the corresponding personal data being available only to the principal investigator.
Data statistical analyses
After data collection, the questionnaires were reviewed, and responses were coded and analyzed using STATA software version 14.Descriptive statistics including frequencies, percentage distributions,means, and standard deviations were used to describe the sociodemographic characteristics of the respondents.Univariate analysis was used to test the respondents’ knowledge on integrated herbal medicine processes in Ghana.Additionally, the respondents’ratings of the overall costs of certified herbal drugs dispensed at herbal units of government hospitals and its adverse effects on the utilization of the herbal units were analyzed using correlation tests.
Results
Socio-demographic characteristics of study participants
A total of 413 respondents were enrolled in this study, of which 223(54%) were female.Five medical herbalists working in the catchment area facilities were included.The ages of the respondents ranged from 18 to 82 years, with a median age of 35 years (25th and 75th percentile 27 and 49 years, respectively) and a mean age of 38.73 years (standard deviation 15.23).Most respondents (152; 36.8%) had secondary education as their highest educational background.The majority of the respondents (349; 84.5%) were Christians; 231(55.9%)of the respondents were married.The major occupation of the respondents was trading, however, many of them also worked in public service.A detailed description of the respondents’sociodemographic characteristics is shown in Table 2.
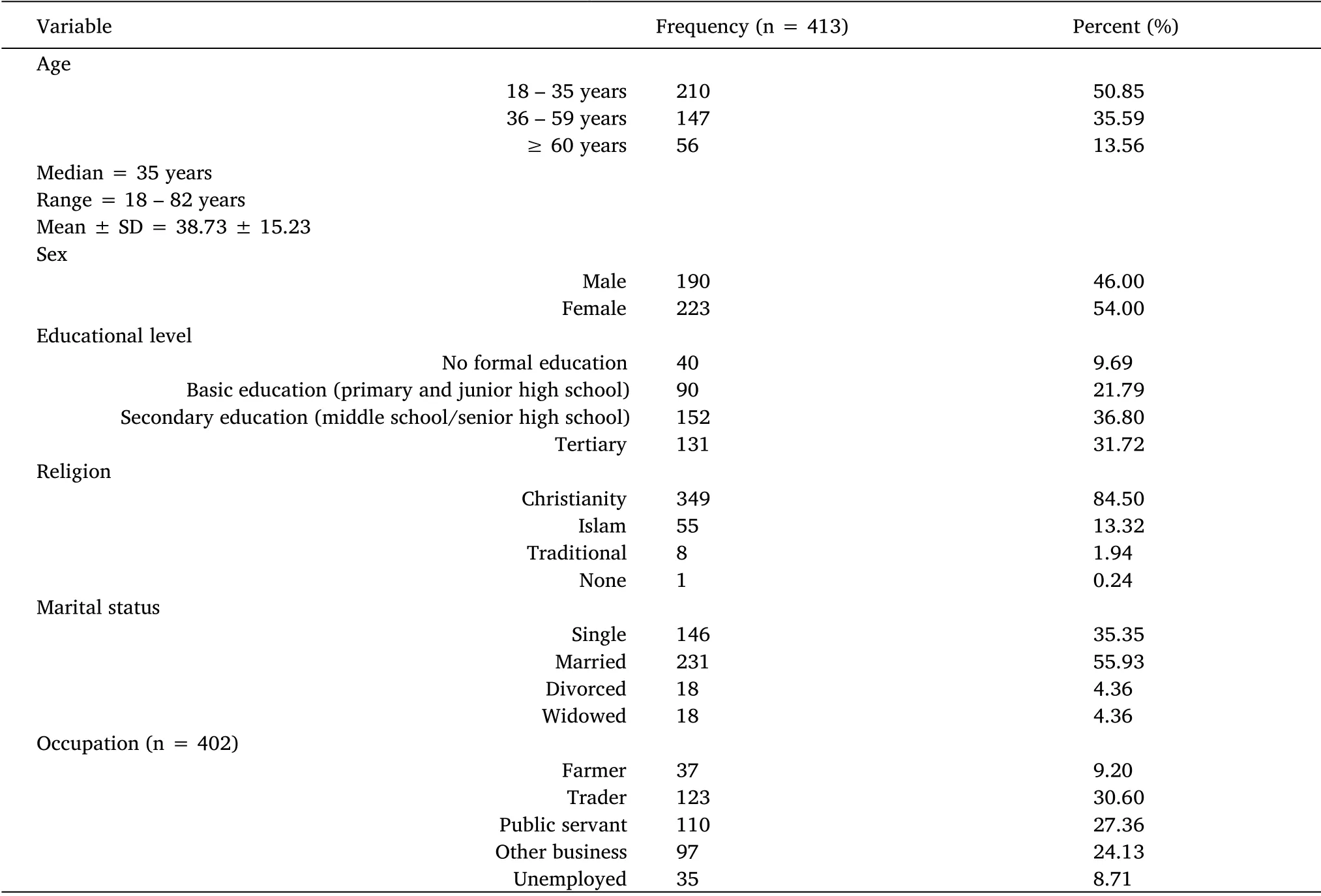
Table 2 Socio-demographic characteristics of respondents
Respondents’ knowledge on herbal medicine practice in Ghana
All respondents had heard of TM and knew that herbal medicine was a form of TM.Most participants (339; 83.1%) were previously aware of the existence of a herbal unit at the respective hospital and understood that the service rendered was as a result of the integration of herbal medicine into the healthcare system.Most respondents (355; 87%)were aware that the medical herbalist working at the respective herbal unit had been formally trained.Regarding the source of knowledge on herbal medicine unit at the various government hospitals, 202 (50%)respondents revealed that it was through a friend.Regarding adverse effects of herbal medicines, 320 (79%) of the 405 respondents who answered suggested that there were none.Table 3 shows a detailed description of the variables measured based on the respondents’knowledge on herbal medicine practices in Ghana.
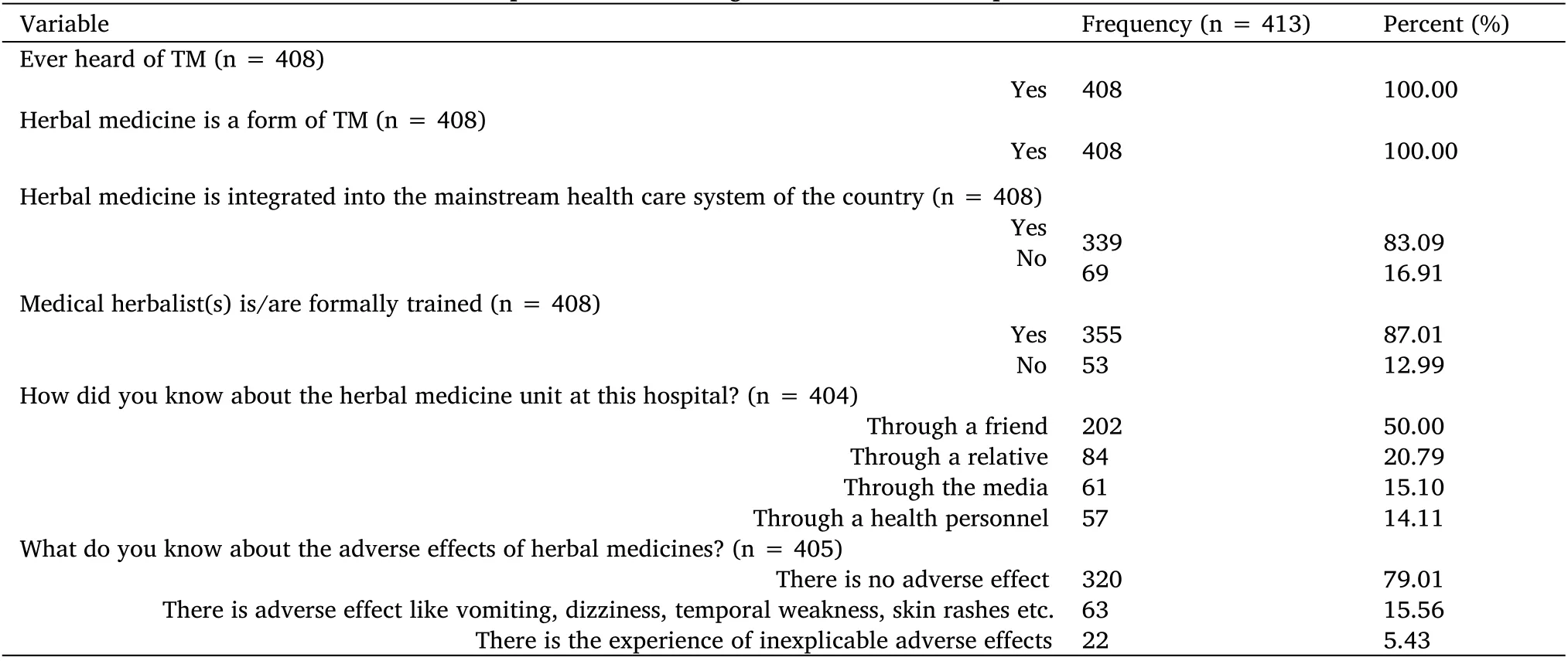
Table 3 Respondents’knowledge on herbal medicine practice in Ghana
Effects of costs of certified herbal drugs on the utilization of herbal medicine services at government hospitals
All 5 medical herbalists enrolled in the study reported that patients had to pay for every herbal drug dispensed at the herbal unit, with a minimum amount of Gh¢50 ($8.7) spent on herbal drugs per visit.
As shown in Table 4, 210 (51.5%) considered the per-treatment costs of purchasing herbal medicines from the herbal unit very high.Additionally, 294 (72.1%) respondents believed that the costs of herbal drugs dispensed at the herbal unit adversely affected the utilization of the service.Almost all respondents (406; 99.5%)recommended the inclusion of certified herbal drugs in the national health insurance drug list (NHIDL); however, 2 (0.49%) respondents recommended otherwise.The respondents also indicated that the costs of herbal drugs affected the utilization of the herbal unit.
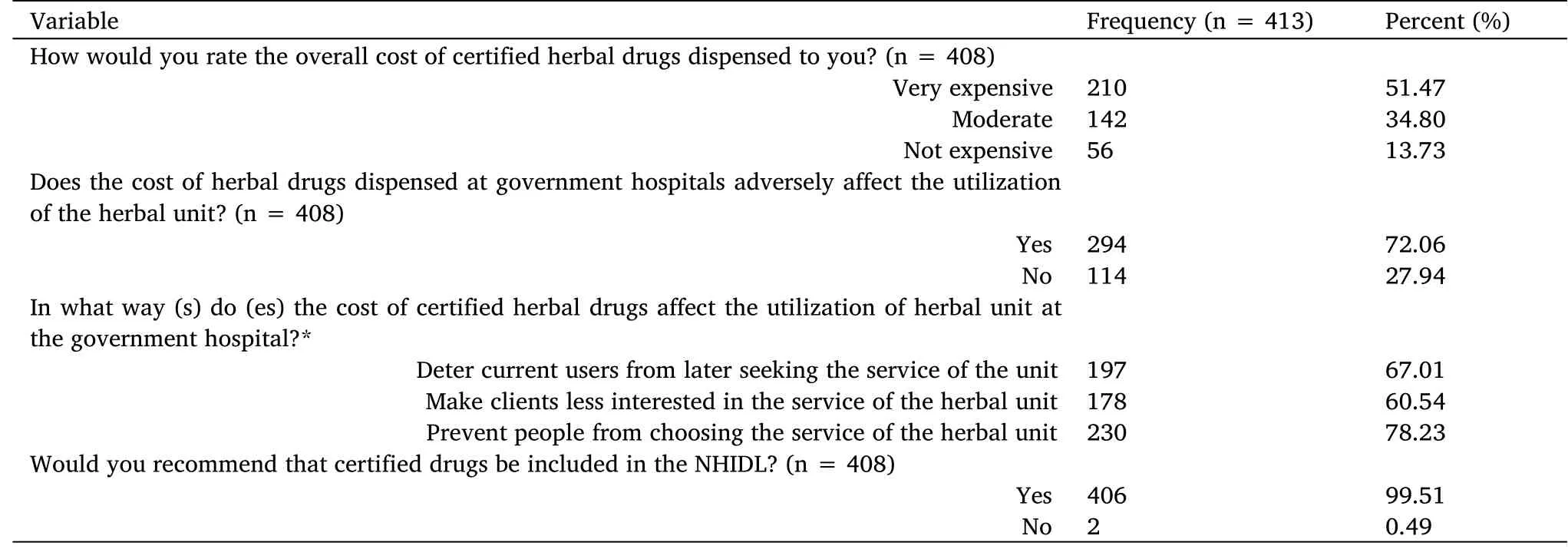
Table 4 Implication of the cost of certified herbal drugs on the utilization of the herbal unit at government hospitals
Discussion
This study explored the readiness of patients to continue using integrated herbal medicine units to meet their primary healthcare needs.Moreover, it evaluated the implications of out-of-pocket payments for herbal drugs administered to patients using such centers,the resultant effect on patient choice to continue seeking herbal medicine services, and the willingness of patients to recommend facilities to others.
Integration of herbal medicine services into any primary healthcare system is critical, and its benefits and positive outcomes are well documented in countries where they exist [24, 25].Under the German model, approximately 85% of the conventional practitioners participating in a national survey reported including some alternative therapies, especially botanicals, in their treatments;prescription-based services account for 20% of herbal medicines dispensed in the country [26, 27].In addition to the possible reduction of treatment costs, prescriber-based herbal medicine services are likely to increase the reporting and documentation of side effects.Taken together, these factors aid in the monitoring of treatment outcomes and evidence-based use of complementary therapies.
In Ghana, attention has been drawn to the importance of providing safe, standardized, and well-regulated herbal medicine services in health facilities.A pilot program for integrating such services began in 2011, with approximately 17 government health facilities across the country offering herbal medicine services to the Ghanaian public [13].Such herbal units are staffed with medical herbalists who are licensed to consult and prescribe herbal medicines to patients in governmental and private hospitals in Ghana [14].
The respondents in this study were individuals who had visited a herbal unit on at least one occasion.These participants attributed the services provided by the herbal unit to the integration of herbal medicine into the mainstream healthcare system.In addition,respondents were aware that medical herbalists working at herbal units were formally trained.This indicates that the general population was not naive to the use of herbal medicine in primary healthcare and had adequate knowledge of the integration process.Respondents also demonstrated characteristics of a population that held a preference for traditional/herbal medicines, as they were referred to these centers mainly through testimonials from friends and family.The participants generally believed that herbal medicines would exert no adverse effects, which has also been found in previous studies [28, 29]; the perceived safety of herbal remedies in certain communities is associated with sociocultural compatibility.
The results confirmed that clients who sought healthcare services at herbal units had to pay for the treatment dispensed to them after consultation.The minimum amount spent was Gh¢50 (equivalent to$8.7); the majority of patients considered this very expensive,although other studies have shown that users of herbal medicines generally consider the costs of such treatments affordable [14, 30].Such a contrast in the perception of costs could be income-related as our study population comprised low-income earners, mainly traders and farmers.Both medical herbalists and patients suggested that the costs of herbal medicines adversely affected the utilization of services provided by the herbal unit.Statistical analyses also indicated a relationship between these two factors.The costs of treatment may thus prevent people from using herbal units.Additionally, such costs were found to deter current clients from using herbal units again later and to reduce the probability of these clients to recommend these services.In line with this, a medical herbalist who participated in this study disclosed that some clients who were scheduled to return for clinical review failed to report because of the costs of medications.
Participants highly recommended the inclusion of certified herbal medicines in the NHIDL.From the perspective of medical herbalists,as the herbal unit is run as a primary healthcare facility, the inclusion of medications in the NHIDL will make such services equally accessible to the general population.Clients using herbal units also suggested that not everyone could afford herbal drugs.NHIDL compensation will thus make herbal medicine services accessible to all patients and increase the utilization of herbal units in the country.
Strength and limitations of the study
The objective of this study was to provide information that would enhance the discourse on integrated herbal medicine processes.The findings may help inform appropriate stakeholders to undertake restructuring of the integration process.Generalizability of the produced insights was facilitated by enrolling participants from all 3 government hospitals comprising herbal units within Kumasi Metropolis.Regardless of the appropriate study design, certain factors such as the sampling technique and interview time, may be a limitation.
Conclusion
The costs of certified herbal medicines negatively affect patronage and utilization of the services provided by the herbal unit at government hospitals.It is therefore imperative for certified herbal medicines to be covered by the NHIS to make the services of established herbal units accessible to the general public.
 Traditional Medicine Research2022年4期
Traditional Medicine Research2022年4期
- Traditional Medicine Research的其它文章
- Integration of multi-omics in investigations on the mechanisms of action of Chinese herbal medicine interventions in metabolic diseases
- Active compounds in RenShenJian decoction ameliorate insulin resistance in vitro
- Quality evaluation of Pinelliae Rhizoma using network pharmacology and multicomponent quantitative analysis
- Inhibition of rat prostate smooth muscle contractility by extracts of Costus speciosus(crepe ginger)
- Biologically active components for cosmeceutical use extracted from Chaetomorpha aerea
- Advances in traditional Chinese medicine for respiratory disease therapy in 2021
