Associations of early-life factors and indoor environmental exposure with asthma among children:a case–control study in Chongqing,China
Yun-Tian Deng·Xue-Mei Li·En-Mei Liu ·Wen-Kui Xiong·Shuo Wang·Rui Zhu·Yu-Bin Ding ·Zhao-Hui Zhong
Abstract Background Childhood asthma has substantial effects on children’s health.It is important to identify influencing factors in early life in the development of childhood asthma.We aim to evaluate the effects of early-life factors and indoor environmental exposure on childhood asthma in Chongqing,China.Method We designed a case–control study to enrol children with asthma aged 3 to <14 years old and controls in Chongqing,China.The “Children’s Early Life and Indoor Environment Survey” was used to collect the early-life factors and indoor environmental exposure of foetuses in utero and of infants during the first 3 years of life.A multivariate logistic regression model was used to evaluate the association between independent variables and childhood asthma and the interaction of early-life factors and environmental exposure.Results A total of 160 asthma cases and 247 controls were included in this study.The mean ages of the cases and controls were 5.53 ± 1.88 and 5.72 ± 2.34 years,respectively (P =0.192).Early-life factors and indoor environmental exposure were independently associated with childhood asthma.Infectious diseases of the respiratory system in children under 3 years old [adjusted odds ratio (OR)=5.76,95% confidence interval (CI) 2.49–13.30],bedroom air conditioner use (adjusted OR=4.61,95% CI 1.45–14.64),and bedroom dampness/mould (adjusted OR=2.98,95% CI 1.54–5.75) ranked as the three most significant exposures associated with the risk of childhood asthma.Other factors associated with an increased risk of childhood asthma included second-hand smoke exposure in early life (adjusted OR=1.93,95% CI 1.24–3.00),neonatal pneumonia (adjusted OR=1.90,95% CI 1.05–3.42) and maternal allergic diseases during pregnancy (adjusted OR=2.13,95% CI 1.10–4.10).The interaction effects of child second-hand smoke exposure with other covariates were not found to be statistically significant.Conclusions Early-life factors and indoor environmental exposure are closely related to childhood asthma in Chongqing,China.Further interventions and management in the early life of children should be considered to prevent and control childhood asthma in Chongqing and similar cities.
Keywords Asthma·Children·Environment·Risk/protective factor
Introduction
Asthma is the most common chronic disease among children and has exerted great effects on children’s health [1,2].The International Study of Asthma and Allergies in Childhood (ISAAC) reported rising global trends in the prevalence of allergic disorders [3].Globally,14% of children are affected by asthma,with a mortality rate of approximately 0.7 per 100,000 [4].In China,the prevalence of childhood asthma among children under the age of 14 has shown a steady increase during the past three decades,especially in urban areas [5,6].
The causes of allergic diseases are known to be anomalous immune responses and allergic inflammatory reactions,but the causes of these diseases in childhood are complex and involve hereditary and environmental factors[7,8].Increasing evidence has shown a potential association of lifelong environmental exposure with childhood asthma [9],and pregnancy and early life are critical time periods in the early programming of asthma [10].Many previous studies have developed and identified potential risk factors and protective factors for this special period.Some exposures,such as antibiotic use,exposure to indoor allergens or microbes,and microbial infections in early life,are potential stimuli for the early programming of asthma [11–18].Therefore,it is of great significance to identify important impacting factors in the development of childhood asthma in early life.
Chongqing is one of the largest municipalities located in Southwest China [19].Epidemiological surveys of asthma have reported that the prevalence of childhood asthma in Chongqing increased from 2.6% in 1990 to 3.3%in 2000 [5,20],3.3% in 2010,and 4.43% in 2013,with the second highest prevalence in China [21].Chongqing has unique climatic conditions of hot summers and cold winters with high relative outdoor humidity [22].The integrated maternal and child health system in Chongqing provides an excellent opportunity to investigate the associations of early-life factors and indoor environmental exposure with childhood asthma.
In this study,we aim to evaluate the effects of early-life factors and indoor environmental exposure on childhood asthma in Chongqing,China.
Methods
Study design and participants
A case–control study was designed to enrol children aged 3 to <14 years old with a physician diagnosis of asthma as cases from September 2020 to January 2021.The patients visited the asthma clinic departments of Chongqing Health Centre for Women and Children and Children’s Hospital of Chongqing Medical University,two main tertiary care facilities for children in Chongqing,China.Asthma diagnosis was based on the criteria of GINA2019 (Global Initiative for Asthma) [23] and the "Guidelines for the Diagnosis and Prevention of Children's Bronchial Asthma(2016 edition)" [24].For the purpose of comparison,controls were randomly selected from healthy children who visited the medical examination centres of these two hospitals in the same period and were matched by gender and age.The controls were reported not to have physiciandiagnosed asthma and not to have asthmatic symptoms(wheezing,dry cough,and chest tightness) during the past 12 months.Children in both the asthma and the control groups had lived in Chongqing from their mothers’ pregnancy to the survey date.The study excluded cases with congenital heart diseases,nervous system diseases,and other chronic diseases.
Data collection
We conducted a survey using a questionnaire to collect data on the early-life factors and indoor environmental exposure of foetuses in utero and infants during the first 3 years of life.We adopted the ISAAC questionnaire and the American Thoracic Society questionnaire (ATS-DLD-78-C) to collect data on the children’s respiratory health status and family history and adopted the questionnaire used in the Swedish Dampness in Buildings and Health study to collect data on indoor environmental exposure [25].The questionnaire was used and validated in the Chinese population [26,27],and the Cronbach’s alpha of the questionnaire was 0.97.
Early-life factors were defined as factors that occurred in the period from pregnancy to 3 years after birth (i.e.,pregnancy-related factors,birth factors,child factors,or sociodemographic determinants).We collected five earlylife factors,including maternal diseases during pregnancy,tobacco smoke exposure during pregnancy,feeding patterns,history of respiratory tract diseases and allergic diseases in children under 3 years old.Respiratory tract diseases and allergic diseases in children under 3 years old were based on doctors’ diagnoses,while maternal diseases during pregnancy relied on the parents’ self-report.
Indoor environmental exposure was defined as the family environment to which the child was exposed from pregnancy through the first 3 years.The questionnaires for indoor environment indicators included specific questions related to possible risk and protective factors.Specifically,11 factors on 5 aspects of indoor environmental exposure were taken into consideration,including child tobacco smoke exposure and the exposure level,family living environment(residential floor and air conditioner use),household cleanliness (bedroom dampness/mould,cockroaches in home,household cleaning frequency),indoor air quality (air purifier use,household cooking habits,kitchen layouts),and pet keeping.
Statistical analysis
The sample size was estimated on an assumed 50% exposure rate of environmental factors in the control group according to our pilot study and an estimated odds ratio (OR) of 2.0 in the case group.With 80% power and a 5.0% level of significance,the sample size of each group was not less than 140 subjects.
Categorical variables were expressed asn(%),and continuous variables were expressed as the mean ± standard deviation or as medians with interquartile ranges (IQR)according to the data distribution.Comparisons of categorical data between the case and control groups for patients were performed by the Chi-squared test or Fisher’s exact test,and continuous data were analysed by an independentsample Student’sttest or the Kruskal–Wallis test according to the distribution of data.
Logistic regression models were used to estimate the associations between exposures and outcomes.Univariate logistic regression was performed to identify potential variables associated with asthma by calculating the crude ORs and 95% confidence intervals (CIs).The multivariable logistic regression model consisted of variables with aPvalue <0.1 in the univariate regression model.The interaction effects were assessed using a multiplicative interaction term in the multivariable logistic regression model.The effect modification of demographic characteristics on the relationship between early-life factors and indoor environment exposure and the odds of childhood asthma were retained in the final model.The ORs and 95% CIs were adjusted by age and gender in the multivariable regression models.This study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology statement.
Statistical analyses were performed with SPSS version 26.0.AllPvalues were two-tailed tests,andPvalues <0.05 were considered significant.
Result
Demographic information
A total of 160 asthma cases and 247 controls were included in this study (Table 1).The study subjects were distributed in 21 central districts and 6 counties of Chongqing,concentrated in Yu Bei District (115,28.26%),Jiang Bei District(97,23.83%),Nan An District (49,12.04%),Sha Pingba District (24,5.9%),Jiu Longpo District (21,5.22%) and Yu Zhong District (19,4.73%).All children lived in urban areas without changing residence,and 91.4% of them lived in central districts.
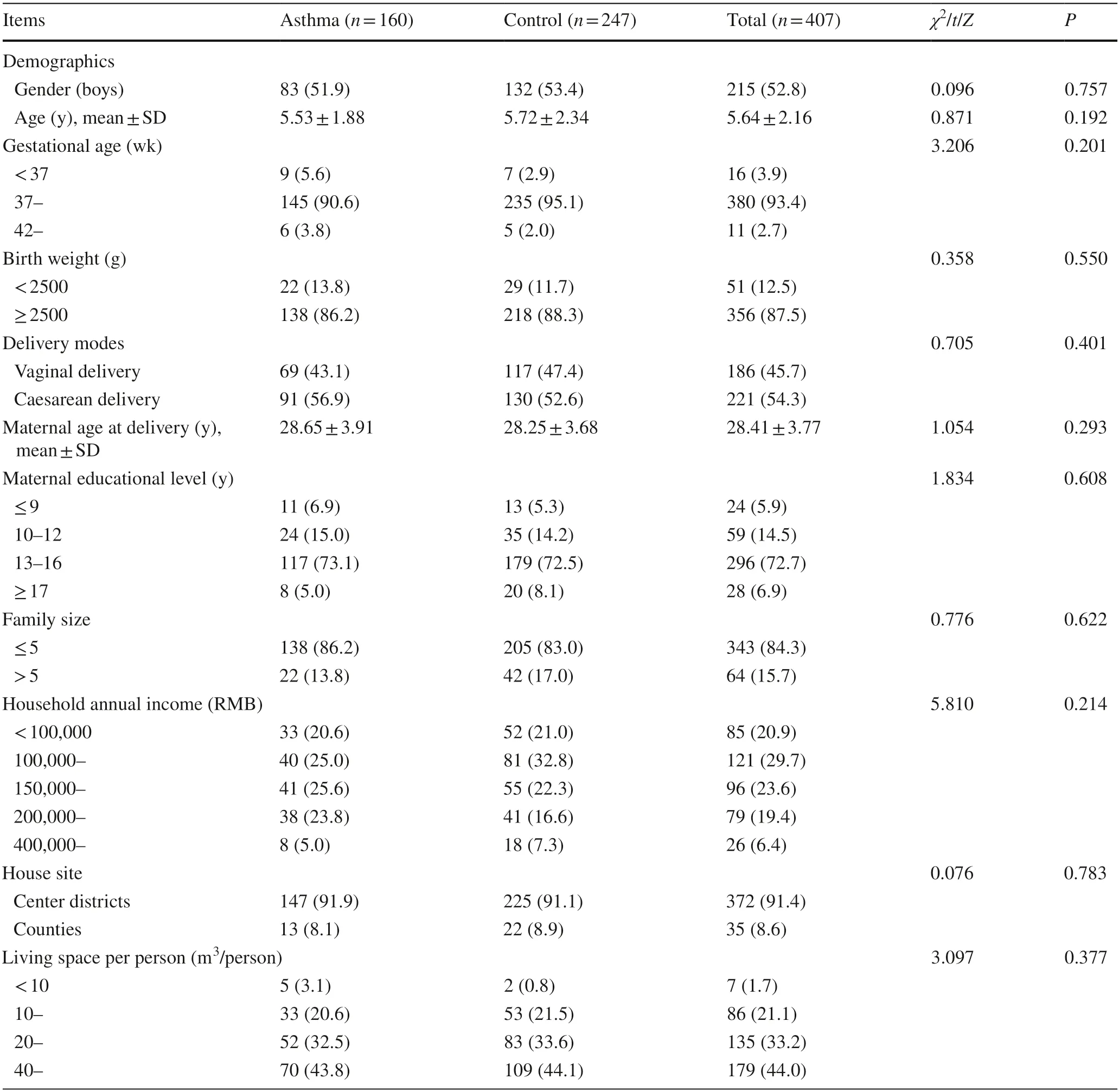
Table 1 Demographic information of study population
The mean ages of the cases and controls were 5.53 ± 1.88 and 5.72 ± 2.34 years old,respectively (P=0.192).The maternal delivery age and child gender distribution of the two groups were comparable,and no significant differences were observed for gestational age,birth weight or delivery modes.The proportion of education levels of mothers,household incomes,family size and average living space were not statistically different between the cases and controls (maternal educational level,P=0.608;family size,P=0.622;household incomes,P=0.214;living space per person,P=0.377,respectively).
Early-life factors and indoor environmental exposure associated with childhood asthma
ORs from univariate logistic regression of early-life factors and indoor environmental exposure for childhood asthma are shown in Table 2.With regard to maternal status during pregnancy,maternal history of allergic diseases,especially allergic asthma/rhinitis during pregnancy,showed an increased risk (OR=2.38,95% CI 1.31–4.35) of childhood asthma.Maternal exposure to second-hand smoke during pregnancy increased the risk of childhood asthma(OR=2.24,95% CI 1.49–3.36).There was no statistically significant difference in feeding patterns between asthmatic and control children.However,compared with children who had been breastfed for <3 months,those who had been breastfed for ≥ 3 months and ≥ 6 months had a lower risk of developing asthma (OR=0.52,95% CI 0.27–0.99;OR=0.48,95% CI 0.27–0.84,respectively).
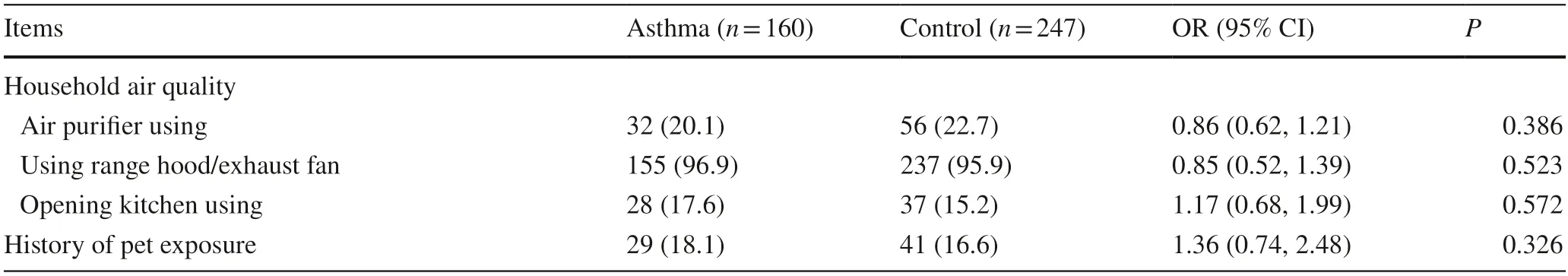
Table 2(continued)
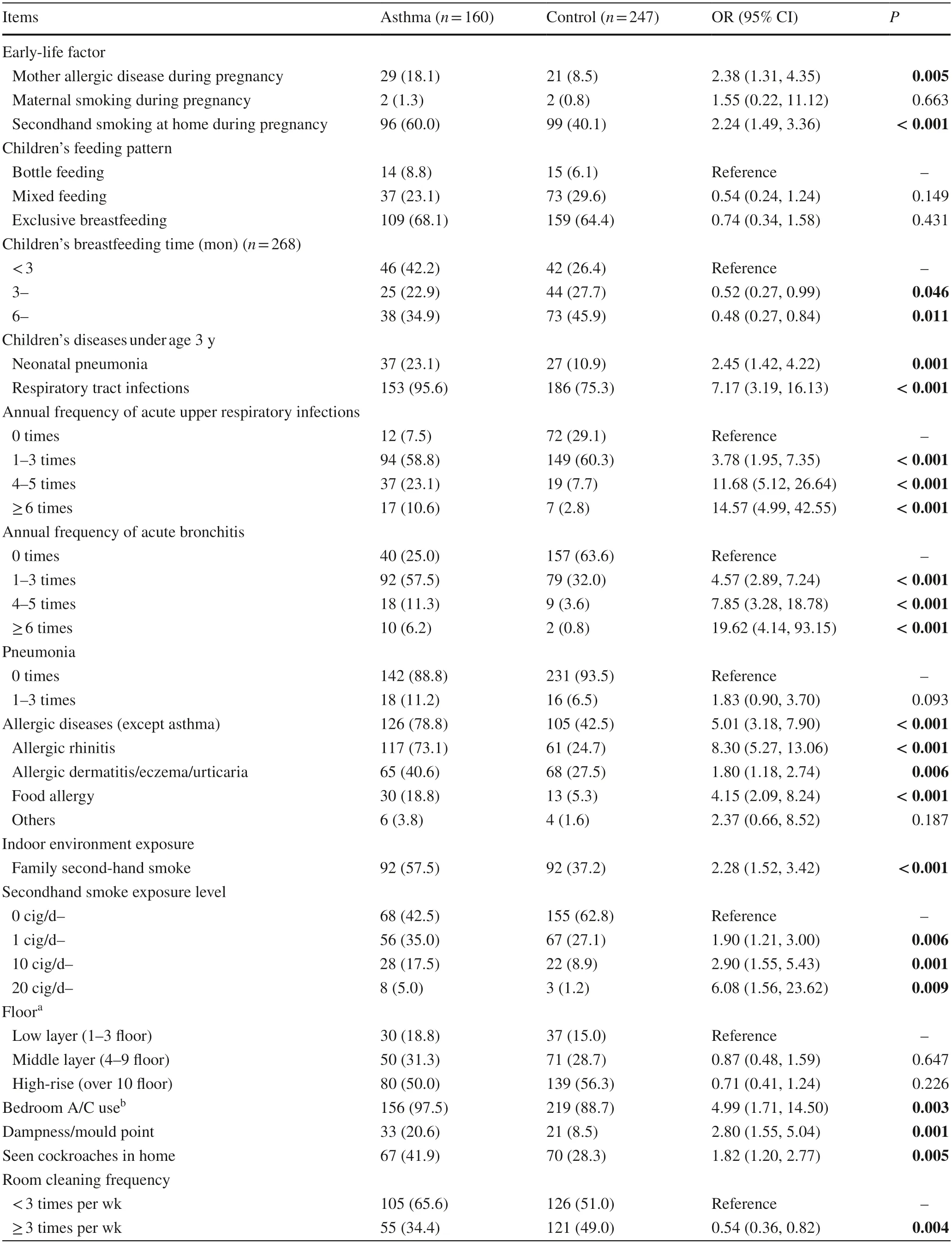
Table 2 Univariate logistic regression of early-life factors and indoor environment exposure for childhood asthma in Chongqing City
Regarding respiratory infections and allergic diseases in the first 3 years,23.1% of children with childhood asthma had been hospitalized for neonatal pneumonia,resulting in an increased risk of asthma (OR=2.45,95% CI 1.42–4.22).After the neonatal period,respiratory tract infections in the first 3 years significantly increased the risk of childhood asthma (OR=7.17,95% CI 3.17–16.13).The more frequent upper respiratory tract infections and bronchitis were,the higher the risk of childhood asthma,with a significant association of upper respiratory tract infections ≥ 6 times/year (OR=14.57,95% CI 4.99–42.55) or bronchitis ≥ 6 times/year (OR=19.62,95% CI 4.14–93.15).Allergic diseases in the first 3 years were related to childhood asthma(OR=5.01,95% CI 3.18–7.90).
For indoor environmental exposure,second-hand smoke exposure in the first 3 years increased the risk of asthma(OR=2.28,95% CI 1.52–3.42).An increasing level of cigarette exposure,1.90 for 1–9 cigs/day,2.90 for 10–19 cigs/day,and 6.08 for ≥ 20 cigs/day,suggested a dose–response relationship between smoke exposure and childhood asthma.
Visible dampness/mould and cockroaches in houses in the first 3 years after birth were associated with a higher risk of childhood asthma (OR=2.80,95% CI 1.55–5.04;OR=1.82,95% CI 1.20–2.77,respectively),while frequent room cleaning was associated with a lower risk of childhood asthma(OR=0.54,95% CI 0.36–0.82).The risk of childhood asthma increased when using an air conditioner in the bedroom(OR=4.99,95% CI 1.71–14.50).No significant associations were found between residential floor,range hood fans,open kitchens,air purifiers and keeping pets with childhood asthma.
Multivariate analysis between exposure and asthma with an interaction effect
As shown in Table 3,the multivariate logistic regression without an interaction term in Model 1 revealed thatmaternal allergic diseases during pregnancy (adjusted OR=2.13,95% CI 1.10–4.10),hospitalization for neonatal pneumonia (adjusted OR=1.90,95% CI 1.05–3.42),respiratory tract infections in the first 3 years (adjusted OR=5.76,95% CI 2.49–13.30),family second-hand smoke exposure(adjusted OR=1.93,95% CI 1.24–3.00),dampness/mould in bedrooms (adjusted OR=2.98,95% CI 1.54–5.75) and bedroom air conditioner use (adjusted OR=4.61,95% CI 1.45–14.64) increased the risk of childhood asthma.
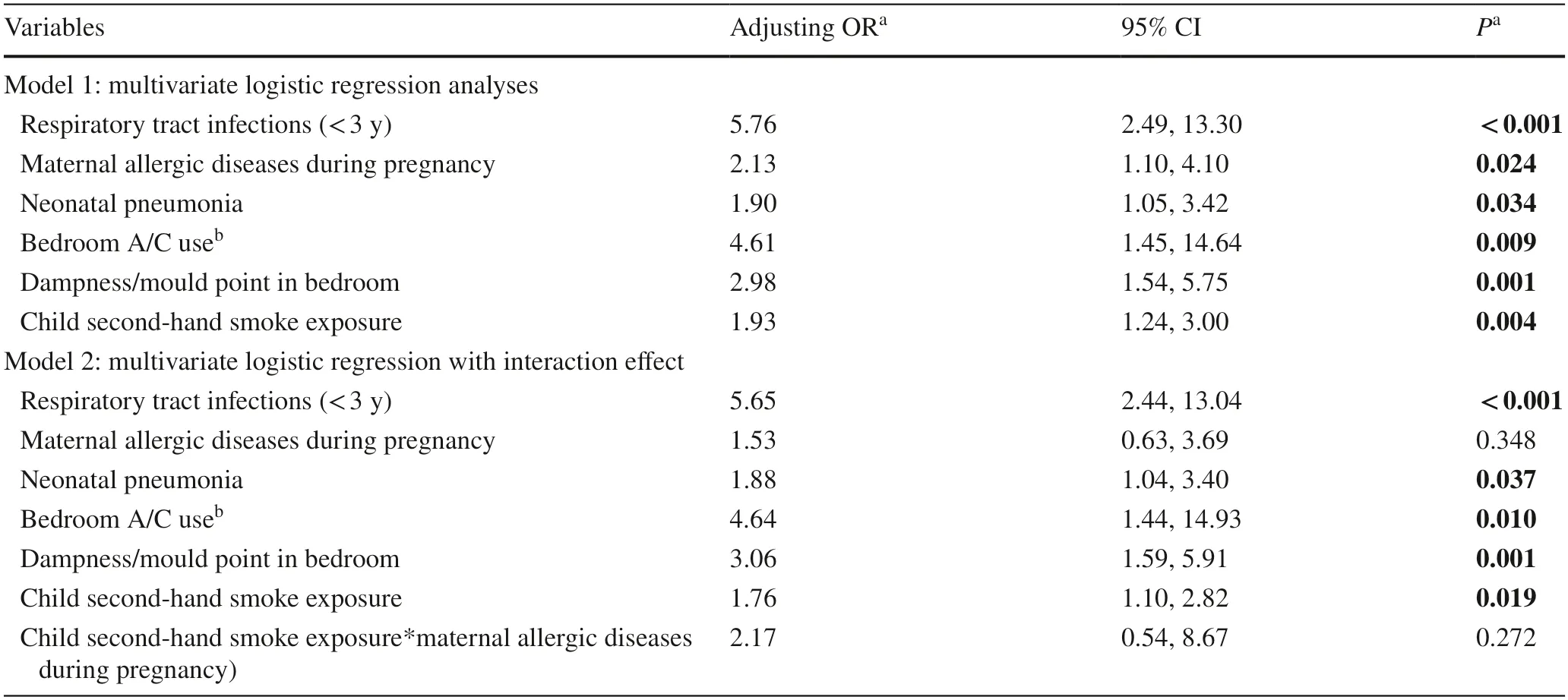
Table 3 Multivariate logistic regression analyses between exposure and asthma with an interaction effect
To explore the interaction of early-life risk factors and indoor environmental exposure on childhood asthma,we explored the interaction effects of child second-hand smoke exposure with other covariates.There was no statistically significant interaction between child secondhand smoke exposure and respiratory tract infections(OR=3.04,95% CI 0.51–17.96,P=0.221),maternal allergic diseases during pregnancy (OR=2.11,95% CI 0.57–7.94,P=0.265),neonatal pneumonia (OR=1.46,95% CI 0.47–4.51,P=0.513),bedroom air conditioner use(OR=0.29,95% CI 0.03–3.28,P=0.313),and dampness/mould (OR=1.61,95% CI 0.73–3.54,P=0.235).Considering that maternal allergic diseases during pregnancy are a significant risk factor associated with allergic diseases of children,we added the interaction term of child secondhand smoke exposure*maternal allergic diseases during pregnancy in the multivariate logistic regression.Although the test for the interaction term was not statistically significant (adjusted OR=2.17,95% CI 0.54–8.67,P=0.272),the interaction effect was suggested to increase the risk of childhood asthma.The effects of early-life factors and indoor exposure were still independently positively associated with childhood asthma (Table 3,Model 2).
Discussion
This study used a case–control study design to examine the association of early-life factors and indoor environmental exposure with asthma among children aged 3 to <14 years old in Chongqing,China.We found that maternal allergies during pregnancy,hospitalization for neonatal pneumonia,history of respiratory tract infections and allergic diseases in the first 3 years,early-life second-hand smoke exposure,exposure to visible mould,and air conditioner use increased the risk of childhood asthma,while longer duration of breastfeeding and frequent room cleaning might be protective factors for asthma.
A family history of allergies is a strong risk factor for asthma.Previous studies have also highlighted that children’s susceptibility during the perinatal period may be associated with the risk of allergic diseases,especially asthma [28].The results of our study suggest that maternal allergic diseases during pregnancy are risk factors for childhood asthma.Allergic diseases in children under the age of 3 are well-known risk factors for asthma.Allergic rhinitis and asthma are often correlated,and allergic rhinitis may cause childhood asthma in urban areas [29].Our findings also confirm that allergic rhinitis is an independent risk factor for childhood asthma as well as atopic dermatitis.
The association between prenatal and early-life secondhand smoke exposure and childhood asthma is well known,and our study is consistent with a previous study [30].The proportion of pregnant women who smoke is very low in China;however,pregnant women are likely to be exposed to a second-hand smoke environment.In a recent study in Chongqing,43.61% of pregnant women reported that their husbands were active smokers [31].Among children with asthma in our study population,60% of mothers reported exposure to second-hand smoke during pregnancy,and 55% reported exposure to household second-hand smoke in the first 3 years.Mechanisms of the impact of secondhand smoke on childhood asthma include structural airway remodelling,altered innate immune responses to pathogens and allergens,endocrine disturbing effects,and epigenetic modifications [32,33].
Notably,neonatal pneumonia and respiratory tract infections in early life were associated with childhood asthma in our study.Previous research has shown that viral respiratory infection may contribute to allergic sensitization [34],and is also closely related to childhood asthma,especially human rhinovirus (HRV) and respiratory syncytial virus (RSV) [35].HRV is commonly related to childhood wheezing and is associated with the development of childhood asthma [36].RSV can cause infection of the small bronchioles and inflammation of surrounding tissues,which can lead to bronchiolitis and increase the risk of childhood asthma [37];however,whether this association is causal remains a matter of controversy [38–42].In addition to virus infections,there also have been many investigations into the role of bacterial pathogens.Bisgaard et al.found that acute wheezy episodes in young children were associated with bacterial infections (Haemophilus influenzae,Moraxella catarrhalis,and Streptococcus pneumoniae),independent of the association with virus infections [43].In a recent birth cohort study (the Childhood Origins of Asthma Study)using nasopharyngeal mucus samples based on 16S rRNA,Staphylococcus-dominant microbiome in the first 6 months of life was associated with increased risk of recurrent wheezing by age 3 years and persistent asthma throughout childhood;during wheezing illnesses,detection of HRVs and predominance ofMoraxellawere associated with persistent asthma [44].Furthermore,the use of antibiotics in the early stages of life can cause changes in the microbiota of children.The effects exist in utero as well as in neonates and childhood,eventually increasing children’s susceptibility to asthma [45].In a populationbased study of 4.7 million children in Canada,the author found that the incidence of asthma increased by 24% with each 10% increase in antibiotic prescriptions in infancy[adjusted incidence rate ratio 1.24 (95% CI 1.20–1.28)][46].It is worth noting that asthma might be misdiagnosed as recurrent respiratory tract infections in clinical practice,especially for young children [47,48].Misdiagnosis of asthma,in addition to under-treatment with corticosteroids and over-treatment with antibiotics,results in unnecessary morbidity,poor quality of life and increased medical costs.
Breastfeeding has been suggested to decrease the risk of childhood asthma in some studies;however,there is no conclusive evidence that breastfeeding is a protective factor[49,50].In our study,we failed to find a significant association between feeding patterns and the risk of asthma.Nevertheless,we found that a long duration of breastfeeding decreased the risk of childhood asthma,which is consistent with previous studies [51,52].Maternal microbes and other factors in breastmilk shape the composition and diversity of the early-life gut microbiota in direct and indirect ways,which influences immune system maturation and may protect against allergies [53,54].Human milk oligosaccharides in breastmilk also affect epithelial barrier functions to block the attachment of microorganisms to epithelial cell surface sugars,thereby preventing respiratory infectious diseases and reducing asthma attacks [55].
In our study,bedroom dampness and mould in early life were found to be associated with childhood asthma.It has been reported that the absolute concentration of most mould taxa maintains an increasing trend at elevated humidity [49,56].Due to its specific topographical location,Chongqing has high relative humidity throughout the year [57].Consistent with our study,a cross-sectional study in Chongqing found a significant association between household dampness,mould and childhood asthma,with an especially stronger association for early residence [58].Several other studies have also found that children with household dampness and mould exposure in their early residence had higher odds of developing allergies and airway diseases [59–62],which might be explained by the association between dampness/mould and asthma-associated bacteria in the indoor environment [63].Moreover,the risk of indoor mould exposure was not masked by the stronger effect of secondhand smoke,suggesting that household mould exposure in Chongqing might be more serious.Parents in Chongqing should be aware of the need to reduce indoor dampness and mould exposure.
Air conditioners can help regulate the indoor temperature and reduce humidity,theoretically improving asthma control;however,they may trigger and aggravate asthma if not properly maintained [64].When the filters are dirty,air contaminants,such as mould spores,breed in them and increase indoor airborne contaminants [65].It is,therefore,important for family members to properly maintain the filters of air conditioners and air purifiers.
The interaction between early-life factors and indoor environmental exposure was the focus of our study.We selected child second-hand smoke exposure and maternal allergic diseases during pregnancy to estimate the most significant interaction pattern and found that the interaction effect,although not significant,was suggested to increase the risk of childhood asthma.In a Norwegian cohort study,the effect of early-life environmental tobacco smoke exposure on asthma was found to be stronger in children with parental atopy than in children without parental atopy [66].There might be a gene–environment interaction between early tobacco exposure and genetic risk factors that affects the susceptibility to asthma.More studies are needed to validate this possibility.
Our findings highlight the effect of early-life factors and indoor environmental exposure on childhood asthma,which presents a potential window for intervention for the prevention of childhood asthma.Harju et al.reported that paternal cessation of smoking during pregnancy was associated with a decreased risk of asthma [67].Smoking has been banned in indoor public places in Chongqing since January 2021.Furthermore,cessation programmes should be carried out in household life.Indoor allergen mitigation strategies are recommended in the asthma management guidelines,including single-component allergen-specific interventions and multicomponent interventions.A multicomponent mitigation strategy is the use of two or more single-component interventions,such as air purifiers,high-efficiency particulate arrestance vacuum cleaners,mould mitigation,and pet removal [68].Regarding the reduction of respiratory tract infections,a palivizumab-based prophylaxis strategy in the prevention of RSV infection in high-risk infants seems to reduce wheezing illnesses early in life;however,its effect on subsequent asthma development has not yet been demonstrated [69].
This study has some limitations.First,we used questionnaires to collect information regarding early-life factors and indoor environmental exposure.There may have been inevitable inaccurate recall or misunderstanding of questions.However,because 98% of the surveyed children were from a onechild family and nearly 95% of the mothers had received more than 10 years of education,the potential for recall bias was minimal in this study.Second,although confounding factors were considered in the multivariate analysis,other factors were perhaps not included in this study,including the use of antibiotics during pregnancy,ambient air pollution,and parental stress.The ORs in our association analyses may be overestimated.Finally,the number of surveyed children was small,and larger scale studies are needed to confirm our findings.
AcknowledgementsWe sincerely appreciate all the children,parents,and others who were involved in the study.
Author contributionsDYT performed the statistical analysis and drafted the manuscript,contributed to the study design and participants recruitment.LXM and LEM conceived the study and developed its design.XWK,WS and ZR were involved in the study design and participants recruitment.DYB and ZZH supervised the field work and revised the manuscript.All authors have read and approved the final manuscript.
FundingThe study was funded by Scientific Research &Innovation Experiment Project of Chongqing Medical University (grant/award number:SRIEP202107),Chongqing Health Commission and Chongqing Municipal Bureau of Science and Technology Key Funding(grant/award number:2019ZDXM017).
Data availabilityData are only available on an approved request to the corresponding author.
Declarations
Ethical approvalThe ethical application and the consent procedure of this study were approved by the Ethics Committees of Chongqing Medical University (2021016) and Chongqing Health Center for Women and Children (2019005).
Conflict of interestNo financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.The authors have no conflict of interest to declare.
 World Journal of Pediatrics2022年3期
World Journal of Pediatrics2022年3期
- World Journal of Pediatrics的其它文章
- Long-term physical,mental and social health effects of COVID-19 in the pediatric population:a scoping review
- Prediction modelling in the early detection of neonatal sepsis
- Maternal smoking status during pregnancy and low birth weight in offspring:systematic review and meta-analysis of 55 cohort studies published from 1986 to 2020
- Urinary cystatin C:pediatric reference intervals and comparative assessment as a biomarker of renal injury among children in the regions with high burden of CKDu in Sri Lanka
- Handmade tri-leaflet ePTFE conduits versus homografts for right ventricular outflow tract reconstruction
- Occurrence of early epilepsy in children with traumatic brain injury:a retrospective study
