Onyx embolization of a spinal epidural hemorrhage caused by thoracic spinal epidural arteriovenous fistula: A case report and literature review
Xi Chen, Liang Ge, Hailin Wan, Lei Huang, Yeqing Jiang, Gang Lu, Xiaolong Zhang
Department of Radiology, Huashan Hospital, Fudan University, Shanghai, 200040, China
Keywords:Endovascular therapy Spinal epidural arteriovenous fistula Spinal epidural hemorrhage
ABSTRACT Spinal epidural hemorrhages (SEDH) caused by spinal epidural arteriovenous fistulas (SEAVFs) are rare; thus,their specific pathogenesis has not been explained. Furthermore, the standard treatment for SEAVFs has not yet been defined.Here we report the case of a 36-year-old Chinese man who experienced acute onset chest pain and tightness. His symptoms rapidly aggravated until the lower limbs were unable to support him. Spinal magnetic resonance angiography (MRA) revealed a localized SEAVF and a secondary spinal cord lesion at the T4 level.Digital subtraction angiography(DSA)confirmed the presence of the SEDH/SEAVF at the T3–4 level with the left radicular artery feeding the fistula.Based on DSA and MRA findings,SEDH,local spinal cord infarction,and spinal venous reflux disorder were conditionally diagnosed. Using the arterial route, Onyx-34 was injected into the fistula to embolize the feeding arteries and the venous system. Angiography was performed after the microcatheter was withdrawn, and no residual fistula or anterior spinal artery was observed. The six-week follow-up MRI showed acceptable healing of the SEAVF, and the patient improved neurologically. This case suggests that endovascular treatment with Onyx-34 embolization should be considered a promising treatment strategy for this type of complicated SEAVF.
1. Introduction
Spinal epidural arteriovenous fistulas (SEAVFs) often cause neurological morbidity owing to venous hypertension or mass effects. The standard treatment for SEAVF has not yet been defined, with reported options including surgical, endovascular, and medical treatments.1–3Spinal epidural arteriovenous fistulas (SEAVFs) are accepted causes of spinal infarction or epidural hemorrhage(SEDH).4,5
In contrast to dural arteriovenous fistulas, only a few SEAVFs have been documented. The lack of knowledge of its etiology and the lesion characteristics makes it difficult to establish treatment strategies for SEAVFs. Bleeding is generally considered unlikely in patients with SEAVF. Therefore, conservative treatment can often be adopted in asymptomatic cases or those with tolerable symptoms, indicating no counterflow in the perimedullary vein.6
Some reports have described the successful surgical and endovascular treatment of SEAVFs.7–9Moreover,rare cases of SEDH caused by SEAVFs treated with endovascular therapy were previously reported. Here we report a case of SEDH/SEAVF that was successfully treated with endovascular treatment using Onyx-34.
2. Case report
A 36-year-old Chinese man experienced acute-onset chest pain and tightness late at night on July 16. The patient's lower limbs had developed weakness and hypoesthesia.His symptoms aggravated rapidly until he was unable to walk or stand within 14 h the following day.
Magnetic resonance imaging (MRI day 1) of the brain was normal.Magnetic resonance angiography(MRA day 1,not shown)of the spinal column showed an abnormal signal in the T2–6 region of the spinal cord that was considered acute myelitis. Corticosteroids were administered at a local hospital,but his symptoms were not alleviated.After medical treatment, his chest pain and tightness disappeared, but sensation below the T6 level was lost with incontinence and paralysis below the waist.
On admission on August 31, the patient remained fully alert and reported no previous medical history. The modified Aminoff and Logue score was 5, and a physical examination determined that the muscle strength of the bilateral lower limbs was 0,while that of the upper limbs was normal; a complete sensory deficiency was detected below the T6 level. The patient had defecatory and voiding dysfunction. Spinal MRA(day 48) revealed an enhanced lesion on the left side of the epidural space at the T3–4 level and an abnormal signal at the T4 level (Fig.1).
The patient was diagnosed with localized spinal epidural arteriovenous fistula(SEAVF)with a possible secondary spinal cord lesion at the T4 level.Spinal digital subtraction angiography(DSA day 54)revealed a spinal epidural hemorrhage caused by SEAVF on the left side of the epidural at the T3–4 level(Fig.2)fed by the left radicular artery.DSA and MRI findings suggested a local spinal cord infarction and spinal venous reflux disorder.SEDH was limited to the epidural space at the T3–4 level,while a secondary spinal cord infarction was found via MRA and DSA.The final diagnosis was SEDH caused by a SEAVF.
Medical treatment was first selected at a local hospital out of concern for paralysis caused by the spinal cord injury and possible spinal arterial embolism resulting from surgical or endovascular interventions.Despite paraplegia and the progressive epidural hemorrhage visible on DSA,interventional therapy is the primary strategy.
After heparinization, a Cobra catheter was inserted in the left T4 intercostal artery. Guided by a Synchro-10 wire, the Marathon microcatheter was navigated into the feeding artery. Angiography via a microcatheter showed that the feeding artery penetrated the epidural venous plexus and the distal spinal artery.Nimodipine was administered via the microcatheter,which was guided to the distal part of the feeding artery. Microcatheter angiography showed that the spinal artery dissection and the proximal end of the feeding artery were directly connected to the epidural venous plexus(Fig.3).
The coils available at our center were not suitable for use with the Marathon microcatheter. Therefore, Onyx-34 was injected into the venous segment to successfully embolize the feeding arteries. Angiography was performed after the microcatheter was withdrawn, and no residual fistula or anterior spinal artery was found (Fig. 4). Follow-up MRI performed 6 weeks after endovascular therapy showed SEAVF healing(Fig.5), and the patient improved neurologically. The modified Aminoff and Logue score was 5 – the muscle strength of the bilateral lower limbs was 0, that of the upper limbs was normal, and sensory deficiency persisted below the L1 level.
3. Discussion
SEAVF is a distinctly infrequent spinal vascular disease defined as direct communication between the extradural or paravertebral arterial branches and the extradural venous plexus.10Venous drainage can flow retrogradely into the subdural or perimedullary venous system,resulting in venous hypertension myelopathy,spinal cord function injury,or spinal cord compression injury caused by dilatation of the extradural vein.11SEDH caused by SEAVF are rare,and no standard of treatment has been defined. Because of the difference in SEAVF conditions, we must formulate individual treatment strategies strictly.Owing to the variety of SEAVF manifestations, treatment strategies must be devised on a case-by-case basis.
Most of the current literature is limited to case reports,and no large case analysis exists for SEAVF.Therefore,the incidence and prevalence of SEAVF have not yet been determined,and its etiology and pathogenesis remain unknown. Some researchers have suggested that injury to the extradural venous plexus by discectomy or other spinal surgeries may be the pathological basis of SEAVF. In a systematic review, Huang et al.12reported that 10% of SEAVF patients had a history of spinal surgery.However, most documented SEAVFs lack a specific history and are idiopathic.No history of surgery or trauma was present in this case.
Yu et al.13described three cases of five SEDHs caused by SEAVF,resulting in good outcomes after microsurgical treatment. However,these may represent early-stage SEAVFs. Rispoli et al.14described one case involving urgent surgical decompression through an epidural hematoma; postoperatively, the patient completely recovered motor function of the upper and lower extremities. However, different cases may represent different developmental stages of the disease, and these cases may represent early stages of SEAVF.Surgical treatment may be the best option in acute cases.
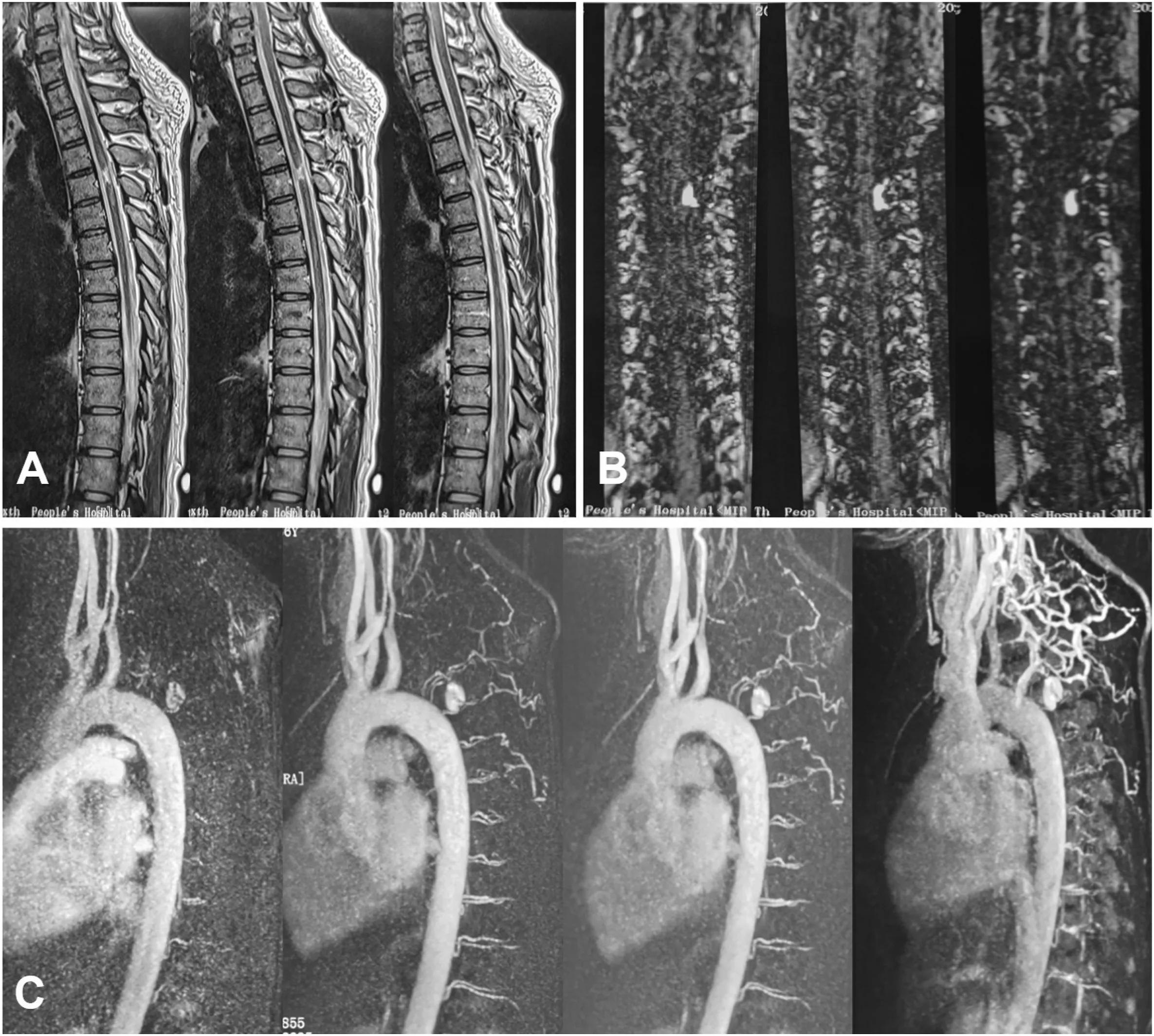
Fig. 1. A. T2WI showed high signals in the T4 spinal cord (spinal cord infarction) and abnormal signal lesions outside the spinal dura at the T3-4 level. B. TWIST identified high signal lesions outside the spinal dura at the T3-4 level. C. MRA revealed the feeding artery and high signal lesions outside the spinal dura at T3-4.

Fig.2. A.DSA detected a SEAVF on the left side of the epidural at the level of T3-4 fed by the left radicular artery,while the spinal artery was not captured.The lesion was larger than depicted on the MRI,due to obvious extravasation of the contrast medium.B.3D reconstruction showed the lesions located outside the spinal dura at the T3-4 level.
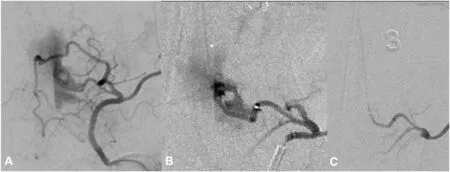
Fig.3. A.No spinal artery was perceivable on angiography.B.Angiography via microcatheter revealed that the feeding artery entered the epidural venous plexus,and the distal spinal artery was thereby visualized (arrow). C. The spinal artery dissection and its proximal end were directly connected to the epidural venous plexus.
Determining a treatment strategy becomes extremely difficult in longterm cases of SEDH caused by spinal SEAVF,as no previous reports have described the successful treatment of such lesions. Due to the lack of specificity of clinical symptoms and imaging features, SEAVF is often misdiagnosed and its treatment is delayed. In this study, the local hospital misdiagnosed the problem, but we were able to correctly identify and successfully treat the problem.

Fig.4. A,B.The feeding arteries were successfully embolized by injecting Onyx-34 into the venous system.C.The microcatheter was withdrawn and an angiography reperformed. No residual fistula was found.
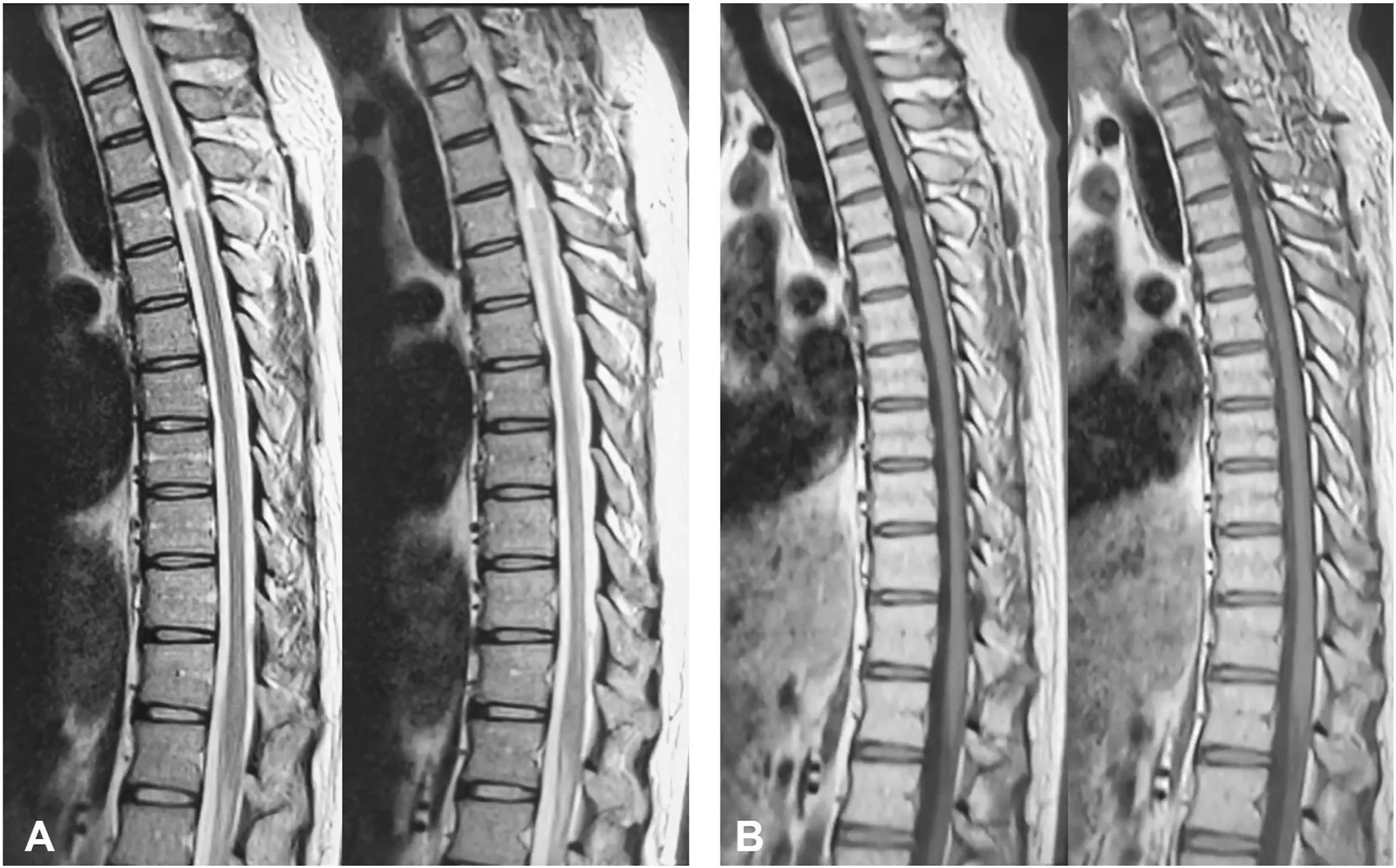
Fig. 5. A. T2WI showed a high signal in the T4 spinal cord. B. T1WI showed a low signal in the T4 region. While myelopathy has not been cured, the epidural arteriovenous fistula nearly disappeared.
SEAVF is a significant cause of SEDH.Conservative treatment cannot prevent multiple re-bleeding episodes. Endovascular embolization and microsurgery are the preferred treatment strategies for SEDH/SEAVF.The clinical outcome of SEDH/SEAVF is crucially related to its manifestation: the milder the symptoms, the better the outcome.15According to the literature, the curative rate for interventional therapy alone is 75–90%.16The key to treatment is locating the fistula and completely disrupting the arteriovenous connection. Embolization is intended to block the fistula connection,thereby alleviating the pressure of the dilated venous system.Treatment consists of complete obliteration by embolization or excision to provide symptom control and prevent further neurological deterioration.17,18Endovascular embolization is preferable to extensive surgery for removing the entire venous pouch unless emergency hematoma evacuation is necessary.19Significant venous occlusion is likely to result in substantially greater deterioration due to outflow restriction of any additional AVF regions. During embolization, embolic material filling the proximal segment of the draining vein is an indicator of complete fistula obliteration. Thus, endovascular treatment with maneuverable Onyx-34 is a favorable choice for SEAVF management.20
Interventional embolization alone causes the embolic agent to occupy the entire venous lacuna,thereby making it difficult to reduce the volume of the venous lake.In our case,partial embolization of the feeding artery reduced the pressure of the venous lake and achieved good results. The main complication of interventional therapy is that the blood supply to the anterior spinal artery is affected by embolization of the radicular artery.Therefore,the development of the anterior spinal artery should be scrutinized using angiography of the artery feeding the fistula. If the anterior spinal artery is not developed,the possibility of arterial damage cannot be ruled out.The degree of spinal cord function recovery is closely related to the time from onset to treatment. The later the diagnosis, the less likely the spinal cord function will recover. Follow-up methods should include MRI to observe the range of abnormal intramedullary signals and try to detect abnormal pressure in the venous system.
4. Conclusion
The etiology of spinal epidural hemorrhage is an epidural arteriovenous fistula. This may be because the radicular artery ruptured when it passed through the dura mater and moved into the pial artery.Although several options have been suggested for treating SEDH caused by SEAVF,endovascular treatment with Onyx-34 embolization should be considered a promising treatment strategy for such difficult SEDH/SEAVF lesions.
Patient consent
Written informed consent was obtained from patients for publication of this case report and any accompanying images.
Declaration of competing InterestCOI
The authors declare that there is no conflict of interest. We declare that we do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Funding
This study has received funding from the National Natural Science Foundation of China(Grant No.81771242).
 Journal of Interventional Medicine2022年2期
Journal of Interventional Medicine2022年2期
- Journal of Interventional Medicine的其它文章
- Intravascular treatment for abnormal catheter positioning of port-a-cath system in the subclavian vein: A single-center study
- A creatinine-based model for predicting recurrent bleeding after modified percutaneous transhepatic variceal embolization in patients with cirrhosis
- Irreversible electroporation versus radiofrequency ablation for malignant hepatic tumor: A prospective single-center double-arm trial
- Safety and efficacy of transcatheter arterial embolization for management of refractory hematuria of prostatic origin
- Intrahepatic flow diversion prior to segmental Yttrium-90 radioembolization for challenging tumor vasculature
- Preparation and investigation of a novel iodine-based visible polyvinyl alcohol embolization material
