Intravascular treatment for abnormal catheter positioning of port-a-cath system in the subclavian vein: A single-center study
Yong Li, Jianxi Guo, Yanfang Zhang, Jian Kong
Department of Interventional Radiology,Shenzhen People’s Hospital(Second Clinical Medical College of Jinan University,First Affiliated Hospital of Southern University of Science and Technology), Shenzhen, China
Keywords:Port-a-cath system Tip migration Catheter fracture Intravascular treatment
ABSTRACT
1. Introduction
The Port-a-cath system(PCS)is a long-term indwelling venous access device that can be implanted subcutaneously.It avoids unnecessary pain and repeated punctures and allows the administration of medicines directly to the central venous system.The most common complications of PCS are venous thrombosis, infection, and abnormal catheter positioning.1,2Abnormal positioning includes migration3,4and fracture of catheters.5Percutaneous puncture is a safe, effective, and minimally invasive method of intravascular adjustment or removal of abnormally positioned catheters. This report describes the clinical use of cobra catheters, pigtail catheters, and retrieval devices for intravascular adjustment or removal of abnormally positioned catheters through percutaneous punctures.
2. Materials and methods
2.1. Patients
A retrospective analysis was conducted on 58 patients with tumors who were noted to have abnormal catheter positioning and underwent intravascular treatment through percutaneous punctures in the Interventional Radiology Department of Shenzhen People’s Hospital between January 2009 and June 2019. The diagnosis of abnormal catheter positioning was confirmed in all patients using preoperative plain chest radiography or computed tomography (CT) images. Percutaneous puncture was then performed for intravascular adjustment of the migrated catheters or removal of the fractured catheters. All interventional procedures were performed using digital subtraction angiography(DSA) in interventional operating rooms. All patients were hospitalizedand signed an informed consent form prior to study enrollment. The present study was reviewed and approved by the Ethics Committee of Shenzhen People’s Hospital,China(NO.LL-KY-2020443).
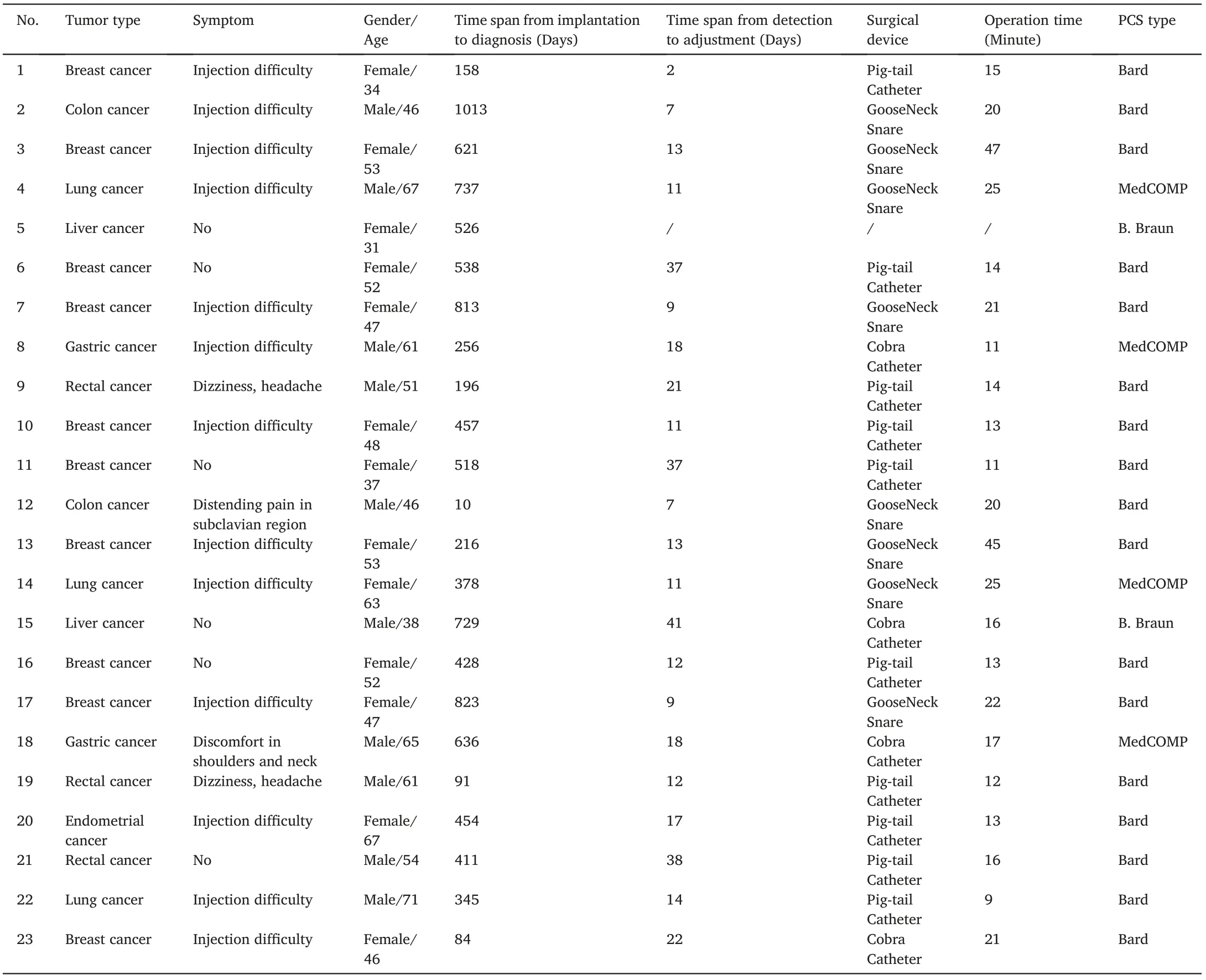
Table 1 Clinical data of patients with catheter migration.
2.2. Perioperative management
Color ultrasonography of the subclavian vein and internal jugular vein, D-dimer test, routine blood test, and coagulation function examination were performed on all patients before surgery. During surgery,real-time monitoring of the blood pressure, heart rate, and electrocardiogram indices was performed.Data on total blood count,prothrombin time (PT), and partial thromboplastin time (PTT) were obtained within three days after surgery.
2.3. Operative technique
Local anesthesia was given in the supine position by administering 2% lidocaine hydrochloride injection to the patient’s right inguinal region. The femoral vein was then punctured using the Seldinger technique, and guidewires and vascular sheaths were introduced under fluoroscopy guidance.In this study, 6 F sheaths were used to adjust the catheter position, whereas 8 F or larger sheaths were used to remove fractured catheters.
A cobra catheter (Cordis, Miami Lakes, FL, USA) or pigtail catheter(Cordis, Miami Lakes, FL, USA) was used to relocate migrated catheters to the superior vena cava by pulling on the junction of the subclavian vein and the internal jugular vein.The tail of the pigtail catheter was cut into a semicircular shape using sterile scalpels to hook the catheter.A 6 F gooseneck snare (Microvena, White Bear Lake, MN, USA) was used to hook the free end of the catheter and reposition it to the superior vena cava when the use of both the cobra and pigtail catheters had failed.
The gooseneck snare was also used to retrieve fractured catheters.Exposure of the free end was achieved by using the tail of the pigtail or cobra catheter to hook the middle part of the fractured catheter when it was difficult to see.The gooseneck snare was then used to hook the free end and pull the catheter downward to the vascular sheath. The entire system would be subsequently removed.
Intraoperative angiography was performed to assess the presence of thrombosis and electrocardiographic monitoring was performed to record immediate operation-related complications. Patients with catheter migration underwent chest radiography every month after surgery and were followed up for three consecutive months. Patients with catheter fracture were followed-up through telephone interviews for one month after surgery.
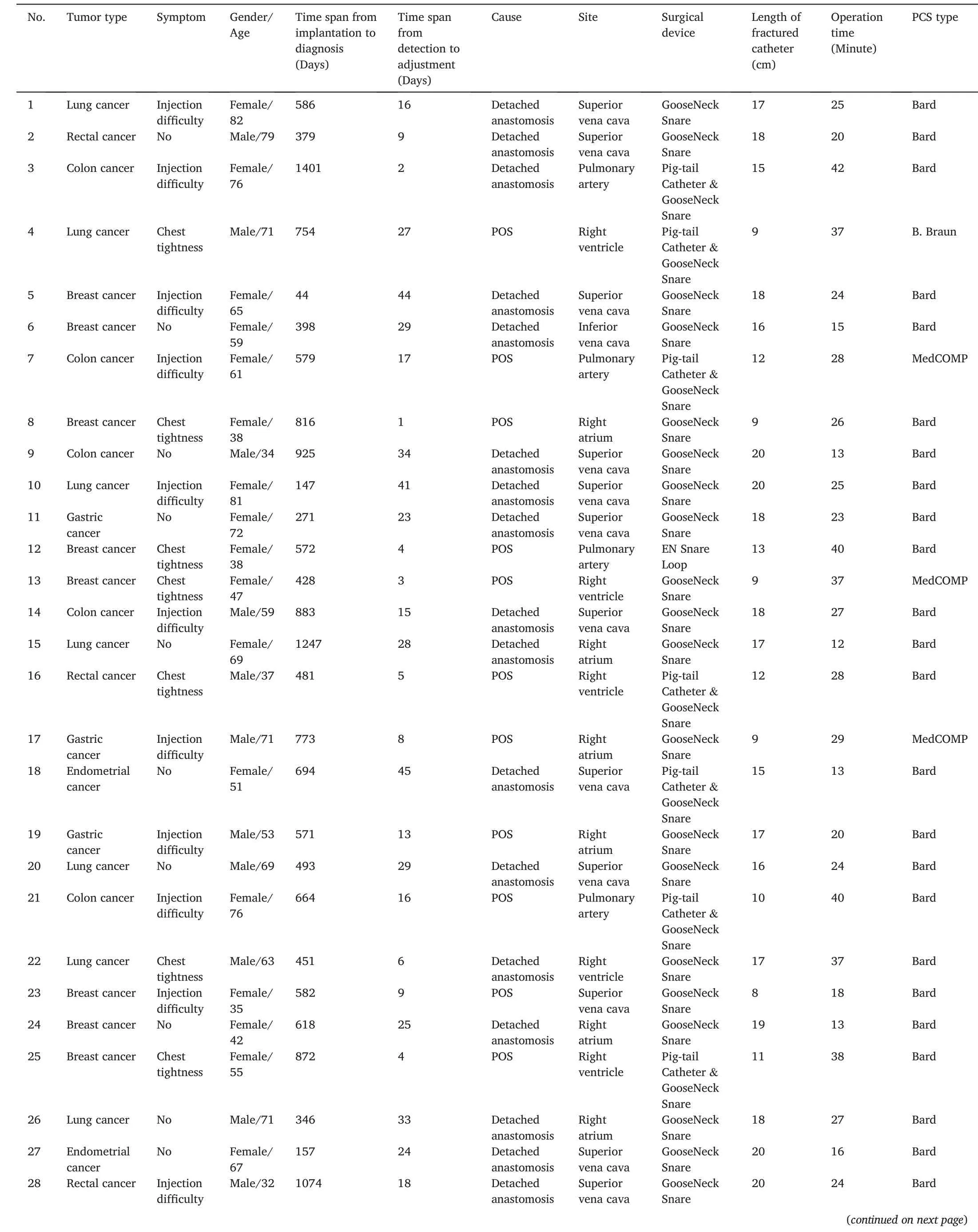
Table 2 Clinical data of patients with catheter fracture.
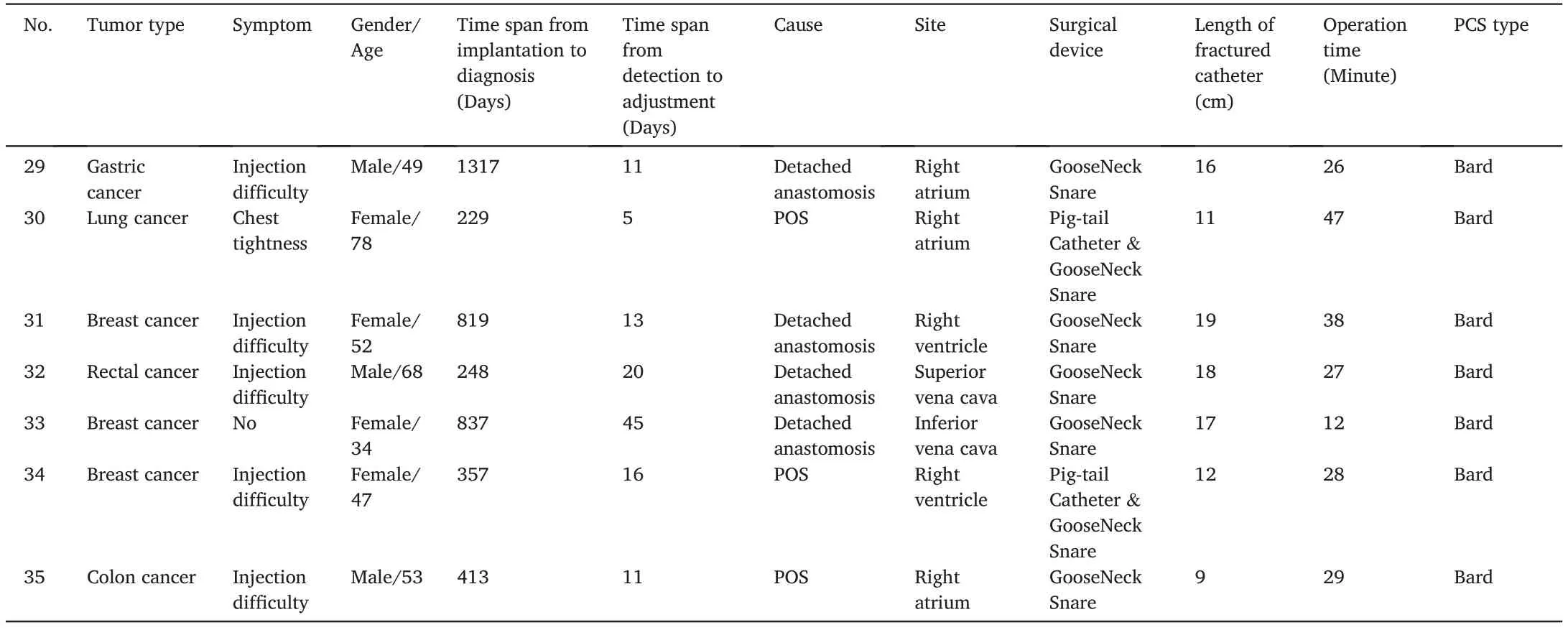
Table 2 (continued)
3. Results
A total of 1716 venous access systems were implanted in the hospital between January 2009 and June 2019. A total of 58 cases of abnormal positioning were detected, consisting of 23 cases of migrated catheters and 35 cases of fractured catheters. Of the 58 cases, 52 patients with abnormally positioned catheters underwent implantation in this hospital,whereas the other 6 underwent the procedure in other hospitals.Therefore,the incidence of abnormal catheter positioning in this hospital was 3.0%(52/1716).The detailed patient data are presented in Tables 1 and 2. The patients were comprised of 25 men and 33 women, and the average age of the patients was 55.59 ± 14.09 years old (range: 31–82 years). The average time from implantation to diagnosis of abnormal positioning was 549.38 ± 312.72 days (range: 10–1401 days), whereas the average time from diagnosis to adjustment or removal was 18.05 ±12.23 days(range:1–45 days).
The 23 cases of migrated catheters were comprised of 5 cases of elastic retraction and 18 cases of tip migration. Among the 18 patients who suffered tip migration, and 2 received implantation in other hospitals;therefore,the incidence of migration in our hospital was 1.2%(21/1716).Of the 5 cases of elastic retraction,routine chest radiography of 1 case showed that the proximal end of the catheter was twisted and the tip was in the upper segment of the superior vena cava.However,as the PCS was functioning effectively, adjustments were not performed for this patient.The other 4 cases of elastic retraction presented with difficulties in injection,and the radiograph showed that the segment of the catheter in the subclavian vein was folded and the tip was located in the subclavian vein.Repositioning was successfully performed in 1 case through a pigtail catheter and in another 2 cases using a gooseneck snare.In the last case,the entire port system was removed percutaneously,and a new PCS was implanted in the contralateral subclavian vein,after relocation using both a pigtail catheter and gooseneck snare failed.Meanwhile,in all 18 patients diagnosed with tip migration, the tips of the catheters were displaced into the internal jugular vein.Clinical manifestations included injection difficulty in 9 cases, dizziness and headache in 2, distending pain in the subclavian region in 1,shoulder and neck discomfort in 1,and no symptoms in 5. All migrated catheters were adjusted intravascularly through percutaneous punctures, and the average operation time was 19.09±9.82 min.Repositioning was successfully performed in 9 patients with only a homemade pigtail catheter (Fig. 1A–F), in 4 patients with only a cobra catheter,and in 5 patients with a gooseneck snare after the use of both pigtail and Cobra catheters failed.Among the 5 patients who underwent repositioning using a gooseneck snare,1 presented with fibrin sheath adhesion between the distal end of the catheter tip and the wall of the internal jugular vein.The distal end of the catheter was not exposed after relocation, and both the pigtail and cobra catheters failed in retrieval. The gooseneck snare initially failed to hook the distal end.Repeated pulling with a pigtail catheter exposed the free end,which was then successfully hooked by the gooseneck snare and repositioned after several attempts. The success rate of percutaneous vascular adjustment was 91.3%(21/23).
The fracture site was the superior vena cava in 13 cases, the right atrium in 9, the right ventricle in 7, the pulmonary artery in 4, and the inferior vena cava in 2. Clinical manifestations included injection difficulty in 16 cases,chest tightness in 8,and no symptoms in 11.Among the 35 patients with catheter fractures, 14 (40%) developed pinch-off syndrome (POS, catheter fracture in the subclavian region caused by continuous pressure from the clavicle and the first rib),whereas the other 21 cases(60%)developed disconnection between the port and catheter.Four of the fracture patients received implantation in other hospitals;therefore, the incidence rate of fractures in our hospital was 1.8% (31/1716). All ruptured catheters were removed by percutaneous puncture with a 100%success rate(35/35).The average operation time was 26.51± 9.46 min. The mean length of the removed catheters was 15 ± 4 cm(range: 8–20 cm). Both the gooseneck snare and pigtail catheter were used in 9 cases,as the pigtail catheter was needed to expose the free end.Meanwhile,in 25 patients,the gooseneck snare was the only device used to remove the fractured catheters (Fig. 2A–C). The distal end of the fractured catheter was near the right atrium wall in 1 patient and the sheath of the gooseneck snare could not reach the proximal end of the free catheter. Therefore, a 6 F JR4.0 angiographic catheter and a 6 F gooseneck snare were used together to hook the free end, enabling successful removal. An EN snare loop (Angiotech Medical Device Technologies,South Jordan,Utah,USA)was used to treat 1 patient.Entry of the external sheath of the loop to the pulmonary trunk was challenging because the fracture was in the middle of the catheter (at the junction between the first rib and the clavicle).The distal end of the catheter was located in the middle branches of the right pulmonary artery, and the proximal end was located in the right main pulmonary artery close to the bifurcation site and attached to the vessel wall.After several unsuccessful attempts, a 6 F JL4.0 guide catheter and an EN snare loop were jointly used,and the fractured catheter was successfully hooked(Fig.3A–E).All PCSs with fractured catheters were removed, and new systems were implanted in the contralateral subclavian region in patients who still needed central venous access.
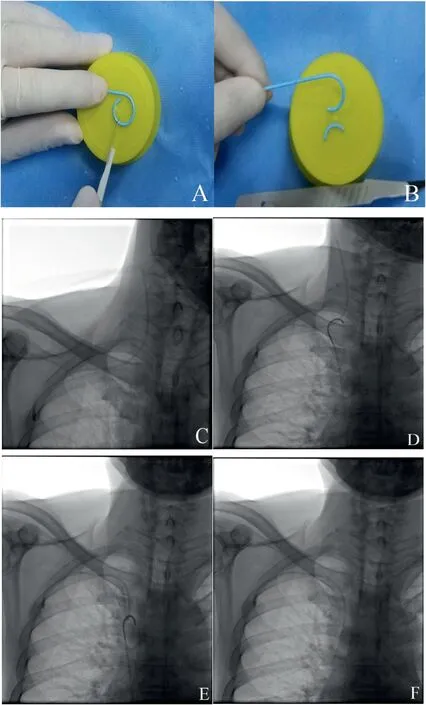
Fig. 1. Surgery procedure for a 61-year-old male patient with rectal cancer, diagnosed with catheter migration 3 months after PCS implantation.
All the patients were treated using the right femoral venous approach.The detailed patient data are presented in Tables 1 and 2.The 23 patients with catheter migration did not present with surgery-related complications. Among the 35 cases of catheter fracture, 3 developed transient atrial arrhythmias or ventricular arrhythmias during surgery; however,the complications were not severe, and there was no need for intervention with drugs. No surgery-related complications were observed either immediately or during the 1-month follow-up period.
4. Discussion
Subcutaneous implantation of a PCS was introduced by Niederhuber6in 1982.Currently,it is widely used in the clinical treatment of patients requiring long-term intravenous infusion. Studies have reported that approximately 5 million PCSs are implanted every year in the United States.7The interventional radiology center of our hospital has implanted 1716 PCSs into subclavian veins since its establishment in 2009. This figure has been increasing yearly.

Fig. 2. Surgery procedure of a 63-year-old male patient with lung cancer, diagnosed with catheter fracture 15 months after PCS implantation.
Spontaneous catheter migration is rare.The incidence rate of catheter migration within the follow-up period of 5–9 months is 0.9%–1.8%.8,9The incidence of catheter migration in the current study was 1.2%(21/1716),which is consistent with the previous findings.The ideal site of the catheter tip is between the lower third of the superior vena cava and the upper third of the right atrium.10The PCS should not be used when the tip becomes displaced to small veins,the brachiocephalic vein,and the subclavian vein,as this increases the risk of venous thrombosis.Additionally,the risk of injection into the veins is high,leading to severe complications.4,11–13Therefore, it is necessary to adjust the position of the catheter or remove the PCS when migration occurs.
A previously reported technique of high-pressure injection of normal saline was initially used in the current hospital to reposition migrated catheters through irrigation.14However, this technique is ineffective,and can lead to rupture and separation of the connection between the port and the catheter.Adjustment with catheters or gooseneck snares is more effective and feasible than reimplantation or replacement of PCS.15Gebauer et al.15reported the use of catheters and a gooseneck snare in adjusting migrated catheters through the femoral vein with a 93% success rate(27/29).In the current study,the success rate of percutaneous vascular adjustment was 91.3%(21/23),which is similar to that reported in previous studies.
The gooseneck snare is used when the free end of the migrated catheter tip is exposed so that it can be hooked and relocated to the superior vena cava,which is similar to the removal of fractured catheters.16Bessoud et al.16reported that the success rates of other surgical tools were very low if the gooseneck snare had failed to adjust the position of the migrated catheter. In 1 patient in this study, the catheter tip was located in the internal jugular vein, and the formation of fibrin sheaths led to a firm attachment of the distal end to the vein. The migrated catheter was successfully hooked using a pigtail catheter. However,pulling multiple times did not change the position of the catheter,which can be attributed to the soft tail end of the guide catheter or endothelialization between the migrated catheter and the vessel wall. Successful adjustment was achieved by hooking the freed end of the tip using a gooseneck snare.
The cause of spontaneous catheter displacement is not fully understood. Potential causes include a short indwelling catheter, vigorous movement and pulling of the shoulders and upper arms,change in chest pressure resulting from severe cough and frequent vomiting, and migration and pulling off the subcutaneous port.3,17,18Therefore, the solution involves minimizing the number of high-risk factors during PCS implantation.
Catheter fracture was initially reported to cause the formation of embolisms in the distal end in 1954,19and several clinical studies reported that the incidence of catheter fracture ranges from 0 to 4.1%,20–23whereas the death rate or rate of severe complications was approximately 71%.24,25Therefore,intervention should be carried out immediately if a fracture occurs,and intravascular removal of fractured catheters through percutaneous puncture is the conventional technique.26The success rate of PCS catheter removal by percutaneous puncture is 90–97.8%.22,27In the current study,the incidence of catheter fracture was 1.8%(31/1716),which is consistent with previous reports.Notably,all fractured catheters were successfully removed through percutaneous punctures, with a 100% success rate (35/35), and no surgery-related complications were observed.
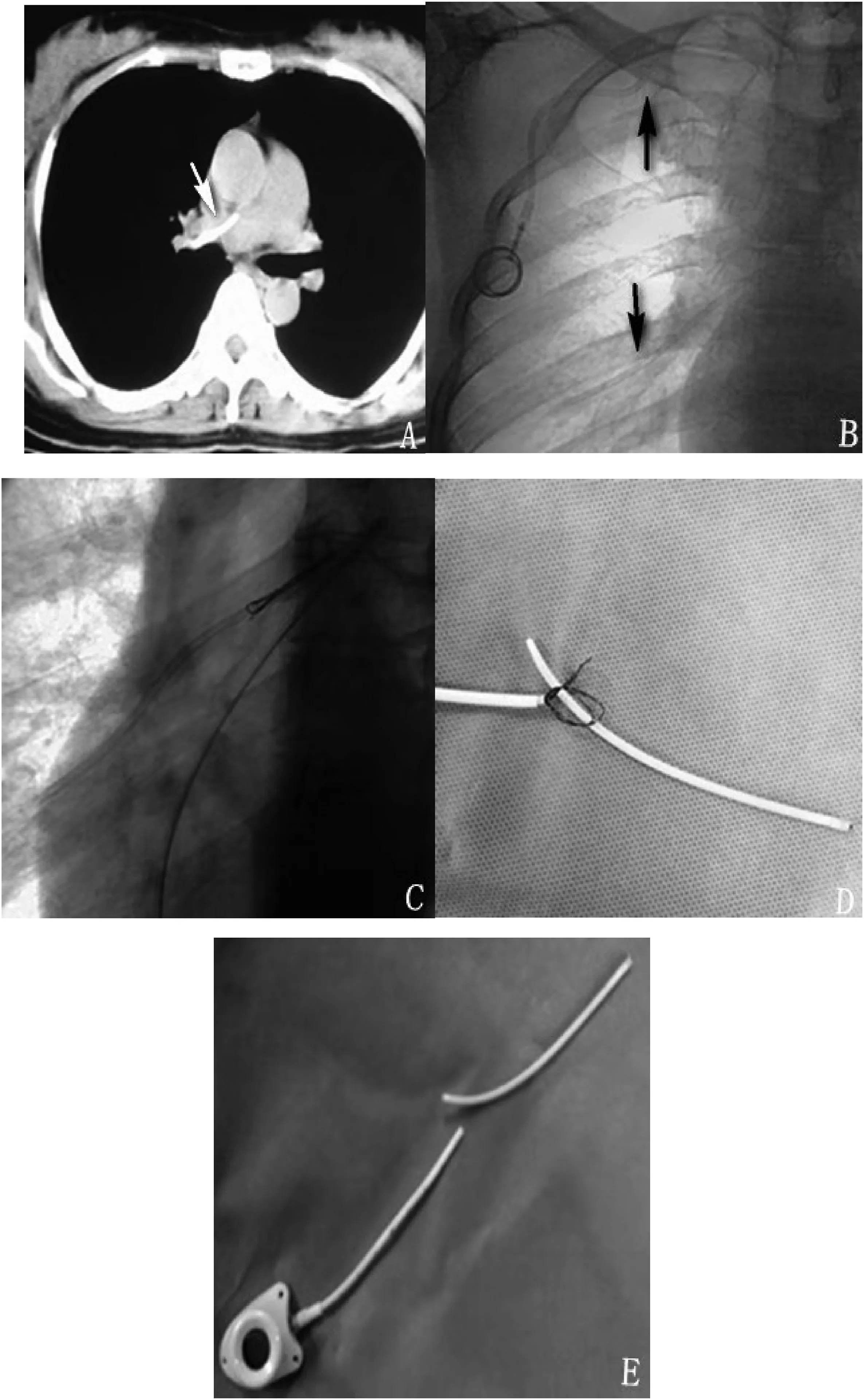
Fig. 3. Surgery procedure for a 38-year-old female patient with breast cancer, diagnosed with catheter fracture 19 months after PCS implantation.
Several interventional devices are currently used for intravascular removal. The most commonly used device in previous studies was the gooseneck snare.16,28In the present study,removal of fractured catheters was performed in 25 patients using the gooseneck snare, while the EN snare loop was used in only 1 patient.There was at least 1 free end in 26 patients, which made it easier for the 2 devices to hook the fractured catheter. Nine patients presented with fractured catheters that did not have free ends or the free ends were not exposed. In these cases, the gooseneck snare alone failed to hook the free ends of the fractured catheter;therefore,a pigtail catheter and a gooseneck snare were jointly used.The tail of the pigtail catheter was first used to hook the fractured catheter and expose the free ends by pulling them, and then the gooseneck snare was used to successfully hook the free ends. During the removal of the fractured catheters in 2 cases, it was observed that the fixed angle made hooking of the free ends challenging owing to the rigid external sheath of the snare. The external casing is replaced by an angiographic or guiding catheter with a stable angle,and the catheter is continuously checked to successfully remove the broken catheter.
The position of fractured foreign bodies in the cardiovascular system depends on gravity, their entry path, length, stiffness, and blood flow pattern in the blood vessels and heart cavities.22,28,29Bessoud et al.16reported that the most common site of embolisms was the pulmonary artery. Cheng et al.22reported that most embolisms were located between the inferior vena cava and the right atrium or between the right atrium and the superior vena cava,which is consistent with the findings of Koseoglu et al.30and Liu et al.28In the current study,the most common location of fractured catheters was at the junction of the superior vena cava and the right atrium.
Possible causes of catheter fracture include the use of improper equipment leading to damage to the catheter, use of small syringes leading to increased pressure inside the catheter,continuous pressure on the catheter between the clavicle and the first rib (POS), improper connection between the port and the catheter,deformity of the connection between the port and the catheter,and improper positioning of the catheter.22,23,28In the current study,there were 14 cases of POS(14/35,40%) and 21 cases of detachment of the proximal end from the port(21/35, 60%). Among the 35 patients with catheter fractures, 31 were implanted in our hospital, including 27 patients for whom the Bard Access System(27/1401,1.9%)(BD,Franklin Lakes,NJ,USA)was used,1 patient for whom the B. Braun Access System(B. Braun Medical Inc.,Bethlehem,PA,USA)was used(1/63,1.6%),and 3 patients for whom the MedCOMP Access System(Medical Components,Inc.,Harleysville,PA,USA)(3/252,1.2%)was used.Lin et al.31reported that the risk of fracture may be related to POS and PCS design. Shoulder movement exerts a pulling force on the catheter(“pinching”the catheter),leading to continuous pulling or compression of the connection between the catheter and the port,resulting in pressure on the catheter or fracture of the segment being pulled.31Liu et al.28reported that the subclavian vein should be punctured at the junction of the middle and outer thirds of the clavicle to avoid POS.Furthermore,the port and the catheter should be firmly connected to avoid an angle between the 2 PCS parts or deformation of their connection. Moreover, follow-up chest radiography should be performed routinely and over a long follow-up period,and the system should be removed immediately if it1is no longer in use.
5. Conclusions
The incidence of abnormal catheter positioning is low. Once an abnormality is detected, the use of the system should be stopped immediately, and adjustment or removal should be performed with effective methods. Intravascular techniques for catheter adjustment or removal are safe, efficient,and minimally invasive.
Author statement
Yong Li: Conceptualization, Methodology, Software, Data curation,Writing- Original draft preparation, Visualization, Investigation. Jianxi Guo:Conceptualization,Methodology,Software,Data curation,Writing-Original draft preparation, Visualization, Investigation, Writing-Reviewing and Editing. Yanfang Zhang: Validation, Writing- Reviewing and Editing.Jian Kong:Conceptualization,Methodology,Data curation,Writing- Original draft preparation, Visualization, Investigation, Supervision, Validation,Writing-Reviewing and Editing.
Conflicts of interest and source of funding
There are no conflicts of interest.It has received honoraria from Key-Area Research and Development Program of Guangdong Province,China(2020B010165004).
Appendix A. Supplementary data
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jimed.2022.03.003.
 Journal of Interventional Medicine2022年2期
Journal of Interventional Medicine2022年2期
- Journal of Interventional Medicine的其它文章
- Advances in the interventional therapy of hepatocellular carcinoma originating from the caudate lobe
- The underlying molecular mechanism of intratumoral radiofrequency hyperthermia-enhanced chemotherapy of pancreatic cancer
- The apoptotic effect of ozone therapy on mitochondrial activity of highly metastatic breast cancer cell line MDA-MB-231 using in vitro approaches
- Preparation and investigation of a novel iodine-based visible polyvinyl alcohol embolization material
- Intrahepatic flow diversion prior to segmental Yttrium-90 radioembolization for challenging tumor vasculature
- Safety and efficacy of transcatheter arterial embolization for management of refractory hematuria of prostatic origin
